The term “Asian blepharoplasty” refers specifically to the surgical creation of an upper eyelid crease amongst people of Southeast Asian descent. Unlike traditional blepharoplasty, which is typically performed on persons of Western descent, Asian blepharoplasty is more commonly performed on younger individuals for cosmetic reasons. It is now recognized that the creation of the “Western” high crease is neither cosmetically pleasing nor natural-appearing on the Asian face, thus a successful result requires a clear understanding of anatomy as well as meticulous surgical planning. ,
In this chapter, authors discuss eyelid morphology, anatomic details, pre-operative assessment, and surgical techniques as they relate to Asian blepharoplasty.
Defining the asian eyelid
As there is a high degree of variability amongst Asian eyelids, a one-size-fits-all approach will yield suboptimal results. There is a common misconception that all Asians are born without an upper lid crease, however, approximately half of the Asian population do have a natural crease.
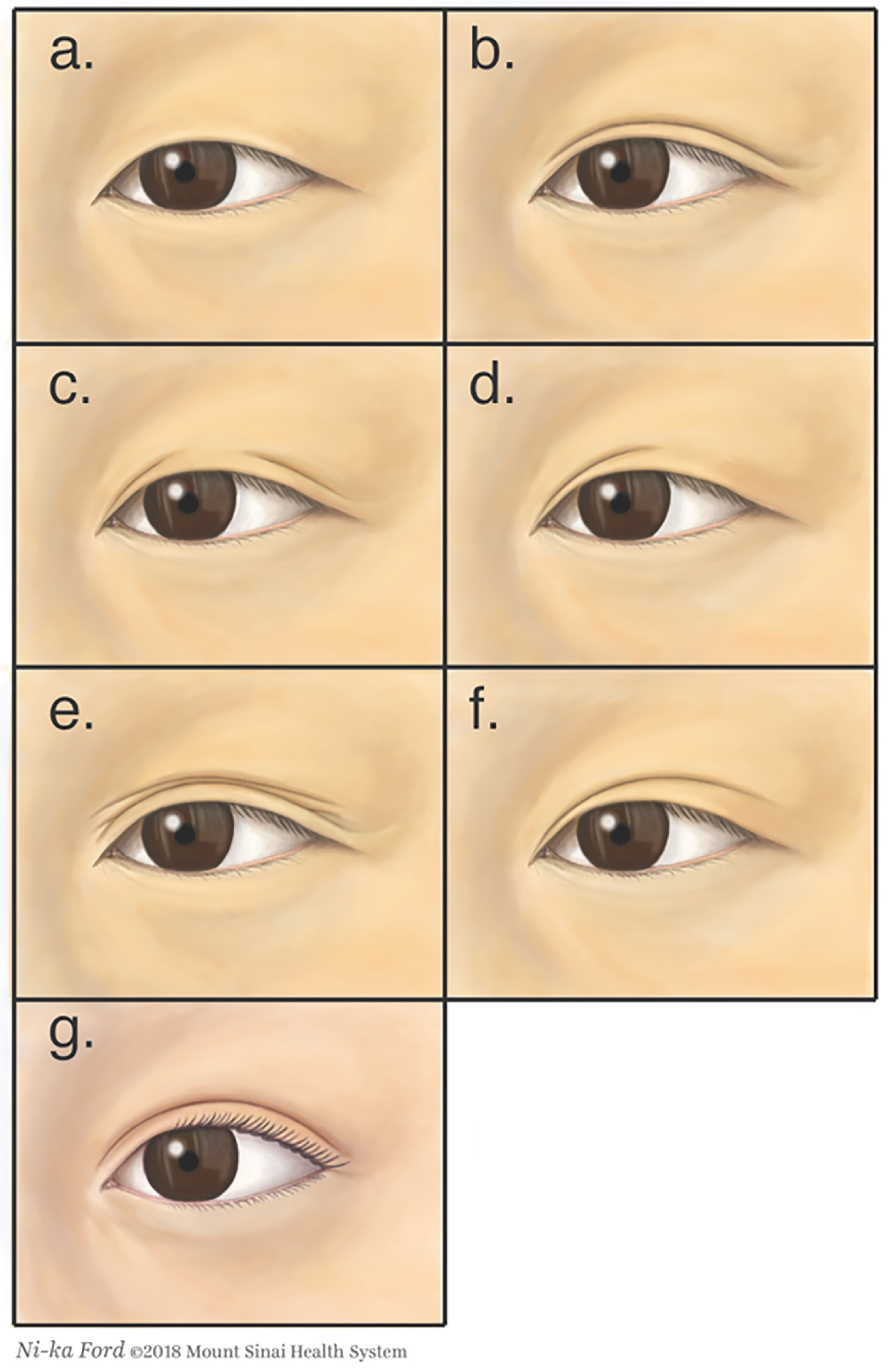
Chen has previously described the seven major variations of the Asian eyelid ( Fig. 6.1 ). ,
- a.
