Premalignant and Malignant Skin Lesions
Thanh-Nga T. Tran
Squamous cell carcinoma (SCC), basal cell carcinoma (BCC), melanoma, and Merkel cell carcinoma (MCC) are among the most common cutaneous malignancies encountered by primary care physicians as well as dermatologists. Primary skin malignancies account for more than 50% of all malignancies in the United States. There are more than 1 million cases of nonmelanoma skin cancers (NMSCs) as well as more than 60,000 cases of malignant melanoma diagnosed annually (melanoma in situ will account for an additional 46,000 cases). Approximately 75% to 80% of NMSCs are basal cell carcinomas (BCCs) and up to 25% are squamous cell carcinoma (SCCs). Although BCCs rarely metastasize and hence, rarely cause death, they can result in significant morbidity due to local invasion if not diagnosed and treated appropriately. SCCs, on the other hand, have a metastatic potential and can be locally aggressive, creating significant morbidity as well as mortality for the patient. Actinic keratoses (AKs) are the most commonly treated neoplasm of the skin, and are thought to be a precursor to SCCs. Melanoma, on the other hand, has remained one of the deadliest skin malignancies, and its incidence is on the rise, possibly related to the pattern of sun exposure. Therefore, it is imperative to recognize the cutaneous signs of melanoma and refer patients appropriately. Merkel cell carcinoma (MCC), while a relatively rare tumor of neuroendocrine origin, is also important due to its high rate of recurrence and relatively poor prognosis. The treatment and diagnosis of many cutaneous tumors are continually changing, and the role of clinicians (e.g., primary care providers, dermatologists, plastic surgeons, pathologists) focuses on an accurate diagnosis and a thorough understanding of the clinical sequelae. In addition, these rare cutaneous tumors are often difficult to diagnose based solely on the physical examination findings, and the proper diagnosis relies on excisional biopsy with histologic studies. This chapter focuses mainly on nonmelanoma skin cancers, with an emphasis on skin cancer precursors and Merkel cell carcinoma.
Pathogenesis
Ultraviolet radiation (UVR) is the major cause of NMSCs and AKs and has also been linked to MCC development. The sun emits UVR that is subdivided into UVA (400 to 320 nm); UVB (320 to 290 nm); and UVC (290 to 200 nm). More than 95% of the sun’s UVR that reaches the earth’s surface is UVA and about 1% to 10% of radiation that reaches the earth is UVB. Most UVC is absorbed by the ozone layer and oxygen in the atmosphere and is thus a very small source of adverse human health effects. UVR targets nucleic acids, proteins, lipids, and other macromolecules. The biologic consequences for DNA structure are
particularly striking with formation of “signature” mutations in the p53 gene. These are found frequently in human cancer and in more than 90% of skin cancer, specifically in SCC. P53 is a tumor suppressor gene that is a central factor in cellular stress response, and governs response to such insults as DNA damage, hypoxia, nucleotide imbalance, oxidative stress, and spindle damage. Modification of p53 occurs in a dose-dependent manner after exposure to UVR and the loss of p53 confers a survival advantage to UV-damaged cells. However, the role of p53 in melanoma is still unclear. The exact cause of MCC is unknown, but it appears to be linked to sun exposure and immunosuppression, with most cases occurring on sun-exposed areas of the body.
particularly striking with formation of “signature” mutations in the p53 gene. These are found frequently in human cancer and in more than 90% of skin cancer, specifically in SCC. P53 is a tumor suppressor gene that is a central factor in cellular stress response, and governs response to such insults as DNA damage, hypoxia, nucleotide imbalance, oxidative stress, and spindle damage. Modification of p53 occurs in a dose-dependent manner after exposure to UVR and the loss of p53 confers a survival advantage to UV-damaged cells. However, the role of p53 in melanoma is still unclear. The exact cause of MCC is unknown, but it appears to be linked to sun exposure and immunosuppression, with most cases occurring on sun-exposed areas of the body.
Risk Factors and Epidemiology
Although several associations have been established for skin cancer risk, such as skin phototype, immune response, viral infection, and genetic background, solar UVR is broadly accepted to be the main initiator and promoter of skin cancer, particularly basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). For SCC, the weight of evidence points toward “chronic” or total exposure. However, for BCCs, intermittent intense exposures as well as burning appear to have a greater influence on subsequent skin cancer risk. Most skin cancers cause a large immune response that is suppressed with continued actinic exposure, leading to reduced immune surveillance for mutated cells. Melanoma incidence has most strongly and consistently been associated with reported “intermittent sun exposure” that is mostly accrued through recreational activities. Among other risk factors are the use of tanning equipment, exposure to therapeutic UV sources such as psoralen plus UVA (PUVA) or narrow-band UVB for skin diseases; exposure to ionizing radiation; chemical exposure such as arsenic, pesticides, asphalt, and tar; infection with human papilloma virus (HPV), especially of the anogenital region in organ transplant patients, etc. Other possible risk factors include residence at high altitudes, dietary fat intake, tobacco abuse, thermal burns, and chronic ulcers.
