Adjunctive Procedures for Rejuvenation
Samuel M. Lam
Edwin F. Williams III
Rejuvenative surgery for the face has undergone nothing short of a revolution this past decade, from minimally invasive brow techniques to diverse approaches to the midface. The trend in surgical technique has been toward less invasive strategies that facilitate faster recovery. As part of this Zeitgeist, adjunctive procedures have risen to the forefront in the rejuvenative armamentarium to respond to the demand for quick fixes. Younger patients, who do not require extensive surgical intervention, are seeking prophylactic treatments (e.g., botulinum toxin) and minor improvements with soft-tissue injectables and solid fillers. Adjunctive therapies work equally well in more mature patients as part of a global strategy for rejuvenation. Technological triumphs have kept pace with public demand, and a myriad array of soft-tissue replacement products are under investigation or have entered the market.
Unfortunately, no ideal treatment material or method exists today; that is, biocompatible, natural, permanent, and yet removable. This quandary is the crux of the problem. An alloplast must be stable and well integrated for perpetuity, yet be pliable and natural to palpation and examination, and be easily removable in the event of rejection or infection. Solid fillers may have a firm texture that is intolerable to some patients and may have a higher extrusion or infection rate. Injectable agents may achieve a more natural feel but should be temporary in nature so that they will disappear should infection or other deleterious outcome manifest. Permanent injectables (e.g., Artecoll, Bioplastique, and Dermalive) not currently approved in the United States, have been reported to engender granulomatous reaction several years after implantation and may be only partially extracted with mutilating surgical excision.1, 2 and 3 Appropriately chosen materials and properly performed procedures ensure patient satisfaction and optimal aesthetic benefit.
PREOPERATIVE CONSIDERATIONS: PATIENT SELECTION AND RELEVANT ANATOMY
Perhaps the first order of business for any patient who presents to the facial plastic surgeon for consultation is what that patient desires corrected. Besides the aesthetic deficit that the patient perceives, the surgeon usually should promptly establish whether the patient intends to undergo larger flap-type surgery or envisions only a more limited “adjunctive” procedure with less recovery time. Astute attention to the patient’s inclination toward less or more surgery facilitates good rapport and ensures a mutual strategy for success. A patient’s demeanor and comments may serve as invaluable clues to the surgeon as to the patient’s true intentions and objectives. Furthermore, the patient may express hesitation as to whether a certain “look” would be ultimately attractive for him or her and request a temporary measure that can approximate a permanent solution. For instance, botulinum toxin (BTX) may act as a useful agent to demonstrate to the patient the benefit of a potential browlift in the future. Alternatively, collagen may act as a reliable indicator as to how the nasolabial fold would appear with a permanent solid filler (e.g., expanded polytetrafluoroethylene [ePTFE] or acellular dermis). The age of the patient also guides the surgeon as to what recommendations to make: A younger patient may not require or desire invasive surgical intervention, making a limited surgical or dermatological procedure more appropriate.
This section on preoperative considerations is divided according to particular zones of the face that would benefit from an adjunctive-type procedure (e.g., the glabellar frown lines; the lateral-canthal crow’s feet; the nasolabial smile lines and marionette labiomandibular lines; thin, hypoplastic lips; and perioral rhagades). By classifying anatomic deficiencies in this manner, the surgeon can evaluate a particular patient complaint and work through the exercise of the modality that is most applicable in a certain situation. The following section on intraoperative considerations elaborates on each method of rejuvenation in a detailed and stepwise fashion.
Generally, a reasonable treatment strategy for adjunctive procedures divides the face into two vertical portions with an imaginary horizontal line drawn through the bottom of the nose (Fig. 8-1). Botulinum toxin therapy is particularly well suited for early wrinkles present in animation above this line, but may be less appropriate for wrinkles below this line.
Perioral BTX therapy for an overactive depressor offers limited benefit with the attendant risk of oral incompetence. However, soft-tissue augmentation is effective below this horizontal line but less so above it. A fundamental difference in wrinkle quality above versus below this line explains the authors’ rationale for this strategy. Wrinkle lines that form above this line are generally etched-in lines from repeated motion and benefit from either BTX therapy early (incipient lines) or resurfacing later (mature lines). Deeper glabellar lines also may be appropriately excised if very advanced. Solid or liquid soft-tissue augmentation in the periocular region cannot readily and evenly efface the fine etched-in lines in this region. Although the glabella tolerates this type of augmentation, liquid fillers are contraindicated because of skin necrosis and retrograde thrombosis and blindness;4 and solid augmentation may not be the best modality to treat this area. (Consider either resurfacing or excision as better alternatives.) Nevertheless, solid soft-tissue augmentation has been successful for those patients willing to tolerate some palpability in this area.
Perioral BTX therapy for an overactive depressor offers limited benefit with the attendant risk of oral incompetence. However, soft-tissue augmentation is effective below this horizontal line but less so above it. A fundamental difference in wrinkle quality above versus below this line explains the authors’ rationale for this strategy. Wrinkle lines that form above this line are generally etched-in lines from repeated motion and benefit from either BTX therapy early (incipient lines) or resurfacing later (mature lines). Deeper glabellar lines also may be appropriately excised if very advanced. Solid or liquid soft-tissue augmentation in the periocular region cannot readily and evenly efface the fine etched-in lines in this region. Although the glabella tolerates this type of augmentation, liquid fillers are contraindicated because of skin necrosis and retrograde thrombosis and blindness;4 and solid augmentation may not be the best modality to treat this area. (Consider either resurfacing or excision as better alternatives.) Nevertheless, solid soft-tissue augmentation has been successful for those patients willing to tolerate some palpability in this area.