In approximately half of Asian eyelids, there is no eyelid crease.
- b.
Asian eyelid with a parallel eyelid crease: the parallel crease runs parallel to the eyelid margin over the entire length of the eye, independent of the medial canthal fold
- c.
Asian eyelid with a segmented eyelid crease
- d.
Asian eyelid with a partial or incomplete eyelid crease
- e.
Asian eyelid with multiple eyelid creases
- f.
Asian eyelid with a nasally tapered crease: the nasally tapered crease is a low-set crease running parallel to the eyelid margin for the lateral two-thirds of the eye, then converging inwards to join the medial canthus (in a small percentage of cases, it exhibits some lateral flare)
- g.
The typical Caucasian eyelid with a semilunar crease is rare in Asian eyelids
Other notable findings in the Asian eye include a fullness or puffiness of the upper eyelid, which can give the impression of a smaller palpebral fissure; an upward lateral canthal tilt; and an epicanthal fold. The surgical implications of these variations will be discussed separately.
Anatomy of the asian eyelid and surgical implications
Much of our knowledge regarding the anatomy of the Asian eye comes from cadaver studies ( Fig. 6.2 ). There is no significant difference in the skin and orbicularis muscle between Caucasians and Asians; although patients who lack an eyelid crease may actually have hypertrophied orbicularis muscle.
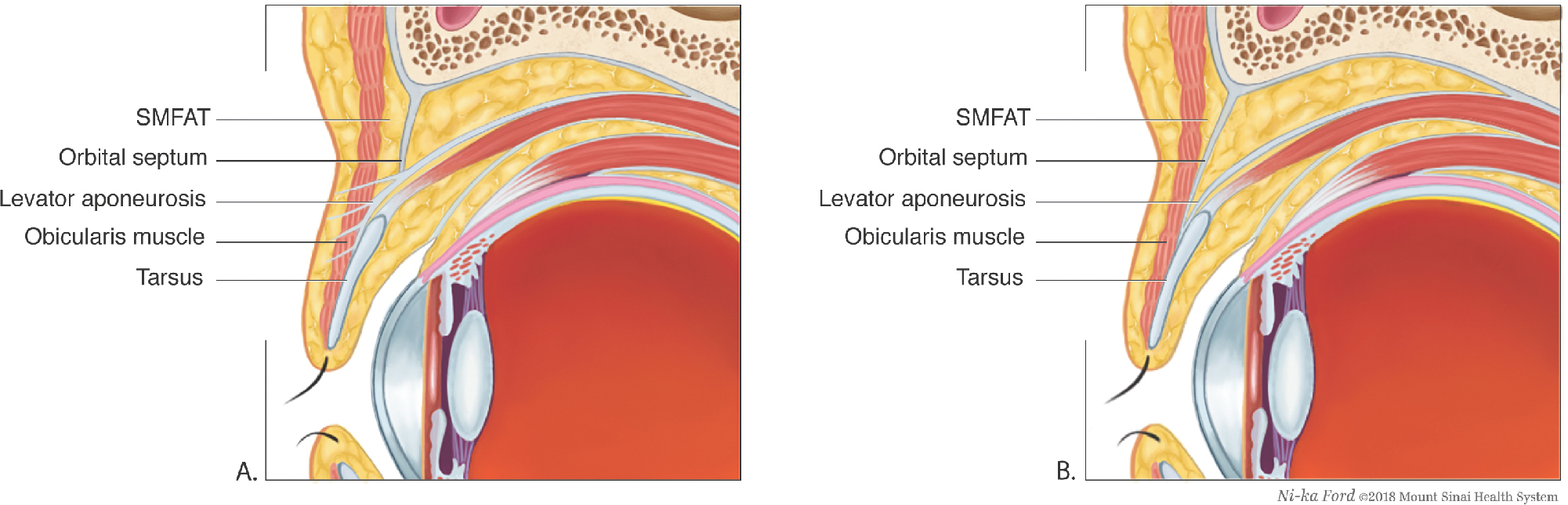
The submuscular fibroadipose tissue (SMFAT) lies between the orbicularis muscle and the orbital septum. In Caucasians, this tissue has little significance; however, in Asians, the SMFAT forms the thickness of the upper eyelid.
Underlying the SMFAT is the orbital septum; a sheet of fibrous tissue originating from the periorbita, that separates into two layers distally. The posterior layer reflects and attaches to the anterior layer of the levator aponeurosis; the anterior layer extends to the lid margin. In Caucasians, the orbital septum typically fuses to the aponeurosis around 3.7 mm higher than the superior tarsal border (STB), which prevents preaponeurotic fat descent during eye opening. Traditionally, this fusion point was thought to be lower across East Asians as compared to Caucasians; however, recent works by Kakizaki et al. suggests that the lower extension of the preaponeurotic fat is the main factor in maintaining a lower eyelid crease in Asians. In Asians, the preaponeurotic fat may actually cover part of the tarsal plate.
