Abstract
Despite the continued release of new devices, from lasers to ultrasound, chemical peels remain our steadfast resurfacing tool. This is due in large part to their proven efficacy and safety. This chapter reviews the science of chemexfoliation, the tools most commonly used, the technique, and the expected results; avoidance and treatment of complications are also discussed. In addition, mechanical resurfacing procedures, including motorized dermabrasion, manual dermasanding and microdermabrasion, are outlined. Of note, the early recognition of delayed or aberrant wound healing, followed by appropriate treatment, is a necessary component of the practice of chemical peeling and dermabrasion.
Keywords
chemical peeling, chemical resurfacing, chemexfoliation, superficial peel, medium-depth peel, deep peel, TCA CROSS, glycolic acid, salicylic acid, phenol, Jessner’s solution, Baker–Gordon peel, microdermabrasion, manual dermasanding, dermabrasion
▪ Chemical resurfacing: chemical peeling, chemexfoliation ▪ Mechanical resurfacing: dermabrasion (includes dermasanding) ▪ Cosmeceutical: topical agent possessing pharmacologic and physiologic effects but promoted to a variable degree as a cosmetic ▪ Jessner’s peel: Combes’ peel ▪ Baker–Gordon peel: deep phenol peel
- ▪
Chemical peeling, dermabrasion, and laser ablation are the three main methods of skin resurfacing
- ▪
Chemical and mechanical resurfacing procedures have a long history of safety and efficacy in ameliorating various skin conditions and improving cutaneous photoaging
- ▪
Resurfacing procedures represent one part of a comprehensive skin care program that should include photoprotective measures and topical medical and/or cosmeceutical agents
- ▪
Each resurfacing procedure injures the skin to a specific depth in order to promote the regrowth of new skin with improved surface characteristics
- ▪
The degree of clinical improvement, the length of the recovery period, and the risk of complications are all proportionate to the depth of tissue injury chosen and skin type
- ▪
Selection of suitable patients and proper choice of resurfacing procedure are critical to success
- ▪
Both dermabrasion and the “TCA CROSS” technique are methods for treating acne scars
- ▪
Prolonged erythema, pigmentary or textural irregularities, infection, delayed healing, and scarring are potential complications of resurfacing
- ▪
Resurfacing procedures are a rewarding part of dermatologic practice, both for the patient and for the physician
Introduction and History
Resurfacing procedures to improve the health and appearance of the skin have been utilized by humans for thousands of years. The ancient Egyptians applied various chemicals to the skin and may have even used abrasives like sandpaper in order to obtain a smoother skin surface . Resurfacing methods within the practice of dermatology were initially described over 100 years ago. Early on, chemical cauterants were used primarily for proliferative lesions and skin disorders, with pioneers such as Hebra and Jessner discovering the usefulness of acidic and basic compounds for skin exfoliation. Over the past several decades, the role of chemoexfoliation has expanded dramatically to include textural and cosmetic revisions. Our society’s increasing emphasis on a youthful image and aesthetic appearance has resulted in an explosion in public demand for commercial skin care products, professional assistance from physicians and non-physicians to assure proper medical and cosmeceutical skin therapy, and procedural intervention by physicians.
All ablative resurfacing procedures injure the skin, in a controlled fashion, to a specific depth and thereby promote the growth of new skin with improved surface characteristics. The three fundamental methods used to create this controlled injury are chemical resurfacing (chemical peeling), mechanical resurfacing (motorized dermabrasion or manual dermasanding), and laser resurfacing (see Ch. 137 ). Chemical resurfacing entails the application of acidic or basic abrasive chemical substances that can destroy selective levels of the epidermis or dermis. Mechanical resurfacing involves skin contact with an abrasive surface which physically removes portions of the epidermis and dermis.