The development of skin cancers can be influenced by genetics, such as in xeroderma pigmentosum (XP), a disorder of DNA repair mechanisms or in oculocutaneous albinism, a group of autosomal recessive disorders in which there is a variable degree of pigmentary dilution of the skin, eyes, and hair, leading to increased risk in development of skin cancers. BCC is associated with mutations that activate the proto-oncogene SMOOTHENED or that inactivate the tumor-suppressor PATCHED. Nevoid basal cell carcinoma syndrome (NBCCS) is a rare, autosomal dominant disorder, in which the underlying genetic defect is a mutation in the human PATCHED (PTCH) gene. Mutation in PTCH leads to loss of control of several genes known to play a role in both organogenesis and carcinogenesis, and this may explain both the congenital anomalies and cancer predisposition seen in NBCCS. BCCs can number from a few to thousands, making treatment decisions difficult.
One of the more important risk factors for the development of skin cancers, particularly SCCs, is immunosuppression. Several years after transplantation, AKs and SCCs begin to appear with increasing frequency. In organ transplantation patients, the risk of developing BCCs is 5 to 10 times that of the general population, whereas the risk for SCCs is 40 to 250 times greater, influenced by skin type, cumulative UV light exposure, age at transplantation, direct carcinogenic effects of immunosuppressive medications, HPV infection, and the degree and the length of immunosuppression. Of the two cancers, SCCs can cause significant morbidity and mortality in transplant patients, as the lesions tend to be more numerous, especially in sun-exposed areas with greater risk of local and regional recurrences. HPV DNA is found in approximately 70% to 90% of transplant-associated SCCs.
MCCs have been linked to sun exposure, with most cases occurring on sun-exposed areas of the body, as well as to immunosuppression, exposure to other sources of ultraviolet light, and certain conditions such as HIV infection, chronic lymphocytic leukemia, Hodgkin lymphoma, ectodermal dysplasia, and Cowden disease. Other possible causes include exposure to arsenic and treatment for psoriasis that uses psoralens and ultraviolet-A light (PUVA).
Among women under 40, the rate of BCC has tripled in the past 30 years, while that of SCC has quadrupled. At current rates, 1 in 5 people in the United States will develop a skin cancer of some sort during their lifetime, with more than 1 million new cases appearing in 2008 alone. The lifetime risk in the United States of invasive melanoma has increased from 1:1,500 in 1935 to 1 in 63 for invasive melanomas and 1 in 33 if in situ melanoma is included, in 2007. In the United States, melanoma is the most common form of cancer in young adults 25 to 29 years old and the second most common cancer in adolescents and young adults 15 to 29 years old. One American dies from melanoma almost every hour (every 62 minutes). Although melanoma accounts for only 5% of total cutaneous malignancy, it is responsible for approximately 75% to 80% of skin cancer-related deaths. Approximately 1,200 new cases of MCCs are diagnosed in the United States each year with the incidence rising, with a 3-fold increase between 1986 and 2001.
 |
A 65-year-old patient with skin phototype I who spent his childhood on the beach came in to the office due to rough, scaly spots on his scalp and forehead (Fig. 7-1). None has bled or grown rapidly. However, they just “do not go away.” He seeks diagnosis and treatment. What is the most likely diagnosis? What test can be done to confirm the diagnosis?
Premalignant Skin Lesion
Actinic Keratosis
Background
Actinic keratoses (AK) are some of the most frequently encountered lesions in clinical practice. Individuals most at risk include the elderly, those with lighter skin types, and those with a history of chronic sun exposure. They have historically been characterized as being “precancerous” or “premalignant” because the atypical keratinocytes within these lesions are confined to the epidermis, not yet reaching full thickness invasion characteristic of carcinomas. The likelihood of an invasive SCC evolving from a given AK has been estimated to occur at a rate of 0.075% to 0.096% per lesion per year, and the rate of development of SCCs for a typical average number of 7.7 AKs per person can range anywhere from 10% to 20% over 10 years if lesions are left untreated.