In Asians, the average tarsal height is approximately 9.2 mm, which is significantly shorter than in Caucasians (11.3 mm). ,
Preoperative evaluation
Asian patients who present for creation of an upper eyelid crease often have a clear idea of their desired cosmetic outcome. Initial consultation should focus on patients’ specific goals and aesthetic expectations. This is facilitated by the use of a straightened paper clip to temporarily create an upper eyelid crease by invaginating the pretarsal skin at the desired height. This allows the patient to evaluate potential postoperative outcomes with the crease set at various levels.
The surgeon should also ascertain whether the patient has undergone previous surgical correction, as any residual scar tissue secondary to previous surgical augmentation may make the planned operation significantly more challenging. Weakened orbicularis muscle also predisposes to a higher risk of eyelid malposition or symptomatic lagophthalmos.
The upper eyelid in Asians is often fuller or “puffier” and should be carefully evaluated for hypertrophied fat pads, which may hinder natural crease formation and steer the surgeon toward an external incisional approach with debulking of the fat pads. The surgeon may also observe multiple shallow creases; these are not true eyelid creases, but more commonly the result of brow ptosis or skin laxity. The effect of brow ptosis can be neutralized by using one’s hand to immobilize the frontalis muscle. Measurement of lid crease is best performed when the eye is looking down or closed; otherwise, the natural tilt of the Asian lid crease combined with any overlying skin fold may cause the measured crease height to be lower than the anatomic height. ,
Compared to Caucasians, most Asians have a mild ptosis with average margin reflex distance 1 (MRD1) of 3 to 3.5 mm. An MRD1 less than 3 mm should prompt the examiner to distinguish between pseudoptosis and true ptosis.
Asians with epiblepharon may have downturning of the upper eyelashes, causing trichiasis. The creation of a double eyelid can help evert the cilia; however, if ptosis is surgically overcorrected, it may result in upturning of the cilia with exposure of the palpebral conjunctiva. The direction of the ciliary turn should be carefully noted preoperatively.
Surgical techniques
There are three principal techniques for the surgical creation of an upper eyelid crease:
- 1.
External-incision method (ideal for older patients who concomitantly need removal of excess skin and muscle plus/minus excess fat)
- 2.
Partial-incision method (ideal for younger patients since there is no need for skin excision)
- 3.
Suture ligation method (a quick procedure with a short recovery period, but this technique does not enable the removal of skin and fat and therefore does not usually yield a long-lasting result)
Surgical technique—external incision method
The most commonly performed external incision technique described by Chen involves removal of a variable amount of skin, orbicularis oculi, and pre-aponeurotic fat. , The lid crease-enhancing sutures are placed as skin–levator aponeurosis–skin (SLS) or skin–tarsus–skin (STS). ,
First, the upper lid is everted, and a caliper is used to measure the vertical height of the central portion of the tarsal plate (typically 6.5 to 7.5 mm in Asians). The lid is returned to its natural position, and a mark is made at the central point of the crease incision at a height corresponding to that of the tarsus measured. For a natural appearance, the lid crease incision should not be made higher than the level of the tarsus. Depending on the crease shape chosen, the crease marking is merged toward the medial canthus (nasally tapered) or the marking stays parallel to the lash line as the mark approaches the medial canthus (parallel crease). This first marking is the lower incision line, or eyelid crease line. The upper incision line is determined using the patient’s age and degree of skin laxity. Typically, this includes 1.5 to 2 mm of skin in younger patients and up to 10 mm in older patients. The superior margin is marked while using a Bishop Harman forceps to gently pinch the excess skin.
Next, a Bovie needle tip is used to dissect through the orbicularis until part of the septum is opened; a beveled approach allows more of the posterior fibers of the orbicularis above the upper incision to be thinned. The septum is opened transversely; at this point, partial reduction of fat may be performed to allow natural crease indentation without the placement of closing or buried sutures. In most cases, it is advisable for the surgeon to focus on nasal fat pad removal, taking a conservative approach when addressing the central fat pad. However, the removal of fat should be minimized to avoid a sunken sulcus appearance. After removing the remaining strip of skin-orbicularis, it is important to remove the surgical drapes from the forehead to reveal natural anatomy minimizing any tension placed on the skin, thereby preventing the placement of a high crease. , ,
The next step is eyelid crease construction, which falls into two broad categories:
- •
Skin–levator–skin SLS (or skin–tarsus–skin STS)
- •
Levator aponeurosis to inferior subcutaneous plane (or STB to inferior subcutaneous plane)
Many practitioners favor the first approach, SLS, in which the suture first passes through the inferior skin edge, then the distal fibers of the levator aponeurosis along the STB, and then through the upper skin edge ( Fig. 6.3 ). This creates an attachment between the levator aponeurosis and the subdermal area, mimicking the natural insertion of the levator aponeurosis. In contrast, the STS approach does not incorporate fibers of the levator aponeurosis. Previous surgeons have suggested that the SLS approach creates a more dynamic crease, whereas the STS approach produces a more static crease.