Chapter 1 Anatomy of the Tendon Systems in the Hand
Outline
Flexor Retinaculum
This retinaculum inserts on the ulnar side into the pisiform bone and the hook of the hamate and is reinforced by the pisiform-hamate ligament. On the radial side, the retinaculum firmly inserts into the volar ridge of the trapezium (trapezial tuberosity) and the tubercle of the scaphoid. Occasionally an insertion into the styloid process of the radius can be seen.1,2
Controversial terminology surrounds this strong, fibrous band that crosses the volar side of the carpus. According to the Terminologia Anatomica, the term flexor retinaculum carpi should be used. However, in textbooks, the terms flexor retinaculum, transverse carpal ligament and anterior/volar annular ligament are used for the same structure.3
In hand surgery, it is often preferred to distinguish between the different parts of the flexor retinaculum. Stecco et al3 investigated its histological and anatomical features. Continuous with the antebrachial fascia, a fibrous reinforcement was identified at the volar side of the wrist. After removal of this layer, another fibrous layer was found, with strong lamina and histological similarities to those of a ligament. According to Stecco’s group,3 “ligament derives from Latin ligare (to bind) and means a sheet or band of tough fibrous tissue connecting bones.” They stated that “the role of the pulley for the tendons of the flexor muscles is assumed above all” for this deeper layer covering the carpal tunnel, and therefore the term transverse carpal ligament was suggested to be the most appropriate.
In addition to the thickened continuation of the antebrachial fascia and the transverse carpal ligament, Cobb et al4 described a third, more distal segment composed of an aponeurosis between the thenar and hypothenar muscles. Based on their anatomical findings, they advocate a more extensive release when dividing the carpal ligament.
Tanabe and Okutsu5 endoscopically released the flexor retinaculum in management of carpal tunnel syndrome and found that the mean distance between the ends of the retinaculum increased from 1.3 mm to 6.6 mm if the distal fibers were also divided. They therefore concluded that sectioning of the distal fibers is essential for endoscopic carpal tunnel release.
Extensor Retinaculum
As studied by Taleisnik et al,6 the deep antebrachial fascia begins to thicken proximal to the radiocarpal joint and becomes the dorsal annular ligament, a component of the extensor retinaculum of the wrist. Distally, this supratendinous layer is continuous with the pretendinous fascia of the hand. On the ulnar side, it inserts in three distinct places: proximal around the flexor carpi ulnaris tendon, the middle part into the triquetrum and pisiform bone, and distally onto the fascia of the abductor digiti quinti and base of the fifth metacarpal.
Within the supratendinous layer, at the floor of the fourth and fifth compartment, lies the infratendinous layer, from which circular fibers form a tube around the tendons within the compartments. In the sixth compartment, a duplication of the infratendinous layer forms a tube around the extensor carpi ulnaris (ECU) tendon from the ulnar styloid to the triquetrum. This subsheath stabilizes the tendon along the groove in the distal ulna and contributes to the stability of the distal radioulnar joint. Proximally, longitudinal fibers form the linea jugata that reinforces the tendon to prevent subluxation during full supination. The ECU subsheath is frequently injured, typically in young athletes who play racket or stick sports, which can result in recurrent subluxation of the ECU tendon.7
Flexor Tendons in the Hand
The tendons in the wrist have a relatively constant arrangement with the median nerve. This arrangement varies mainly when muscle or tendon anomalies are present. It is important to keep these variations in mind, because it can be confusing even for the experienced surgeon. Usually, the median nerve can be found directly under the tendon of the palmaris longus. Sometimes, the nerve lies more superficial, next to the palmaris longus tendon. The median nerve is also frequently observed to split in the forearm.8
The palmaris longus tendon lies completely enclosed in the deep fascia of the forearm between the superficial veins and cutaneous nerves. The presence of this tendon is highly variable, as its absence has been reported from 0.6% to 63.9% (either bilateral or unilateral) among different populations all over the world.9 In humans, this tendon is seen as rudimentary, and for that reason, and its easy accessibility, the palmaris longus is often used as a tendon graft.