Pathogenesis
AKs are induced by UV radiation, occurring more frequently in fair, red-haired, or blonde patients who burn frequently and tan poorly (Fitzpatrick’s skin phototype I and II; Table 7-1). Increased sun exposure and higher-intensity exposure increase the chance of AK development as well as immunosuppression following organ transplantation.
Key Features
The actinic keratosis is one of the most frequently encountered lesions in clinical practice.
They are most commonly present on sun-exposed areas of face, ears, scalp, dorsal hands, forearms.
These lesions represent in-situ dysplasia (precancer) resulting from sun exposure.
Clinically, they are discrete, flat or elevated, gritty lesions that can have associated erythema, pigmentation or an adherent scale.
Clinical Presentation
Most often, the primary lesion is a rough, erythematous patch or papule with gritty white to yellow scale that may be associated with tenderness and may range in size from a few millimeters to large confluent patches several centimeters in diameter, especially in heavily sun-exposed individuals. A typical
hypertrophic AK is shown in Figure 7-1. On palpation, the surface is rough, sandpaper-like, and could be more easily felt than seen due to their rough, gritty texture. One of the earliest signs is slight erythema with almost imperceptible adherent scale usually on a background of solar damage such as dyspigmentation, telangiectasia, and wrinkling. More advanced lesions are typically thicker with more visible hyperkeratosis and erythema or even a cutaneous horn. Sun-exposed areas are most often involved. Sites such as the tops of the ears, upper forehead, nasal bridge, malar eminences, dorsal hands, extensor forearms, and scalp in bald individuals must be examined. Lesions larger than 6 mm are suspicious for squamous cell carcinoma and should be biopsied.
hypertrophic AK is shown in Figure 7-1. On palpation, the surface is rough, sandpaper-like, and could be more easily felt than seen due to their rough, gritty texture. One of the earliest signs is slight erythema with almost imperceptible adherent scale usually on a background of solar damage such as dyspigmentation, telangiectasia, and wrinkling. More advanced lesions are typically thicker with more visible hyperkeratosis and erythema or even a cutaneous horn. Sun-exposed areas are most often involved. Sites such as the tops of the ears, upper forehead, nasal bridge, malar eminences, dorsal hands, extensor forearms, and scalp in bald individuals must be examined. Lesions larger than 6 mm are suspicious for squamous cell carcinoma and should be biopsied.
Table 7-1 Fitzpatrick’s Skin Phototypes | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Diagnosis
Differential Diagnosis
The differential for AK must include the possibility of invasive squamous and basal cell carcinoma, although these lesions tend to be more indurated and nodular, with more rapid growth and often eroded and ulcerated surface. Other diseases to consider include:
Discoid lupus erythematosus, which has more dyspigmentation, dilated follicles, and atrophy
Seborrheic keratosis: greasy, brown crusts; sharply demarcated borders; but does not have an erythematous scaly base; may occur in non sun-exposed areas
Bowen disease: a larger plaque with a sharp outline
Warts: tend to be more verrucous with punctate red dots representing thrombosed capillaries
Porokeratosis: a premalignant lesion characterized by small, light brown, keratotic papule or plaque that forms irregularly shaped, annular plaque with a raised, ridgelike border. The risk of malignant degeneration is ∼10% with large, long-standing lesions being at highest risk. Most lesions can be followed clinically unless atypical features are seen.
Diagnostic Methods
Visualization and palpation is helpful for the diagnosis of AKs. However, in the case that malignancy is suspected, a biopsy is recommended.
Therapy
It is impossible to predict the fate of AKs as they may remain unchanged, spontaneously resolve, or progress to invasive SCC. Although the risk of progression of any one AK to invasive SCC is small, a patient may have many lesions, increasing the risk of malignant progression. Because therapy is generally well tolerated and simple, treatment is warranted.
First and foremost in management of AKs is medical education regarding chronic sun exposure, especially during the hours from 10:00 AM to 4:00 PM when sunlight is more intense. Adequate use of sunscreen of a sun-protection factor (SPF) of 30 or above is recommended. There are two broad categories of treatments, medical therapy and surgical therapy.
Medical Therapy
Medical therapy or field therapy is useful in patients with numerous AKs on a background of severe sun damage where individual lesion therapy is difficult. This has the advantage of being able to treat large areas with many lesions, although it is often associated with lengthy treatment course as well as prolonged discomfort and irritation. Currently, the U.S. Food and Drug Administration (FDA) has approved four medications for the treatment of AKs. These are topical 5-fluorouracil (5-FU), 5% imiquimod cream, topical diclofenac gel, and photodynamic therapy (PDT) with topical delta-aminolevulinic acid (ALA-PDT).