Below this horizontal axis, the lines that develop usually do so because of gravitational ptosis (e.g., the nasolabial and labiomandibular folds). These folds, rather than wrinkles, are more amenable to soft-tissue augmentation with either liquid or solid fillers rather than BTX therapy. The one exception to this rule is the perioral rhagades, or smoker’s lines. These fine crevices around the mouth are more akin to the fine lines that circumscribe the eye. Therefore, solid or liquid augmentation of these lines is not very effective. Unlike the periocular rhytids, however, the perioral rhagades are not as amenable to BTX (which may be an apparent caveat) but should be treated with laser ablation or dermabrasion. Hypoplastic lips, on the other hand, may be appropriately treated with soft-tissue augmentation materials like the other areas described below this horizontal axis.
Glabellar Frown Lines
As a review of basic anatomy, the vertical rhytidosis that forms in the glabellar region may be attributed to the overactivity of the horizontally aligned corrugator supercilii musculature. The horizontal rhytids, usually situated somewhat lower, arise from repeated motion of the procerus muscle. These furrows that form may either be present at rest and in motion or only in motion: This consideration largely determines which intervention is most suitable for a particular patient. The deep glabellar lines engender two aesthetically unattractive features: (a) glabellar creases themselves connote to the observer a sign of aging; and (b) deeper furrows may impart the impression of an angry, worried, or tired visage that may belie the patient’s true emotional disposition.
The medial-brow complex is a recalcitrant area to browsuspension surgery (Chapter 4). Meticulous dissection of the medial-brow complex during brow surgery can lead to many undesirable complications (e.g., uneven contour deformity, return of function, inability to reduce established glabellar rhytidosis, and worse yet frank cutaneous necrosis). For all these reasons, the medial-brow region is more amenable to localized adjunctive therapy.
Younger patients with rhytidosis limited only to animation or those who have incipient rhytidosis are best treated with BTX. Unfortunately, this procedure is only temporary and can be expensive with repeated treatment sessions. However, BTX injection is the best and only therapy that is recommended for early rhytidosis.
With glabellar rhytidosis that is present both at rest and in motion, more aggressive therapy may be warranted. Early, incipient rhytids may be treated with BTX as a first step to see whether the formed line will soften over time owing to muscle inactivity. Alternatively, if the patient has other dyschromias or signs of photodamage, a Jessner’s/35% trichloroacetic acid (TCA) peel may efface limited rhytidosis (Chapter 9).
More severe rhytidosis requires carbon dioxide laser ablation in this area. As discussed in Chapter 9, full-face laser therapy may be followed by a protracted recovery time that is insufferable to many patients. Therefore, a chemical peel may be done elsewhere on the face with a targeted laser ablation of the glabella to achieve a more uniform resurfacing if
more global photodamage would cause treatment with laser alone in the glabella to appear discontinuous with the adjacent unresurfaced skin. Other temporary soft-tissue augmentation materials (e.g., collagen) have been associated with skin necrosis and retrograde retinal thrombosis and consequent blindness and are contraindicated in the glabella.
more global photodamage would cause treatment with laser alone in the glabella to appear discontinuous with the adjacent unresurfaced skin. Other temporary soft-tissue augmentation materials (e.g., collagen) have been associated with skin necrosis and retrograde retinal thrombosis and consequent blindness and are contraindicated in the glabella.
Besides laser ablation for deeper wrinkles, solid soft-tissue fillers (e.g., ePTFE or acellular dermis) may provide benefit for the patient and be well tolerated in the thicker glabellar skin. However, as with all solid fillers, the patient must understand the limitations of such augmentation (e.g., palpability, possible mobility and migration, potential visibility, and some risk of extrusion and infection). Given these limitations, a well-established and proven method of rejuvenation of the glabella is direct excision of the rhytid, attenuation of the underlying muscle, reconstruction with a geometric broken-line repair, and possible delayed dermabrasion. (See the following section for a detailed description.) Surgical excision of the rhytid should be reserved only for corrugator-derived vertical rhytids and not the procerus-related horizontal rhytids. The latter rhytids tend to be shallower in depth and do not tolerate this type of surgical technique. Albeit ostensibly aggressive, this technique has stood the test of time and proved valuable in the surgical armamentarium. However, this modality is not necessarily appropriate in other facial areas; for example, excision of the nasolabial fold appears uniformly poor and is not recommended, as the scar ineluctably widens with repeated movement.
Lateral-Canthal Crow’s Feet
Similar to glabellar frown lines, the presence of lateral-canthal crow’s feet should be classified as lines present at rest and motion versus motion only. The latter condition is amenable to BTX therapy to abort the development of the former problem (i.e., so that the animated lines do not become permanently etched-in lines). Botulinum toxin must be continued indefinitely to ensure that the development of more permanent rhytids do not arise. The notion that the muscles become progressively more attenuated and eventually do not require BTX is a fallacy that has been proved with histological evidence. Nevertheless, patients often report that they “unlearn” certain behaviors that caused the wrinkles in the first place after many months and years of muscular inactivity, thus perpetuating the longevity of BTX.