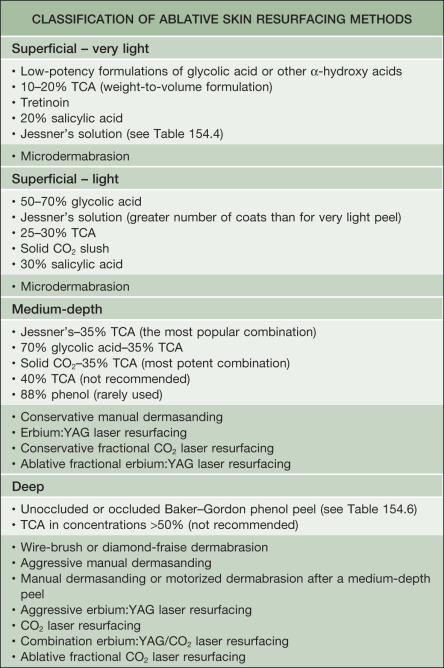
In general, skin resurfacing procedures can be classified as superficial, medium-depth or deep, according to their level of injury ( Table 154.1 ). Skin resurfacing is usually performed only on the head and neck, in part because of the critical aesthetic value of this area. Caution must be exercised in treating the neck, due to its propensity for complications; only superficial procedures should be performed on the lower one-third of the neck and other non-facial areas. Resurfacing of other areas, including the hands and arms, has yielded less predictable and less impressive results as well as a higher risk for scarring.
In comparison to the other resurfacing modalities available for skin rejuvenation, chemical resurfacing probably has the longest and most well-documented history . Experimentation with various peeling compounds in the late nineteenth and early twentieth centuries led to sporadic reports describing their use in the medical literature. The initial reports were met with skepticism, but further investigation by both dermatologists and plastic surgeons verified their effectiveness in facial skin rejuvenation and as a treatment for skin disorders. Over the past several decades, chemical peeling has experienced a tremendous growth in popularity and has become an important part of our armamentarium in the management of various cosmetic as well as non-cosmetic skin problems. Currently, chemical peeling is the third most commonly employed cosmetic procedure, after injectable neurotoxins and soft tissue fillers.
Since Kromayer’s original report of motorized dermabrasion in 1905, there has been considerable growth not only in chemical resurfacing procedures, but also in mechanical resurfacing. Mechanical resurfacing is most often known as dermabrasion but it refers to any procedure that involves surgical planing of the skin using an abrasive surface. The use of dermabrasion was originally limited to the treatment of scars, but its role expanded during the latter half of the twentieth century to include a multitude of indications . Recent adaptations of the traditional techniques of dermabrasion have led to the development of a less invasive procedure, known as microdermabrasion . Dermasanding, which is a manual technique of dermabrasion utilizing abrasive paper, has been in use for centuries, but recently has experienced a resurgence . Although overshadowed by ablative and non-ablative laser resurfacing (see Ch. 137 ), mechanical resurfacing procedures remain a popular option for both patients and physicians.
Preoperative History and Considerations
Indications
The preoperative consultation is important in identifying at-risk patients who are best avoided or who require an extra-cautious approach, as well as in selecting patients who are ideal candidates for intervention. The dermatologist must evaluate the prospective patient and his or her skin condition carefully, in order to determine if a chemical or mechanical resurfacing procedure is indicated. When resurfacing is deemed appropriate, selection of the proper procedure for each patient is critical to assure that the desired results are achieved in a safe and effective manner. In general, the degree of skin surface irregularities is proportional to the depth of the injury that must be created by resurfacing in order to achieve significant improvement. There are six major indications for resurfacing ( Table 154.2 ).
| MAJOR INDICATIONS FOR CHEMICAL AND MECHANICAL SKIN RESURFACING |
|
Pre-neoplastic or neoplastic skin lesions can certainly be improved with resurfacing procedures. Those originating in the epidermis, such as actinic keratoses or lentigines, are more amenable to treatment than those with a dermal extension or origin. Although some dermatologic conditions may be aggravated by resurfacing, acne and pigmentary dyschromias such as melasma respond favorably to superficial chemical peeling or microdermabrasion, especially when accompanied by appropriate cosmeceutical products and sunscreens. Another indication for chemical and mechanical skin resurfacing is to blend the effects of other procedures by preventing or eliminating lines of demarcation.