5-FU has been used more extensively before the development of imiquimod. Several formulations are available, including a 5% cream or solution, a 2% solution, a 1% cream or solution, and, most recently, a micronized 0.5% cream with relatively little difference among the various formulations. The most popular is the 5% cream, which is applied twice daily for 1 month. Patient must be warned that the lesions will likely become increasingly erythematous, leading to possible significant discomfort and can be temporarily disfiguring, with erythematous ulcerations and crust formation. However, if the patient completes the treatment, the lesions usually heal within 2 weeks of stopping treatment, resulting in improved texture of the skin (smoother) as well as reduction in number and size of AKs.
Imiquimod is a topical medication that up-regulates a variety of cytokines, invoking a nonspecific immune response (interferons, macrophages, natural killer cells) and a specific immune response (T lymphocytes). It is applied 2 to 3 times a week for up to 4 months. Reaction to the medication can range from barely perceptible erythema to exudative inflammation, including reaction of subclinical lesions. For patients with a brisk inflammatory response, the dose can be reduced to one to twice a week without significant change in therapeutic efficacy.
Topical diclofenac is a nonsteroidal anti-inflammatory drug with unclear mechanism of action against AKs. It is an effective therapy when applied twice a day for 3 months with the chief advantage in that it produces little to no inflammation and thus is very well tolerated.
ALA-PDT uses delta-aminolevulinic acid, a light-sensitizing compound that preferentially accumulates in dysplastic AK cells, converting intracellularly via enzymatic processes to protoporphyrin IX, a potent photosensitizer. Upon exposure to light at an appropriate wavelength, oxygen free radicals are generated and cell deaths results. The side effect can be similar to topical 5-FU, with intense erythema and irritation, as well as pain, although only one treatment is needed usually.
Surgical Care
Surgical management of AKs often involves physical destruction with limited to no damage to surrounding normal tissue. When the diagnosis is unclear and
invasive tumor is possible, biopsy is indicated. The most common method of physical destruction involves cryosurgery, where a cryogen—most often liquid nitrogen with a temperature of -195.8°C—is sprayed precisely on an AK lesion. Keratinocytes die when exposed to approximately -40 to -50°C, whereas other structure in the skin, such as collagen, blood vessels, and nerves, are more resistant to the lethal effects of cold than keratinocytes. Melanocytes are much more cold sensitive, and hence can also be destroyed during this process, leaving a white spot. Overall, the clearance rate is 67%.
invasive tumor is possible, biopsy is indicated. The most common method of physical destruction involves cryosurgery, where a cryogen—most often liquid nitrogen with a temperature of -195.8°C—is sprayed precisely on an AK lesion. Keratinocytes die when exposed to approximately -40 to -50°C, whereas other structure in the skin, such as collagen, blood vessels, and nerves, are more resistant to the lethal effects of cold than keratinocytes. Melanocytes are much more cold sensitive, and hence can also be destroyed during this process, leaving a white spot. Overall, the clearance rate is 67%.
If malignancy is suspected, a lesion can be treated with curettage, shave excision, or conventional excision, and the tissue can be sent for histologic examination. Side effects include possible reaction to local anesthesia, wound infection, and scarring.
Other methods include ablative laser resurfacing procedures where the entire epidermis is removed (such as in carbon dioxide laser resurfacing) can also be effective though almost never performed. Less invasive resurfacing procedures include medium and deep chemical peels as well as dermabrasion. All of these are cosmetic procedures unlikely to be covered by insurance; all carry the risk of scarring and postinflammatory hyperpigmentation or hypopigmentation, especially in darker-skinned individuals.
“At a Glance” Treatment
Medical care:
Imiquimod cream: used applied 2 to 3 times a week for up to 4 months
5-fluorouracil cream: often 0.5% prescribed at once daily to the affected field and/or discreet lesions for 4 weeks
Diclofenac cream and ALA-PDT are less commonly used.
Surgical care:
Cryosurgery with liquid nitrogen
Less commonly used: chemical peels, photodynamic therapy
Refer patients with significant sun damage and rough lesions on skins, or for skin lesions that do not resolve with cryosurgery or medical therapy, and patients with numerous skin lesions requiring comprehensive treatments such as ALA-PDT.
Lesions that are tender to touch and/or rapidly growing should be biopsied to rule out invasive SCC.