Another preventative measure that can abort incipient lines and minimize the development of further rhytidosis is the newer technique of nonablative therapy (Chapter 9). Various laser and light devices have been used for nonablative therapy, including the pulsed-dye laser, the Q-switched 1064-nm Nd:YAG laser, 980-nm diode laser, 1320-nm Nd:YAG laser, Erbium:Glass laser, Erbium:YAG laser, and intense pulsed light. Nonablative therapy, which has no discernible downtime (no ecchymosis, erythema, or edema if the parameters are properly adjusted), works by stimulating the underlying dermal collagen that can in turn even out the overlying epidermis. However, nonablative therapy only effectively treats fine and early periocular wrinkles and has limited benefit for deeper, perioral rhagades. The patient in his or her thirties who is a good candidate for BTX therapy may be equally well suited for nonablative laser therapy, which can be combined with BTX treatment. The results after a 3- to 6-month period can be outstanding if a patient understands the limitations of this technology.
More established, etched-in lines should be treated instead with an ablative resurfacing modality. Other than actual redundant skin that requires a blepharoplasty, the surgeon should be attentive to fine lower and lateral eyelid wrinkles that should be addressed with a chosen resurfacing technique. Excising skin when only rhytidosis is present can lead to vertical shortening of the lower lid and malpositioning. Fine wrinkles can be treated quite effectively with a Jessner’s/35% TCA peel, whereas deeper wrinkles may benefit from CO2-laser ablation (if the patient is willing to accept the longer recovery period).
The Nasolabial Smile Lines and the Labiomandibular Marionette Lines
As mentioned, the nasolabial and labiomandibular folds are poorly treated with BTX therapy, because these lines represent actual ptosis of tissue rather than wrinkles in animation. Instead, these lines can be augmented with a soft-tissue filler, whether a temporary liquid injectable or a more permanent solid material, to soften these ptotic folds. The patient should be fully cognizant of the limitations in completely effacing these lines and understand that limited improvement is the goal and not the exception. In addition, the patient should realize that a liquid filler (e.g., collagen) is only temporary and that a permanent filler (e.g., ePTFE) may at times be both palpable and visible and may risk extrusion and infection. Furthermore, if this anatomic area is the primary focus of grievance, then the patient should understand that a facelift, whether deep plane or superficial musculoaponeurotic system (SMAS), will do little to improve this line and may actually worsen it on occasion.
If the patient is willing to accept these limitations, then the surgeon can reasonably discuss the possible types of favorable treatment options. Although hyaluronic acid (Restylane) has shown promising aesthetic benefit and longevity abroad, this liquid injectable material has not yet been approved for use in the United States. Although hyaluronic acid should be free of antigenicity (i.e., no skin test is required), the major adverse reaction that has been reported worldwide, albeit on a small scale, is hypersensitivity (0.06% to 0.15%).5, 6 and 7 At this time, bovine collagen remains a mainstay of temporary liquid augmentation. The authors have the greatest experience with Zyplast, which has greater longevity than Zyderm, and is favored by the authors as the
only type of collagen for lower facial rejuvenation. As mentioned, the authors do not support the use of collagen, or equivalent augmentation material, in the upper face or periorbital region. Therefore, Zyplast has served well as the only type of collagen needed. Other liquid implants (e.g., Cymetra, Dermalogen, Isologen) can be expensive or temporary and have not been reliably used in the authors’ experience. As a practical matter, stocking only one liquid injectable eases the burden of inventory and reduces confusion for the patient and surgeon alike.
only type of collagen for lower facial rejuvenation. As mentioned, the authors do not support the use of collagen, or equivalent augmentation material, in the upper face or periorbital region. Therefore, Zyplast has served well as the only type of collagen needed. Other liquid implants (e.g., Cymetra, Dermalogen, Isologen) can be expensive or temporary and have not been reliably used in the authors’ experience. As a practical matter, stocking only one liquid injectable eases the burden of inventory and reduces confusion for the patient and surgeon alike.
If the patient elects to have a permanent soft-tissue filler, then ePTFE may be the most suitable option. Expanded polytetrafluoroethylene comes in many brands, each touting a theoretic advantage based on porosity and pliability. However, in the authors’ experience with these different implants, these considerations remain squarely within the realm of theory and carry very little practical import. As mentioned, the limitations that concern this type of implant are palpability (particularly when smiling or during extreme animation of the lower face), and possible visibility, migration, extrusion, and infection. These latter three complications are relatively rare and can be managed by simple excision and removal of the implant if need be. Women tend to tolerate the issue of palpability much better than men, as is generally true for most cosmetic endeavors.