Photoaging is probably the single condition for which skin resurfacing procedures are most often performed. For patients with photoaging, the Glogau system (see Ch. 152 ) is helpful in deciding upon the most appropriate skin rejuvenation program. It classifies patients into one of four groups based on degree of severity. Patients in category I are often young with minimal to mild photoaging and are best managed with superficial chemical peels or microdermabrasion in conjunction with topical medications or cosmeceuticals (e.g. retinoids, glycolic acids, antioxidants, vitamin C, vitamin E). Patients in category II would likely benefit from a medium-depth chemical peel as well as long-term medical therapy to include a retinoid and/or an α-hydroxy acid (AHA). Individuals in category III typically need prolonged medical treatment in conjunction with one of the following: a medium-depth chemical peel (with or without dermasanding), a deep chemical peel, dermabrasion, or laser resurfacing. For patients with category IV photoaging, interventions utilized for category III individuals are also recommended, but the addition of an invasive surgical operation such as a rhytidectomy or blepharoplasty is often required in order to achieve the desired results. Nowadays, reconstruction of facial form and correction of deep furrows with injectable neurotoxins and soft tissue fillers is such that resurfacing techniques represent a final stage in the combination approach to facial rejuvenation (see Chs 158 & 159).
Contraindications and Patient Selection
When evaluating a patient for chemical or mechanical resurfacing, a careful history and physical examination are important to assess the skin problems which prompted his or her presentation and to identify any factors that may contribute to intraoperative or postoperative difficulties ( Table 154.3 ). The patient should be asked about prior resurfacing procedures, rhytidectomy (facelift), or oral isotretinoin therapy within the last 6 months, as these can increase the risk of complications following medium-depth and deep resurfacing . Any history of abnormal scar formation or therapeutic radiation exposure warrants extreme caution when considering a patient for skin resurfacing. Individuals with prior radiation exposure should be examined closely for the presence of intact facial hair in order to ensure that there are enough pilosebaceous units to promote re-epithelialization . Another important element of the patient’s history is the presence or absence of a prior herpes simplex viral (HSV) infection. Recurrence of oral HSV can be triggered by a resurfacing procedure, especially in the perioral and periorbital regions. Risk factors for HIV infection or viral hepatitis should be identified, and routine laboratory screening is recommended in individuals undergoing dermabrasion with a powered engine. A history of abnormal wound healing from trauma or previous procedures, e.g. hypertrophic scarring, dyschromia, may be a contraindication to peeling or dermabrasion. The general health and nutritional status of the patient is also an important consideration, especially for medium-depth and deep resurfacing procedures, to ensure timely and complete healing.
| CONTRAINDICATIONS TO CHEMICAL AND MECHANICAL SKIN RESURFACING |
| Absolute |
|
| Relative |
|
* These contraindications apply only to medium-depth and deep resurfacing procedures.
Patients with certain cutaneous disorders, such as rosacea, seborrheic dermatitis, atopic dermatitis, psoriasis or vitiligo, may be at increased risk for postoperative complications, including disease exacerbation, prolonged erythema, contact dermatitis, or even delayed healing. In particular, individuals with rosacea have vasomotor instability and may develop an exaggerated inflammatory response to the resurfacing procedure. Caution should also be exercised for patients with autoimmune connective tissue diseases (e.g. cutaneous lupus, systemic sclerosis) as the trauma of chemical peeling may exacerbate the disease. Evaluation of the patient’s Fitzpatrick skin type (see Ch. 0 ) is helpful in predicting the chance of postoperative pigmentary dyschromias. Individuals with Fitzpatrick skin types I or II are at low risk for hyperpigmentation or hypopigmentation after medium-depth or deep resurfacing, whereas those with types III through VI are at greater risk for these complications .
The patient should understand that chemical and mechanical resurfacing procedures cannot reliably reduce pore size, and their ability to improve lax skin or deeper wrinkles and scars is limited and depends upon the type of intervention being performed. While dermabrasion may sometimes eliminate telangiectasias, chemical peels cannot accomplish this and can even unmask them by removing the pigmentary irregularities. The patient must fully understand the potential benefits, limitations and risks of the procedure, and an informed consent must be signed.
A test spot (e.g. along the lateral hair line) may be useful in some patients to assess their suitability for resurfacing and may be particularly helpful when there is a great deal of concern about the chances of postoperative pigmentary dyschromias ; test spots are definitely recommended for individuals with skin types III–VI. Of note, while a favorable test spot result does not guarantee a positive outcome following full-face resurfacing, an unfavorable test spot result is useful in identifying high-risk patients. The latter include those at risk for postinflammatory hyperpigmentation, spotting, irregular coloration, or hypopigmentation. If the dermatologist feels any uncertainty about the patient’s suitability or the likelihood of a favorable result, the procedure should not be performed.