To the radial side of the median nerve, the FPL tendon can be found; to the ulnar side, the superficial flexor tendons. When coursing through the carpal tunnel the superficial flexor tendons are arranged in pairs, the tendons to the middle and ring finger form the superficial pair, and the little and index finger tendons form the deep pair. Dorsal to the superficial tendons lie the flexor profundus tendons.2,8
In the case that the palmaris longus tendon is absent, the tendon of the flexor superficialis indicis can sometimes be found between the superficial flexor tendon to the middle finger and the median nerve. In other variations, the palmaris longus tendon can separate into two or three tendons, the muscle can be doubled, the muscle can be reversed or inverted, and partial or complete insertion in the antebrachial fascia can be seen. Additionally, insertion into the pisiform bone, scaphoid, flexor carpi ulnaris tendon, and muscles of the thenar has been observed.8
Accessory slips for the FDS and FDP are frequently observed, especially to the index finger. Slips arise from the ulnar tuberosity to the superficialis tendon of the index and middle finger, and from the annular ligament to the superficialis tendon of the little finger. The superficialis tendon to the little and index finger can be absent and the index finger’s deep flexor tendon can divide into two tendons or have a shared origin with the FPL.8
The flexor carpi radialis (FCR) tendon courses through its own synovial sheath that forms a narrow osteofibrous tunnel when passing the trapezium. The radial side of the tunnel is formed by the body of the trapezium and the volar side by the trapezial tuberosity. On the ulnar side, the tunnel is separated from the carpal tunnel by a thick septum. Distally, the FPL tendon pivots around this septum. At the floor of the tunnel, the tendon sheath lies in contact with the volar capsule of the scaphotrapeziotrapezoid (STT) joint. The narrow tunnel induces a higher risk of primary stenosing tenosynovitis; however, because of the close relationship with surrounding structures, tenosynovitis can also occur secondary to traumatic or degenerative changes. Tenosynovitis of the FCR tendon is not an uncommon finding in arthritis of the STT joint, which can cause additional pain to the baseline osteoarthritic pain.10,11
The FCR tendon is also suggested to play a role in stabilizing the scapholunate joint through its close relationship between the FCR tendon sheath and the ligaments attached to the tuberosity of the scaphoid. The tendon was thought to use the distal pole of the scaphoid as a pulley to increase its mechanical advantage and prevent the scaphoid from rotating into flexion. Unlike in previous hypotheses, Salvà-Coll et al12 found that loading the FCR tendon rotated the scaphoid in flexion and supination, while rotating the triquetrum in flexion and pronation. These opposite rotations are attributed to relax the dorsal scapholunate ligament.
The FCR tendon inserts into the base of the second metacarpal and gives off a strong, tendinous slip to the third metacarpal. Frequently a small slip to the trapezial tuberosity can be seen. Other variations are insertions in both the trapezium and scaphoid and in the base of the second, third, and fourth metacarpals. The FCR muscle can even be absent. Insertion in the transverse carpal ligament can also be seen and may cause confusion with the palmaris longus tendon.8
The flexor carpi ulnaris (FCU) encloses the pisiform bone, which can be seen as a sesamoid bone for this tendon. The FCU attaches to the base of the fifth metacarpal and hamate, via the pisohamate and pisometacarpal ligaments. The pisohamate ligament creates an additional tunnel, Guyon’s canal, between the hook of the hamate and pisiform bone through which the ulnar artery and nerve pass. Occasionally, the FCU tendon doubles before inserting in the pisiform bone. The FCU can also merge with the flexor superficialis or profundus tendon.8
The FPL tendon passes through its own osseo-aponeurotic canal and inserts at the distal phalanx of the thumb. Sometimes an additional tendon to the index finger is found. The FPL tendon can be absent, in combination with a significant smaller thumb. Another variation is splitting of the tendon into two or three slips that insert into the scaphoid or flexor retinaculum.8
Flexor Tendon Sheaths
Structure of the Sheath at Wrist and Palm
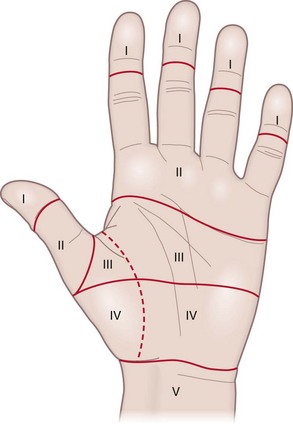
In the wrist, synovial sheaths allow the flexor tendons to glide through the carpal tunnel. The sheaths begin approximately 2.5 cm proximal to the transverse carpal ligament and extend distally to the neck of the metacarpals. In the fingers, the flexor tendons are also surrounded by sheaths. A considerable level of variation in communicating patterns between these sheaths and the digital flexor sheaths is observed.13
As reported by Fussey et al,13 the most common pattern shows one common flexor tendon sheath or ulnar bursa surrounding the tendons of the FDS and FDP. A second sheath, forming the radial bursa, envelopes the FPL tendon.