Alternatively, acellular dermis may prove to be a favorable compromise between a permanent substance such as ePTFE and a temporary liquid injectable such as collagen. Although touted as permanent, the authors have found that acellular dermis is semipermanent to permanent, depending on the patient’s biophysiologic ability to degrade the foreign material. The benefit of acellular dermis is that usually the substance lasts considerably longer than collagen and is not as palpable (if at all) compared with Gore-Tex (W.L. Gore and Associates, Inc., Flagstaff, AZ) or another type of ePTFE. However, the degree of augmentation may be somewhat less than what may be achievable with ePTFE. The patient should be educated as to the derivation of acellular dermis (e.g., processed cadaveric dermis) and should understand the rigorous screening and mechanical process through which the materials have been subjected. Based on these advantages and drawbacks, the surgeon and patient can then arrive at a mutually agreed on, suitable modality.
Although not truly applicable in this chapter dedicated to “adjunctive” therapies, the nasolabial and labiomandibular folds also may be softened with SMAS excised during an SMAS-imbrication rhytidectomy. If the patient consents for this treatment option, he or she may have the best of all possibilities: an autogenous, pliable material that should not be readily palpable and have an enduring quality. In addition, the risk of extrusion and infection is almost unheard of given the autogenous nature of the implant. The implant also does not cost any extra in terms of harvesting time, donor-site morbidity, or purchase cost. Therefore, the perfect candidate for this procedure is the individual who is undergoing a concurrent rhytidectomy and who exhibits notable marionette, or labiomandibular, folds.
Perioral Rhagades or Smoker’s Lines
Perioral rhagades, or smoker’s lines, are best treated with a resurfacing modality (Chapter 9). However, treatment of this pathology is mentioned again in this chapter for sake of completeness and to caution the reader about the use of soft-tissue augmentation or BTX to address this entity. These deeply etched lines can be effectively treated only with laser therapy or dermabrasion and attain limited improvement with a TCA peel. Phenol, which is not covered in this book, is a viable alternative. Soft-tissue augmentation with collagen, equivalent filler, or solid implant does very little to address these wrinkles and is not advisable.
Thin, Hypoplastic Lips
Full, pouty lips are an emblem of sensuality, and thin, attenuated lips signify aging and reduced sexual allure. Many young women who are born with congenitally thin lips seek to amplify their lip volume even at a relatively tender age. More mature women suffer from a longer white lip, reduced vermilion height, and less pronounced Cupid’s bow. Treatment of hypoplastic lips may be divided into two principal strategies: soft-tissue augmentation and advancement cheiloplasty.
As described, soft-tissue augmentation may be effected with either temporary liquid injectables (e.g., collagen) or more permanent materials (e.g., acellular dermis or ePTFE). The patient must weigh the benefits and drawbacks (already explained) to decide what is most appropriate for that individual. However, the authors emphasize that Gore-Tex, or any kind of ePTFE, may not be the most suitable choice for lip augmentation. Unlike the nasolabial fold, the lip is subjected to much more movement and is more proximal to the contaminated oral cavity. For these two reasons, the incidence of infection with lip augmentation tends to be much higher than with nasolabial-fold augmentation, especially with ePTFE. However, acellular dermis has been noted to be much less prone to extrusion and infection and less palpable than ePTFE. Therefore, acellular dermis may be a reasonable alternative for semipermanent to permanent lip augmentation. These conclusions have been arrived at after many years of trial and error and represent empiric observation rather than a controlled study protocol.
Advancement cheiloplasty, or lip advancement, should be discouraged, because it often creates an unnatural result, particularly in the younger patient who requires little additional augmentation. Even in the best surgical hands, the risk of an unnatural outcome may be significant. This treatment modality should be reserved for women who are more advanced
in age and fully comprehend the limitations of this technique. Even more important, these ladies must be willing to wear lipstick as a camouflaging agent on a routine basis. If the patient does not meet these selective, exclusion factors, then the surgeon should resist the temptation to operate.
in age and fully comprehend the limitations of this technique. Even more important, these ladies must be willing to wear lipstick as a camouflaging agent on a routine basis. If the patient does not meet these selective, exclusion factors, then the surgeon should resist the temptation to operate.
INTRAOPERATIVE CONSIDERATIONS: TECHNIQUE AND SALIENT TECHNICAL POINTS
Expanded Polytetrafluoroethylene Acellular Dermis (Nasolabial Fold, Labiomandibular Fold)
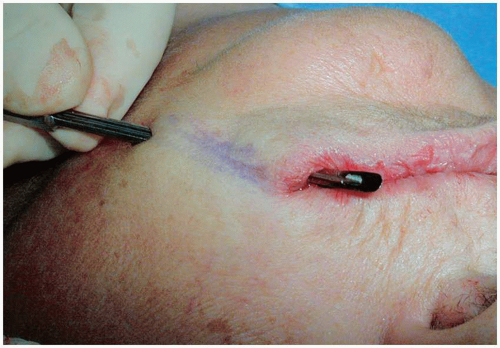
Besides the preparation of acellular dermis or harvesting of SMAS, the actual procedure of insertion for acellular dermis, ePTFE, or SMAS are identical and discussed herein as one procedure (Fig. 8-2). Acellular dermis, ePTFE, and SMAS tissue are henceforth referred to collectively as the implant. This procedure can be undertaken with local anesthesia alone (1% lidocaine with 1:100,000 epinephrine) or some Versed sedation depending on the patient’s disposition and temperament. Clearly, SMAS insertion implies a full rhytidectomy has been performed concurrently, and the reader is directed to Chapter 5 for further details concerning SMAS harvesting and implantation during rhytidectomy. For details of acellular-dermal preparation, the reader is referred to the following section that describes acellular-dermal implantation for lip augmentation. The amount of acellular dermis that is required for labiomandibular, nasolabial, and lip augmentation is also discussed in the following section and summarized in Table 8-1. The preferred type of ePTFE is fibrillar in nature. A 1-mm size is used for a shallower groove and 2-mm for a deeper groove.