Preoperative and Intraoperative Preparations
Another purpose of the preoperative consultation is to ensure that the patient is adequately prepared for the procedure. Almost every patient desiring facial rejuvenation for cutaneous photoaging would benefit from botulinum toxin injections to alleviate dynamic wrinkles (see Ch. 159 ). These injections appear to enhance the results of deeper resurfacing procedures by immobilizing the muscles implicated in the development of dynamic rhytides during the critical time of postoperative collagen remodeling. In patients with photoaging, it is recommended that botulinum toxin injections be administered as an adjunctive therapy at least 3 days prior to medium-depth or deep chemical peels, dermabrasion, or laser resurfacing.
Due to the significant morbidity associated with herpetic infections during the healing period, patients who undergo medium-depth or deep resurfacing (see Table 154.1 ) should be treated prophylactically with an antiviral agent, regardless of whether there is a history of HSV infections . These drugs are not routinely given to patients having a superficial chemical peel or microdermabrasion, because the injury is generally not sufficient to activate the virus. However, therapy may be considered in conjunction with superficial resurfacing in patients with a strong personal history of recurrent HSV infection. Recommended prophylaxis consists of acyclovir 400 mg three times daily, valacyclovir 500 mg twice daily or famciclovir 250 mg twice daily, beginning on the day of the procedure. It is advisable to administer the drug for at least 10 to 14 days thereafter . The reason for such a long duration of therapy is that viral replication is possible only in intact epidermal cells, making clinical infection unlikely during the first few days postoperatively. The risk of an eruption increases dramatically with the onset of re-epithelialization and remains high until this process is complete.
It is important that the patient adhere to a strict skin care regimen during the immediate preoperative and postoperative periods in order to achieve optimal results. The authors treat patients with topical tretinoin on a nightly basis prior to the procedure. Retinoids increase epidermal proliferation and presumably lead to more rapid re-epithelialization after the chemical peel. Because of the tendency for retinoids to cause irritation within 1 to 2 weeks of starting therapy (i.e. retinoid dermatitis), a weaker, more gentle tretinoin formulation should be used in patients with sensitive skin. In patients with active retinoid dermatitis, resurfacing should be delayed, because this condition may lead to a prolongation in postoperative erythema. Decreasing the frequency of application or switching to a less irritating retinoid will allow the inflammation to subside, so that the procedure can be performed .
All- trans -retinoic acid, or tretinoin, has been classified as a superficial chemical peeling agent, but it is best considered as an integral component of a complete skin rejuvenation program. With chronic use, this drug has been shown to improve actinically damaged skin both clinically and histologically . The use of tretinoin prior to chemical peeling, dermabrasion or laser resurfacing speeds epidermal healing and enhances the effects of the procedure . For chemical peels in particular, use of preoperative topical tretinoin to reduce areas of hyperkeratosis and decrease the thickness of the stratum corneum allows for greater penetration of the peel solution, resulting in a more homogeneous peel and a deeper peel. Use of tretinoin is restricted, however, during the postoperative healing period, until there is complete re-epithelialization and diminished inflammatory erythema.
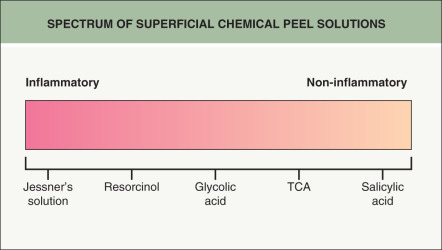
Hydroquinone blocks the enzyme tyrosinase and can reduce the production of epidermal melanin during the healing phase. Patients with skin type III or higher may benefit from twice-daily application of 2% to 4% topical hydroquinone during the preoperative and postoperative (post-healing) periods – even if there is no history of pigmentary abnormalities . It is also necessary to use hydroquinone in patients of any skin type when peeling is done to treat pigmentary dyschromias such as melasma or postinflammatory hyperpigmentation . While a Wood’s lamp was used in the past to localize melanin pigment to either the epidermis or dermis (i.e. epidermal versus dermal melasma), histopathologic studies and confocal microscopy have shown that there is often a mixture of the two forms in an individual patient. Nonetheless, in both melasma and postinflammatory hyperpigmentation, increased melanin within the epidermis responds better to superficial peels than does dermal pigment. The use of non-inflammatory peeling agents, e.g. salicylic acid, is preferred for disorders such as melasma as there is less tendency for postinflammatory hyperpigmentation ( Fig. 154.1 ).
