Basic Definitions and Differential Diagnosis
Shraddha Desai
Jeffrey T.S. Hsu
Introduction
Primary care providers (PCPs) must understand multiple aspects of medicine. From headaches to foot pain, the physician must be prepared to address all of these conditions in an appropriate and timely manner. As more patients are being limited from seeing specialists, they turn to their PCP with more complex issues. This is especially true for dermatologic conditions. Often, dermatoses appear similar and are difficult to describe, resulting in delayed diagnosis. However, by understanding basic terminology and common presentations, PCPs can effectively diagnose skin conditions. It is our hope that this text will help PCPs deal with common dermatologic presentations.
Before one can accurately diagnose dermatologic conditions, learning the descriptive terminology is helpful. Being able to accurately describe skin lesions allows concise communication between providers, especially by telephone or electronic communication. This chapter attempts to summarize the common vocabulary of dermatology and to present that information in a usable format.
General Terms
A lesion is an area of altered skin. All dermatologic descriptions should include a primary and/or secondary lesion descriptor.
Primary lesion—the physical change in skin that is caused directly by the disease
Secondary lesion—the changes that occur in the skin after the evolution of the disease or resulting appearance after scratching or infection
Dermatosis: skin disease
“Dermatitis” and “eczema” are synonyms. In common usage, “dermatitis” is often used for acute rashes and “eczema” for more chronic rashes. Also, “eczema” is often used as a synonym for atopic dermatitis
Morphology: form or structure of a lesion
Maculopapule or “maculopapular”: There is no such thing as a maculopapule. This term is often used as a description for hypersensitivity-related dermatitis. A better descriptor in many cases would be “morbilliform.”
Primary Skin Lesions
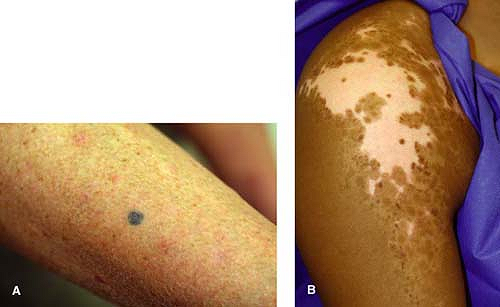
Macule—a flat area of color change that cannot be detected by touch (Fig. 1-1A)
Patch—a flat area greater than 1 cm (Fig. 1-1B)
Papule—a solid raised lesion less than 1.0 cm that can have a variety of shapes (acuminate, dome-shaped, etc.) and may be associated with secondary lesions like scale and crust (Fig. 1-2)
Nodule—a raised solid lesion that is more firm than a papule or plaque and often deeper (Fig. 1-3)
Tumor—a solid mass of the skin or subcutaneous tissue that is larger than a nodule (Fig. 1-4)
Plaque—a solid lesion greater than 1.0 cm, which is often elevated or thickened and formed by the confluence of papules (Fig. 1-5)
Vesicle—a small circumscribed collection of free fluid less than 1.0 cm in diameter (Fig. 1-6)
Bulla—a large circumscribed collection of free fluid greater than 1.0 cm in diameter (Fig. 1-7)
Pustule—a circumscribed elevated lesion (less than 1.0 cm) that contains purulent material (protein-rich and filled with neutrophils); an abscess is a larger collection of pus (Fig. 1-8)
Wheal—an area of swelling in the epidermis; transient (Fig. 1-9)
Burrow—a raised tortuous channel produced by a parasite (scabies) (Fig. 1-10)
Telangiectasia—a permanently dilated superficial blood vessel in the skin; this can be isolated or part of a larger condition such as ataxia telangiectasia (Fig. 1-11)
Secondary Skin Lesions
Scale—compact desquamated layers of stratum corneum that look like plates and flakes; these are caused by abnormal keratinization and shedding (Fig. 1-12)
Crust—the result of drying plasma and exudate on the skin (Fig. 1-13)
Atrophy—the thinning of epidermis or subcutaneous fat resulting in a depression of the skin (Fig. 1-14)

Figure 1-14 Atrophy. Cutaneous lichen sclerosus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access