For the nasolabial fold, a stab incision is made with a Bard-Parker No. 15C or No. 11 blade parallel and within the crease of the nasolabial fold about 5 mm away from the alar-facial groove and another stab incision is made at the lowest extent of the nasolabial fold. For the labiomandibular fold, the stab incision is made at the inferior extent of the fold (Fig. 8-3B) and inside the buccal mucosa that parallels the fold (Fig. 8-4). Starting from the inferior incision, a standard passer, or introducer, device is used to tunnel in the subcutaneous plane along the fold toward the distal incision (Fig. 8-5A,B). The nondominant hand should guide and control the tunneling of the instrument. Furthermore, the tunnel should be made just large enough to accommodate the implant. For the nasolabial fold, the surgeon should create the tunnel along the nasolabial fold crease, erring slightly medially rather than laterally. Because the nasolabial fold is defined as a mound laterally and a valley medially, the surgeon should place the implant medially to raise the depression and soften the transition between the two elevations.
After the tunnel has been successfully created, one end of the implant is securely fastened to a 0-silk on a Keith-style needle about 0.5 to 1 cm from the end of the implant to avoid slippage of the suture off the implant.** The needle is then passed into the groove of the introducer (Fig. 8-6), and then the introducer is withdrawn leaving the needle in place. The wound edges of one stab incision are retracted laterally and upward with opposing tiny, double hooks. Expanded polytetrafluoroethylene, which has a higher likelihood of implant infection, does not require any preparatory soak in povidone-iodine, or equivalent solution, as the material is hydrophobic and does not benefit from immersion in a disinfectant. The implant is gently pulled through the tunnel until it fully occupies the space (Fig. 8-7). The nondominant hand again should guide the implant so that it does not kink or fold onto itself during insertion.
The length of the implant should be at least 1 cm longer than the tunneled pocket so that the ends may be tucked further distal to both incisions by 2 to 3 mm (Fig. 8-8). For the side of the implant that passes into the buccal mucosa, a more conservative amount should be visible (i.e., less than 5 mm rather than 1 cm in length) (Fig. 8-9). The portion of the implant fastened to the 0-silk suture is amputated and discarded. As mentioned, the distal aspects of the implant then are tucked distal to the incision on both ends, using a tiny double hook and Bishop forceps to facilitate ease of entry and placement. The rationale for the extension of the implant past the incision site is several-fold. First, if the implant terminates at the incision site, a tendency may arise for the wound to contract downward over a void: The implant buttresses against this possibility. Second, if the end of the implant buckles somewhat over time, it may tend to apply pressure against the wound edge and have a greater likelihood for extrusion. Third, the implant may tend to contract over time so the implant is placed as distally as possible to protect against this event. The incisions then are closed using 6-0 polypropylene in a simple, interrupted fashion with two to three sutures placed for each incision site, as determined by wound length (Fig. 8-10). These sutures are removed at 1 week.
As mentioned, the authors believe that for semipermanent to permanent lip augmentation, acellular dermis is the preferred method because of the safety profile of the material and the ultimate natural look and feel. Although a fuller lower lip has sensuous appeal, most patients have a more attenuated upper lip and also generally derive greater satisfaction
with augmentation of the upper lip (Fig. 8-11). Accordingly, often patients desire only selective augmentation of the upper lip. However, simultaneous upper- and lower-lip augmentation remains a more common request.
with augmentation of the upper lip (Fig. 8-11). Accordingly, often patients desire only selective augmentation of the upper lip. However, simultaneous upper- and lower-lip augmentation remains a more common request.
Instrumentation and Equipment
Instrumentation and Equipment for Acellular Dermis and Expanded Polytetrafluoroethylene Augmentation
Prep Stand:
Nonsterile gloves
10-cc syringe (2), 27-gauge (11/4-inch long) needle (2) with lidocaine 1% and 1:100,000 epinephrine
Surgical marking pen
Instruments:
Introducer, also known as a Passer—a device that resembles a Freer but has a sharper edge as well as a central groove that accommodates a needle used to draw the implant through the pocket.
Hemostat (to grasp the free end of the implant so as to prevent pulling the implant accidentally too far into the pocket).