All patients undergoing any type of skin resurfacing procedure must adhere to strict photoprotective measures during the postoperative period. This issue is critical in patients whose Fitzpatrick skin type is III or higher, in patients with pigmentary abnormalities, in patients taking exogenous estrogens, and in all patients having medium-depth or deep resurfacing. Specific methods to minimize sun exposure and proper use of sun blocks should be discussed. Patients are also counseled to avoid tobacco use, as smoking in the postoperative period may interfere with the healing process, thereby limiting the effectiveness of the resurfacing and increasing the risk of poor wound healing.
The need for intraoperative sedation and analgesia is also discussed with the patient preoperatively, so that plans are made accordingly. Superficial resurfacing procedures usually require only “talkesthesia”, a technique that is extremely helpful in awake patients undergoing a procedure, i.e. talking calmly to the patient with encouragement during the procedure. Medium-depth chemical or mechanical resurfacing usually requires a limited degree of perioperative sedation and analgesia, which may include the application of topical amide anesthetics and regional blocks of the supraorbital, infraorbital and mental nerves (see Ch. 143 ), as well as oral diazepam, intramuscular meperidine hydrochloride, and/or intramuscular hydroxyzine hydrochloride. Although deep resurfacing procedures can be accomplished entirely with nerve blockade, local injections of lidocaine, and mild sedatives, some patients require intravenous or general (endotracheal tube) anesthesia. Application of the tumescent technique (see Ch. 156 ) to resurfacing has allowed many patients to undergo deep resurfacing procedures without the additional risks of intravenous or general anesthesia . The patient’s inherent pain tolerance, level of anxiety, concomitant medical conditions, and willingness to pay the extra costs of heavier sedation are important topics to discuss during the preoperative consultation that is used to plan for appropriate anesthesia.
Preoperatively, the patient must be given specific instructions to follow, both for the day of the procedure and for postoperative care. These should be carefully reviewed verbally prior to the procedure, with the same instructions provided in written form. On the day of the procedure, the patient washes his or her face with a gentle cleanser and preferably avoids the application of any cosmetics. Individuals undergoing procedures requiring minimal or no sedation are encouraged to eat a light breakfast, but patients receiving deeper anesthesia should have nothing by mouth except for their usual medications. Particularly for the medium-depth and deep resurfacing procedures, the dermatologist should meet with the patient and his or her family preoperatively to re-establish rapport, answer last-minute questions, discuss perioperative and postoperative expectations and instructions, and assure compliance with antiviral prophylaxis as needed.
Chemical Resurfacing Procedures
Although there is currently a wide variety of resurfacing procedures available for facial rejuvenation, chemical peeling remains a popular choice for both patient and physician. In comparison to some of the newer options, chemical peels have a longstanding safety and efficacy record, are performed with ease, are low in cost, and have a predictable and relatively quick recovery time. Various acidic and basic compounds are used to produce a controlled skin injury and are classified as superficial, medium-depth, and deep peeling agents, according to their level of penetration, destruction, and inflammation (see Table 154.1 ). In general, superficial peels cause epidermal injury and occasionally extend into the papillary dermis, medium-depth peels cause injury through the papillary dermis to the upper reticular dermis, and deep peels cause injury to the mid-reticular dermis.
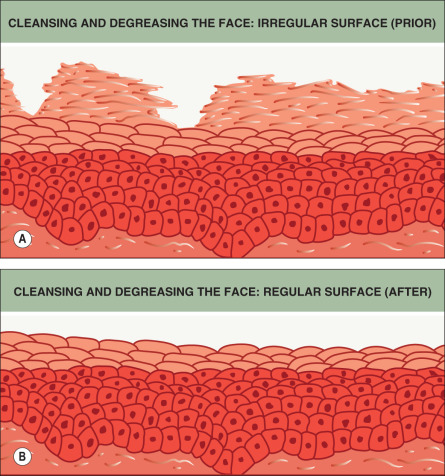
Prior to the application of peeling solutions, the skin surface must be vigorously cleansed to remove residual oils, debris, and excess stratum corneum. The authors use gauze pads containing 0.25% triclosan (an ingredient found in some deodorant soaps), followed by rinsing with water and drying. Because of the defatting and degreasing properties of acetone, gauze pads moistened with an acetone preparation are then used to cleanse the skin even further. Finally, the cleansed skin is palpated immediately prior to peeling, in order to check for the presence of residual oil, and if any is felt, the process is repeated. The importance of cleansing prior to the peeling procedure cannot be overemphasized. A thorough and evenly distributed cleansing and degreasing of the face assures uniform penetration of the peeling solution and leads to an even result without skipping areas ( Fig. 154.2 ).