Field therapy for patients with multiple AKs is beneficial and worth the up-front treatment side effects of inflammation.
Course and Complications
Complications are most often seen in patients with severe actinic damage treated aggressively with cryotherapy or medical therapy. In these patients, blisters may form and exudative inflammation may cause pain, discomfort, and pruritus, as well as increase the risk for infection. Untreated lesions may progress into invasive squamous cell carcinomas especially nodular, indurated, or unresponsive lesions, where a biopsy is warranted.
ICD9 Codes
| 702.0 | Actinic keratosis |
 |
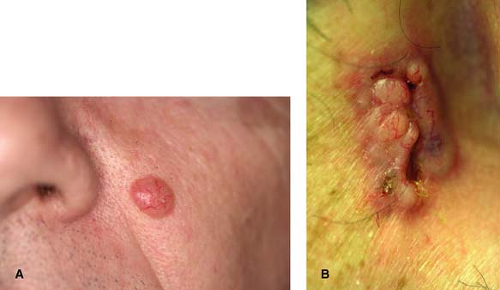
A 55-year-old construction worker who spends most of his days out in the sun develops a skin-colored pearly growth on his medial cheek (Fig. 7-2A) that has been slowly growing over the past year and occasionally bleeds with trauma. What is the most likely diagnosis? What should the treatment be?
Malignant Skin Lesions
Basal Cell Carcinoma
Background
Basal cell carcinoma (BCC) is the most common malignancy, primarily among white, fair-skinned population. Risk factors include chronic sun exposure, positive family history for BCC, immunosuppression, prior blistering sunburns, red hair/fair complexion, skin phototype I and II. BCC is usually slow growing and rarely metastasizes, but it can cause
clinically significant local destruction and disfigurement if neglected or inadequately treated. However, prognosis is excellent with proper therapy. Many clinical variants exist and diagnosis is dependent on the clinician being aware of the many forms BCC may take. Treatment is often tailored on the histologic variant.
clinically significant local destruction and disfigurement if neglected or inadequately treated. However, prognosis is excellent with proper therapy. Many clinical variants exist and diagnosis is dependent on the clinician being aware of the many forms BCC may take. Treatment is often tailored on the histologic variant.
Key Features
Basal cell carcinomas (BCC) are the most common of all cancers in the United States.
No universally accepted classification exists for BCC and at least 26 different subtypes have been described.
Typically BCC appears on sun-exposed skin, are slow growing, and rarely metastasize.
Neglected tumors can lead to significant local destruction and disfigurement.
Prognosis is excellent with proper therapy.
Pathogenesis
The true pathogenesis for BCCs has not exactly been elucidated, although UVR has been shown to be associated with the development of BCCs. Intermittent intense exposures as well as burning appear to have a greater influence on subsequent BCC development. UV-induced mutations in the p53 tumor-suppressor gene have been found in some cases of BCC. Activated BCL2 (an antiapoptosis proto-oncogene) also is commonly found in BCCs and may be detected immunohistochemically. Most BCCs have abnormalities in either patched (PTCH) or smoothened (SMO) genes, which are involved in the hedgehog intracellular signaling pathway, which influences differentiation of a variety of tissues during fetal development, as well as regulation of cell growth and differentiation after embryogenesis. Loss of inhibition of this pathway is associated with human malignancy, including BCC. Other associated risk factors include immunosuppression, arsenic exposure, exposure to artificial UV light such as tanning booths and UV light therapy, certain genodermatoses such as xeroderma pigmentosum, nevoid basal cell carcinoma syndrome with defects in PTCH and SMO genes, as well as history of other NMSC. The risk of developing new nonmelanoma skin cancers is reported to be 35% at 3 years and 50% at 5 years after an initial skin cancer diagnosis.
Clinical Presentation
Most often the nodular BCC characterized by a pearly papule with surface telangiectasia (Fig. 7-2A) and rolled border (Fig. 7-2B) is the typical lesion. However, several clinical and histologic subtypes of BCC may exhibit different clinical and histologic appearance such as superficial (Fig. 7-3); morpheaform (Fig. 7-4); micronodular (Fig. 7-5); or pigmented BCC (Fig. 7-6). Good lighting and magnification is helpful, as well as palpation, and stretching of the skin may help to delineate the tumor and estimate its size and depth. Oblique illumination of the tumor can highlight surface changes, such as a rolled border. Features of BCC are reviewed in Table 7-2.
Table 7-2 Common Types of Basal Cell Carcinoma | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|