Tiny, double-hooks (2)
Metzenbaum or Mayo scissors
Sutures:
0-silk with a 60-mm Keith-type KS (SC2, CS-1) [SC2]<SE-1>* needle (to suture the implant)
6-0 polypropylene, P-3 (P-13, PRE-2) needle (to close the skin incision)
5-0 chromic, P-3 (PRE-2, P-13) <RE-3> needle (to close the lip incision)
Other Supplies:
No. 11 or 15c blade
Acellular-dermal graft, 3  7 cm graft (Table 8-1)
7 cm graft (Table 8-1)
 7 cm graft (Table 8-1)
7 cm graft (Table 8-1)ePTFE, Fibrillar Form (1-mm size for a more superficial depression and 2-mm for a deeper groove)
Instrumentation/Equipment for Advancement Cheiloplasty
Prep Stand:
Nonsterile gloves
10-cc syringe (2), 27-gauge (11/4-inch long) needle (2) with lidocaine 1% and 1:100,000 epinephrine
Surgical marking pen
Castroviejo calipers
Instruments:
Tiny, double-hooks (2)
Bishop forceps
Sutures:
6-0 silk, P-1(P-10, PRE-1) [C1] <EDR-1> needle
Other Supplies:
No. 15 blade
Instrumentation/Equipment for Geometric Broken-Line Repair for Deep, Vertical Glabellar Rhytidosis
Prep Stand:
Nonsterile gloves
10-cc syringe (2), 27-gauge (11/4-inch long) needle (2) with lidocaine 1% and 1:100,000 epinephrine
Surgical marking pen
Castroviejo calipers
Instruments:
Wide double hooks
Tiny double hooks
Dissecting (iris or tenotomy) scissors
Sutures:
4-0 polydioxanone, PS-3 (P-11, PRE-3) [PC-34] needle
6-0 fast-absorbing suture, PC1 (PC-13, SBE-2) <BLE1> needle
Other Supplies:
No. 11 blade
Bipolar cautery
Wire brush dermabrader (at additional session 6 weeks later if necessary for maximal scar camouflage)
Instrumentation and Equipment for Botulinum-Toxin Injection
Reconstitution (Recommended Dilution):
4.5 cc preservative-free saline
18-gauge needle
5-cc syringe
Injection:
30-gauge, 1/2″ needle
1-cc tuberculin syringe
Instrumentation and Equipment for Collagen Injection
Collagen Test Patch
Zyplast 1.5 cc. Recommended for most augmentation purposes.
Zyplast 1.0 cc. Recommended for conservative lip augmentation in the younger patient.
30-gauge needle or special injection needle (both come supplied with the Collagen kit). The specialized needle permits reducing the length of the exposed tip to control depth of the injection.
 FIGURE 8-2. (Continued) E-F. The patient is shown with good aesthetic improvement 6 months after augmentation. |
 FIGURE 8-7. ePTFE Smile-Line Insertion, Step 5. The needle is then pulled through until the implant has been positioned into the pocket with a 1-cm tail of the implant left exposed. |
 FIGURE 8-8. ePTFE Smile-Line Insertion, Step 6. The exposed 1-cm tail of the implant is then tucked further distal to the incision site using fine-toothed forceps and tiny, double-hook retractors. |
One percent lidocaine and 1:100,000 epinephrine is infiltrated into the upper lip, and 10 minutes are allowed to transpire, during which time the acellular dermis is properly prepared (Fig. 8-12). Typically, a 3-  7-cm acellular-dermal graft is sufficient to augment both the upper and lower lips in a conservative fashion. Two thirds of this graft is sectioned lengthwise (i.e., along the long axis of the graft), to be used for the upper lip, and the remaining one third is reserved for the lower lip. This amount of augmentation is particularly well suited for a more mature woman who desires subtle but definitive augmentation. As acellular dermis comes in different thicknesses, the thickest 3-
7-cm acellular-dermal graft is sufficient to augment both the upper and lower lips in a conservative fashion. Two thirds of this graft is sectioned lengthwise (i.e., along the long axis of the graft), to be used for the upper lip, and the remaining one third is reserved for the lower lip. This amount of augmentation is particularly well suited for a more mature woman who desires subtle but definitive augmentation. As acellular dermis comes in different thicknesses, the thickest 3-  7-cm sheet should be ordered to achieve maximal augmentation. Use of two 3-
7-cm sheet should be ordered to achieve maximal augmentation. Use of two 3-  7-cm grafts for lip augmentation (i.e., one for the upper lip and one for the lower) is an aggressive augmentation that may risk extrusion and also increase the period of postoperative edema. Nevertheless, this amount of augmentation can be used for the more outspoken patient who demands significant increase in lip volume. Given the expense of acellular dermis, routine use of two sheets may not be financially justifiable except for the vocal patient who insists on considerable lip augmentation. If the patient desires only selective augmentation of the upper lip, then usually the entire 3-
7-cm grafts for lip augmentation (i.e., one for the upper lip and one for the lower) is an aggressive augmentation that may risk extrusion and also increase the period of postoperative edema. Nevertheless, this amount of augmentation can be used for the more outspoken patient who demands significant increase in lip volume. Given the expense of acellular dermis, routine use of two sheets may not be financially justifiable except for the vocal patient who insists on considerable lip augmentation. If the patient desires only selective augmentation of the upper lip, then usually the entire 3-  7-cm graft is placed into the upper lip so that none
7-cm graft is placed into the upper lip so that none
is wasted. However, if the lip appears too full after this degree of augmentation, a more conservative amount can be used as aesthetically demanded. For nasolabial augmentation, one half of the 3- 7-cm graft is inserted into each smile line. Similarly, one half of the 3-