The effect of a chemical peel is dependent upon the agent used, its concentration, and the techniques employed before and during its application. Each wounding agent used in peels has unique chemical properties and causes a specific pattern of injury to the skin . It is important for the physician using these solutions to be familiar with their cutaneous effects and proper methods of application, to assure correct depth of injury. The marketplace has been flooded with numerous proprietary formulations of these peeling agents, with each product claiming unique advantages. These products are often expensive and have not been shown to be safer or more effective than the conventional solutions. Their advantage rests in the prepackaging of materials and ease for the physician. The following discussion on superficial, medium-depth, and deep peeling will therefore focus on the specific chemical agents that are responsible for producing the various patterns of injury.
Superficial Chemical Peeling
Superficial chemical peels are indicated in the management of acne and its postinflammatory erythema, mild photoaging (Glogau I and II), and epidermal lesions such as lentigines and keratoses, as well as melasma and other pigmentary dyschromias . A series of peels is usually necessary to obtain optimal results . The frequency of peels and degree of exposure to the peeling agent may be increased gradually as necessary. Results are enhanced by medical or cosmeceutical therapy, including a retinoid, antioxidants and, if necessary, a bleaching agent. All superficial chemical peels share the advantages of only mild stinging and burning during application as well as minimal time (a few days) needed for recovery.
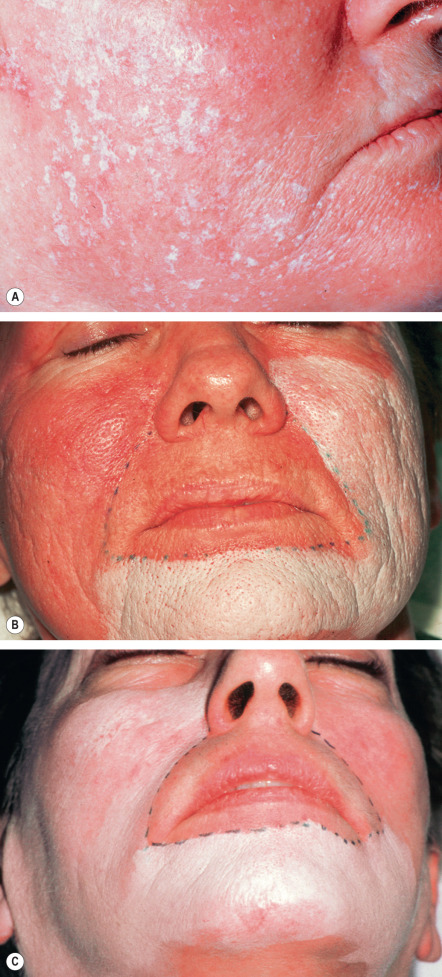
Superficial chemical peels are divided into two varieties – very light and light (see Table 154.1 ). With very light peels, the injury is usually limited to the stratum corneum and only creates exfoliation; however, the injury may extend into the stratum granulosum. The agents used for these peels include low-potency formulations of glycolic acid, 10–20% trichloroacetic acid (TCA), tretinoin, 20% salicylic acid, and Jessner’s solution ( Table 154.4 ) . Light peels injure the entire epidermis down to the basal layer, stimulating the regeneration of a fresh new epithelium. Agents used for light peels include 50–70% glycolic acid, 25–30% TCA, Jessner’s solution (greater number of coats than for very light peels), 30% salicylic acid, and solid CO 2 slush . During the application of superficial peeling agents, there may be mild stinging followed by a level I frosting, defined as the appearance of erythema and streaky whitening on the surface ( Fig. 154.3 ).