In most cases the little finger flexor sheath works in continuity with the tendons along the phalanges. Likewise, the FPL tendon sheath accompanies the tendon along the thumb as far as its insertion.13
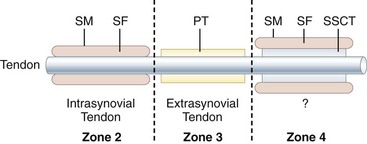
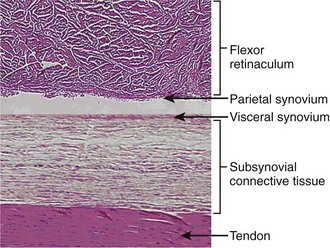
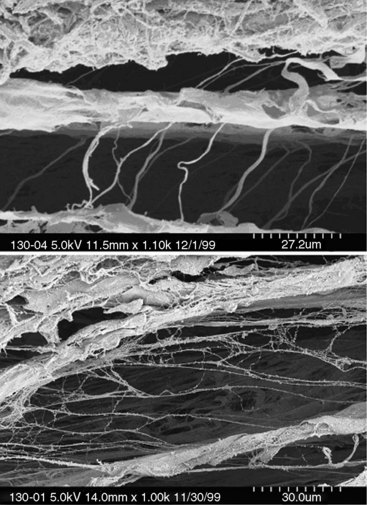
In the carpal tunnel, the subsynovial connective tissue (SSCT) connects the flexor tendons with the synovial membrane of the ulnar bursa. It consists of fibrous bundles parallel to the tendons, which in turn are interconnected by smaller microfibrillar fibers. By acting as a sliding unit, the SSCT reduces friction and maintains the integrity of the vascularity around the tendons. Noninflammatory fibrosis of the SSCT is the most common histological finding in carpal tunnel syndrome, which suggests injury to the SSCT to be an important etiologic factor14 (Figures 1-1 to 1-4).
Structure of the Digital Flexor Sheath
In a histological study of the flexor tendon sheath by Cohen and Kaplan,15 two vascular systems are observed to become organized in the paratenon; one adjacent to the tendons, the other more peripheral. The development of a “synovial-lined cleft” between these systems creates a separation into a visceral and a parietal synovium.
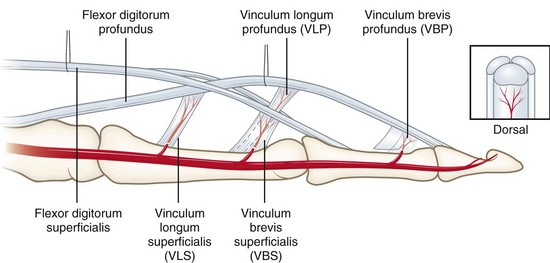
Vincula Tendinea
Several variations in the vincula tendinea have been observed. Ochiai et al16 studied the distribution patterns of the vincula in the fingers of 35 human hands. Their study showed that four transverse communicating branches arising from the digital arteries enter the flexor tendon sheath through openings in the pulleys, traveling toward the vincula. The sites of entry are at the base of the proximal phalanx, the neck of the proximal phalanx, the base of the middle phalanx, and the neck of the middle phalanx (Figure 1-5).
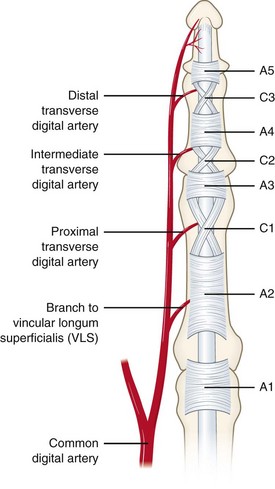
Figure 1-5 The tendon sheath contains the annular pulleys A1 to A5 and the cruciate pulleys C1 to C3.
Two kinds of vincula were found within each digital flexor tendon sheath: vessels arising from the transverse communicating arteries protrude through the mesotenon forming short, triangle-shaped folds (vincula brevia) and long, slender vincula longa (Figure 1-6).