7-cm graft is inserted into each smile line. Similarly, one half of the 3-  7-cm graft is inserted into each marionette line. Table 8-1 summarizes these recommendations. The acellular dermis is rolled and sutured with a 5-0 chromic suture (Fig. 8-13) and tied at one end to the 0-silk, which in turn is affixed to the straight needle that is designed to fit into the groove of the introducer (Fig. 8-14). It is imperative that the 0-silk suture be firmly tied to the end of the implant using a square knot, because it may easily slip off the end of the implant during the forceful draw through the pocket. Stab incisions are made with a No. 15 blade approximately at the junction of the wet and dry lip on either end of the upper lip about 4 to 5 mm medial to the oral commissure (Fig. 8-15). The introducer is then passed through the upper lip using the nondominant hand to guide the device toward the other side (Fig. 8-16A-C). The proper plane of passage is below the outer mucosa but above the orbicularis-oris muscle. The instrument should be advanced slowly and deliberately in order to avoid inadvertent puncture through the outer lip with control provided by the nondominant hand. The straight needle is then passed into the groove of the introducer and pulled through as the introducer is withdrawn (Fig. 8-17A,B). Before the implant is drawn through, the free end of the implant (i.e., the end without the attached suture) should be clamped with a hemostat to prevent the implant from being pulled too far into the pocket. The straight needle is drawn through until the implant is situated properly in the pocket with only a short 1-cm tail showing on the proximal side (Fig. 8-18). When properly situated, the suture is cut free from the implant, and the hemostat clamp removed. The distal end is trimmed to the same 1-cm length tail. The acellular-dermal graft is then tucked further distal to each incision using fine-toothed forceps with tiny, double-pronged hooks for retraction (Fig. 8-19). The incisions are closed with two interrupted 4-0 chromic sutures (Fig. 8-20).
7-cm graft is inserted into each marionette line. Table 8-1 summarizes these recommendations. The acellular dermis is rolled and sutured with a 5-0 chromic suture (Fig. 8-13) and tied at one end to the 0-silk, which in turn is affixed to the straight needle that is designed to fit into the groove of the introducer (Fig. 8-14). It is imperative that the 0-silk suture be firmly tied to the end of the implant using a square knot, because it may easily slip off the end of the implant during the forceful draw through the pocket. Stab incisions are made with a No. 15 blade approximately at the junction of the wet and dry lip on either end of the upper lip about 4 to 5 mm medial to the oral commissure (Fig. 8-15). The introducer is then passed through the upper lip using the nondominant hand to guide the device toward the other side (Fig. 8-16A-C). The proper plane of passage is below the outer mucosa but above the orbicularis-oris muscle. The instrument should be advanced slowly and deliberately in order to avoid inadvertent puncture through the outer lip with control provided by the nondominant hand. The straight needle is then passed into the groove of the introducer and pulled through as the introducer is withdrawn (Fig. 8-17A,B). Before the implant is drawn through, the free end of the implant (i.e., the end without the attached suture) should be clamped with a hemostat to prevent the implant from being pulled too far into the pocket. The straight needle is drawn through until the implant is situated properly in the pocket with only a short 1-cm tail showing on the proximal side (Fig. 8-18). When properly situated, the suture is cut free from the implant, and the hemostat clamp removed. The distal end is trimmed to the same 1-cm length tail. The acellular-dermal graft is then tucked further distal to each incision using fine-toothed forceps with tiny, double-pronged hooks for retraction (Fig. 8-19). The incisions are closed with two interrupted 4-0 chromic sutures (Fig. 8-20).
 7-cm acellular-dermal graft is sufficient to augment both the upper and lower lips in a conservative fashion. Two thirds of this graft is sectioned lengthwise (i.e., along the long axis of the graft), to be used for the upper lip, and the remaining one third is reserved for the lower lip. This amount of augmentation is particularly well suited for a more mature woman who desires subtle but definitive augmentation. As acellular dermis comes in different thicknesses, the thickest 3-
7-cm acellular-dermal graft is sufficient to augment both the upper and lower lips in a conservative fashion. Two thirds of this graft is sectioned lengthwise (i.e., along the long axis of the graft), to be used for the upper lip, and the remaining one third is reserved for the lower lip. This amount of augmentation is particularly well suited for a more mature woman who desires subtle but definitive augmentation. As acellular dermis comes in different thicknesses, the thickest 3-  7-cm sheet should be ordered to achieve maximal augmentation. Use of two 3-
7-cm sheet should be ordered to achieve maximal augmentation. Use of two 3-  7-cm grafts for lip augmentation (i.e., one for the upper lip and one for the lower) is an aggressive augmentation that may risk extrusion and also increase the period of postoperative edema. Nevertheless, this amount of augmentation can be used for the more outspoken patient who demands significant increase in lip volume. Given the expense of acellular dermis, routine use of two sheets may not be financially justifiable except for the vocal patient who insists on considerable lip augmentation. If the patient desires only selective augmentation of the upper lip, then usually the entire 3-
7-cm grafts for lip augmentation (i.e., one for the upper lip and one for the lower) is an aggressive augmentation that may risk extrusion and also increase the period of postoperative edema. Nevertheless, this amount of augmentation can be used for the more outspoken patient who demands significant increase in lip volume. Given the expense of acellular dermis, routine use of two sheets may not be financially justifiable except for the vocal patient who insists on considerable lip augmentation. If the patient desires only selective augmentation of the upper lip, then usually the entire 3-  7-cm graft is placed into the upper lip so that none