| JESSNER’S SOLUTION (COMBES’ FORMULA) | |
|---|---|
| Resorcinol | 14 g |
| Salicylic acid | 14 g |
| 85% lactic acid | 14 g |
| 95% ethanol (q.s.ad) | 100 ml |
Alpha-hydroxy acids (AHAs) are naturally found in foods and have been used widely in skin rejuvenation regimens since the early 1990s. The depth of injury is determined by the specific AHA used, its pH, the concentration of free acid, the volume applied to the skin, and the duration of contact. In low concentrations, AHAs have been shown to decrease the cohesion of corneocytes at the junction of the stratum corneum and the stratum granulosum . Higher concentrations are associated with complete epidermolysis. With chronic use of AHA-containing products on a daily basis, there is an increase in skin thickness, acid mucopolysaccharides and the density of collagen, as well as an improvement in elastic fiber quality . The most popular of the AHAs, glycolic acid , is available in a variety of over-the-counter preparations and can be purchased by physicians in buffered as well as unbuffered concentrations as high as 70% for chemical peels. Weekly or biweekly applications of 40–70% glycolic acid (with cotton swabs, a sable brush, or 2-inch × 2-inch gauze pads) have been used most often for acne, mild photoaging, and melasma . The time of application is critical for glycolic acid, as it must be rinsed off with water or neutralized with 5% sodium bicarbonate after 2 to 4 minutes. It is the only peeling agent that is time-dependent, requiring neutralization to end its action.
Application of 10–20% TCA with either a saturated gauze pad or sable brush produces erythema and a very light frost within 15 to 45 seconds. The depth of penetration of the peeling solution is related to the number of coats applied. Epidermal protein denaturization results in exfoliation without vesiculation. Concentrations of TCA up to 25% can also be used alone as a superficial peeling agent, but may create an injury and inflammation that extends partially into the upper dermis. Jessner’s solution is a combination of keratolytic ingredients that has been used for over 100 years in the treatment of inflammatory and comedonal acne as well as hyperkeratotic skin disorders (see Table 154.4 ). Jessner’s solution has intense keratolytic activity, initially causing loss of corneocyte cohesion within the stratum corneum and subsequently creating intercellular and intracellular edema within the upper epidermis if application is continued . The mode of application for the Jessner’s peel is similar to that of the 10–20% TCA peel. The clinical endpoint of treatment is erythema with blotchy frosting (when used prior to application of TCA in medium-depth peels) or a more uniform frosting (when used alone for superficial peels). While Jessner’s peel can be used in extrafacial sites, care must be taken to restrict the total amount of peel solution, as salicylic acid is absorbed systemically.
Salicylic acid , also referred to as a β-hydroxy acid, is one of the ingredients in Jessner’s solution. It can be used alone for superficial chemical peeling and is a preferred therapy for comedonal acne and inflammatory rosacea as it is lipophilic and concentrates within the pilosebaceous apparatus ( Fig. 154.4 ) . Salicylic acid is quite effective as an adjunctive therapy for both open and closed comedones and for resolving post-acne erythema. As noted previously, salicylic acid produces less inflammation than other superficial peeling agents (see Fig. 154.1 ) and therefore is associated with a lower risk of postinflammatory hyperpigmentation. As a result, it is the preferred peeling agent for removing the excess pigmentation in melasma and postinflammatory hyperpigmentation. Salicyclic acid is more effective in reducing epidermal pigment, especially when combined with a bleaching agent (e.g. hydroquinone) and sunscreens.

Prior to the initial treatment, the patient must understand that the net effect of repetitive superficial chemical peels never approaches the beneficial effect obtained with a single medium-depth or deep peel. The improvements in cutaneous photoaging following superficial peels are usually subtle because there is little to no effect on the dermis. These peels thus cannot produce an appreciable effect on textural changes such as deep wrinkles and furrows which originate within the dermis. Nonetheless, their ease of use and minimal downtime makes these “lunchtime” peels rewarding for patients with realistic expectations and are a favorite of busy patients. Superficial peels are best employed in combination with cosmeceutical agents and other minimal- to no-downtime procedures such as botulinum toxin A injections and intense pulsed light treatments. Desired and expected results include a “brightened” skin appearance with a more uniform color and texture.
Medium-Depth Chemical Peeling
Medium-depth chemical peels consist of controlled damage through the epidermis and papillary dermis, with variable extension to the upper reticular dermis. Both medium-depth and deep chemical peels produce epidermal necrosis plus papillary dermal edema and homogenization with a sparse lymphocytic infiltrate within the first several days . Postoperatively, over a period of 3 months, there is increased collagen production with expansion of the papillary dermis and the development of a mid-dermal band of thicker collagen fibers. These changes correlate with continued clinical improvement in texture, fine lines, and color.
For many years, 40–50% TCA was the prototypical medium-depth peeling agent because of its ability to ameliorate fine wrinkles, actinic changes, and “pre-neoplasias”. TCA as a single agent for medium-depth peeling has fallen out of favor because of the high risk of complications, especially scarring and pigmentary alterations, when used in strengths approaching 50% and higher . Today, most medium-depth chemical peels are performed utilizing 35% TCA in combination with Jessner’s solution, 70% glycolic acid, or solid CO 2 as the “priming” agent. These combination peels have been found to be as effective as 50% TCA alone, but safer with fewer risks . The level of penetration is better controlled with these combination peels, thereby preventing the “hot spots” seen with higher concentrations of TCA that can produce dyschromia and scarring.
Brody and Hailey developed the use of solid CO 2 to freeze the skin prior to the application of 35% TCA. This causes epidermal necrosis and significant dermal edema, thereby allowing deeper penetration of the TCA in selected areas. This technique is particularly useful for effacing the edges of mild acne scars and destroying thicker epidermal growths. Monheit then described a combination medium-depth peel in which Jessner’s solution is first applied, followed by 35% TCA. Similarly, Coleman and Futrell have demonstrated the usefulness of 70% glycolic acid prior to the application of 35% TCA for medium-depth peeling. Jessner’s solution and glycolic acid both appear to effectively weaken the epidermal barrier and allow deeper, more uniform and more controlled penetration of 35% TCA.
Current indications for medium-depth chemical peeling include Glogau group II cutaneous photoaging, epidermal lesions such as actinic keratoses, pigmentary dyschromias, and mild acne scarring, as well as blending of the effects of deeper resurfacing procedures. The most popular of the medium-depth peels for facial rejuvenation is the Jessner’s–35% TCA peel. This peel has been widely accepted because of its broad range of uses, the large number of individuals in whom it is indicated, its ease of modification according to the situation, and its excellent safety profile.
The Jessner’s–35% TCA peel is particularly useful for the improvement of mild to moderate photoaging ( Fig. 154.5 ). It freshens sallow, atrophic skin and softens fine rhytides, with minimal risk of textural or pigmentary complications. Collagen remodeling occurs for as long as 3 to 4 months postoperatively during which time there is continued improvement in texture and rhytides. Deep furrows, however, are not eliminated with this peel and there is no significant skin retraction as is seen with ablative fractional laser resurfacing or deep chemical peels. When used in conjunction with a retinoid, bleaching agent and sunscreens, a single Jessner’s–35% TCA peel lessens pigmentary dyschromias and lentigines more effectively than repetitive superficial peels. Epidermal growths such as actinic keratoses also respond well to this peel. In fact, the Jessner’s–35% TCA peel has been found to be as effective as topical 5-fluorouracil in removing both grossly visible and clinically undetectable actinic keratoses, but has the added advantages of lower morbidity and greater improvement in associated photoaging .

Another indication for the Jessner’s–35% TCA peel is to blend the effects of other resurfacing procedures with the surrounding skin . Patients who have undergone ablative fractional CO 2 laser resurfacing, deep chemical peeling or dermabrasion to a localized area such as the periorbital or perioral region often develop a sharp line of demarcation between the treated and untreated skin. The treated skin may appear hypopigmented (also known as pseudohypopigmentation) in comparison to the untreated skin. These irregularities are often conspicuous and are troubling to the patient. A Jessner’s–35% TCA peel performed on the adjacent untreated skin helps to blend the treated area into its surroundings. For example, a patient with advanced photoaging in the periorbital region and moderate photoaging on the remaining face may desire fractional CO 2 laser resurfacing only around the eyes. In this patient, medium-depth chemical peeling of the areas not treated with the laser would improve the photoaging in these regions and avoid a line of demarcation ( Fig. 154.6 ). Similarly, a patient with acne or surgical scars having spot or regional dermabrasion or ablative fractional laser resurfacing to a facial cosmetic unit would benefit from a Jessner’s–35% TCA peel to the remainder of that cosmetic unit or to the rest of the face. It is important to note that when used in combination with other resurfacing procedures such as laser ablation or dermabrasion, the peel should be performed first, in order to avoid accidental application of the peeling agent onto previously abraded or laser-treated areas, which may lead to scarring ( Fig. 154.7 ).