7-cm graft is placed into the upper lip so that none is wasted. However, if the lip appears too full after this degree of augmentation, a more conservative amount can be used as aesthetically demanded. For nasolabial augmentation, one half of the 3-
 7-cm graft is inserted into each smile line. Similarly, one half of the 3-
7-cm graft is inserted into each smile line. Similarly, one half of the 3-  7-cm graft is inserted into each marionette line. Table 8-1 summarizes these recommendations. The acellular dermis is rolled and sutured with a 5-0 chromic suture (Fig. 8-13) and tied at one end to the 0-silk, which in turn is affixed to the straight needle that is designed to fit into the groove of the introducer (Fig. 8-14). It is imperative that the 0-silk suture be firmly tied to the end of the implant using a square knot, because it may easily slip off the end of the implant during the forceful draw through the pocket. Stab incisions are made with a No. 15 blade approximately at the junction of the wet and dry lip on either end of the upper lip about 4 to 5 mm medial to the oral commissure (Fig. 8-15). The introducer is then passed through the upper lip using the nondominant hand to guide the device toward the other side (Fig. 8-16A-C). The proper plane of passage is below the outer mucosa but above the orbicularis-oris muscle. The instrument should be advanced slowly and deliberately in order to avoid inadvertent puncture through the outer lip with control provided by the nondominant hand. The straight needle is then passed into the groove of the introducer and pulled through as the introducer is withdrawn (Fig. 8-17A,B). Before the implant is drawn through, the free end of the implant (i.e., the end without the attached suture) should be clamped with a hemostat to prevent the implant from being pulled too far into the pocket. The straight needle is drawn through until the implant is situated properly in the pocket with only a short 1-cm tail showing on the proximal side (Fig. 8-18). When properly situated, the suture is cut free from the implant, and the hemostat clamp removed. The distal end is trimmed to the same 1-cm length tail. The acellular-dermal graft is then tucked further distal to each incision using fine-toothed forceps with tiny, double-pronged hooks for retraction (Fig. 8-19). The incisions are closed with two interrupted 4-0 chromic sutures (Fig. 8-20).
7-cm graft is inserted into each marionette line. Table 8-1 summarizes these recommendations. The acellular dermis is rolled and sutured with a 5-0 chromic suture (Fig. 8-13) and tied at one end to the 0-silk, which in turn is affixed to the straight needle that is designed to fit into the groove of the introducer (Fig. 8-14). It is imperative that the 0-silk suture be firmly tied to the end of the implant using a square knot, because it may easily slip off the end of the implant during the forceful draw through the pocket. Stab incisions are made with a No. 15 blade approximately at the junction of the wet and dry lip on either end of the upper lip about 4 to 5 mm medial to the oral commissure (Fig. 8-15). The introducer is then passed through the upper lip using the nondominant hand to guide the device toward the other side (Fig. 8-16A-C). The proper plane of passage is below the outer mucosa but above the orbicularis-oris muscle. The instrument should be advanced slowly and deliberately in order to avoid inadvertent puncture through the outer lip with control provided by the nondominant hand. The straight needle is then passed into the groove of the introducer and pulled through as the introducer is withdrawn (Fig. 8-17A,B). Before the implant is drawn through, the free end of the implant (i.e., the end without the attached suture) should be clamped with a hemostat to prevent the implant from being pulled too far into the pocket. The straight needle is drawn through until the implant is situated properly in the pocket with only a short 1-cm tail showing on the proximal side (Fig. 8-18). When properly situated, the suture is cut free from the implant, and the hemostat clamp removed. The distal end is trimmed to the same 1-cm length tail. The acellular-dermal graft is then tucked further distal to each incision using fine-toothed forceps with tiny, double-pronged hooks for retraction (Fig. 8-19). The incisions are closed with two interrupted 4-0 chromic sutures (Fig. 8-20). FIGURE 8-10. ePTFE Smile-Line Insertion, Step 8. The incisions are then closed with 6-0 polypropylene in a simple, interrupted fashion with two to three sutures placed for each incision |
TABLE 8-1. ACELLULAR DERMIS SIZES FOR LIP, LABIOMANDIBULAR, AND NASOLABIAL AUGMENTATION | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 FIGURE 8-11. A typical patient who exhibits a more attenuated upper lip and desires selective augmentation of the upper lip. |
 FIGURE 8-12. Acellular-Dermis Lip Augmentation, Step 1. A 3-
 7-cm sheet of acellular dermis is reconstituted with hydration according to the package instructions. The acellular dermal graft is cut lengthwise (i.e., along its long axis) into two-thirds and one-third portions, with the former designed for upper lip augmentation and the latter for the lower lip. 7-cm sheet of acellular dermis is reconstituted with hydration according to the package instructions. The acellular dermal graft is cut lengthwise (i.e., along its long axis) into two-thirds and one-third portions, with the former designed for upper lip augmentation and the latter for the lower lip.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|