An Effective Strategy for Patient Care
Edward D. Buckingham
Samuel M. Lam
Edwin F. Williams III
The previous chapter focused on business and marketing strategies that could help build and sustain a plastic surgical practice. This chapter continues that discussion but focuses on specific concerns related to patient care. Like each successive chapter, this chapter is structured according to preoperative, intraoperative, and postoperative considerations. The preoperative process is addressed first with particular attention paid to the role of the patient-care coordinator. Also as part of the preoperative evaluation, the dynamics of the consultation process are elaborated, from the preconsultation and consultation to the postconsultation period. Although some physicians staunchly defend the merits of 35-mm film, this chapter endeavors to convince the reader that digital imaging is a less costly, less labor intensive, more flexible, and more effective medium for every phase of patient care. Intraoperative discussion attempts to delineate the appropriate operating-room environment conducive to optimal patient care and to delve into other nuances that favorably affect delivery of care. Postoperative concerns include developing and maintaining patient rapport and managing the difficult patient. At the conclusion of this chapter, sample copies of all preoperative and postoperative instructions for the patient are provided as a ready reference for the reader.
PREOPERATIVE CONSIDERATIONS: EVALUATION, CONSULTATION, AND IMAGING
Role of the Patient-Care Coordinator
Often patients consider cosmetic surgery for quite some time before placing the initial call for consultation. Once this call has been made, it becomes imperative to ensure that the patient will schedule a consultation by establishing immediate rapport, by answering all queries fully but succinctly, and by engaging the patient’s interest and motivation. A welltrained patient-care coordinator can fulfill this role in a dedicated fashion. In a busy practice, the phone may be answered by a receptionist, the patient-care coordinator, or another staff member. The physician should ensure that every staff member is fully trained to answer the initial phone consultation in a professional and knowledgeable manner. Mock telephone conversations can be used to assess the level of competency of the staff in this regard: The physician or senior staff can role play as a prospective patient to ask each staff member in turn how he or she would respond in a given scenario. These sessions should be nonjudgmental in nature and be emphasized to be simply a didactic tool. Any deficiencies in telephone aptitude should be identified and critiqued for betterment of the staff. Besides the skill of salesmanship, the physician should also ensure that basic fund of knowledge concerning all products and services is upheld through formal, scheduled didactic sessions. This fundamental skill in patient dialog that all staff members should possess underscores the importance of cross training (Chapter 2); that is, the entire staff should feel comfortable with multiple office roles. A related section has been included that offers sample questions that can be used in training the staff and to stimulate discussion. Although every staff member should be well versed in answering the phone, the patient-care coordinator should make every effort to be the primary person in charge of this responsibility to provide needed continuity of care and breed a sense of familiarity when the patient arrives for the consultation. Perhaps the most effective way for this arrangement to be executed is for the receptionist to answer the majority of incoming calls and to direct potential consultations or other patient-related questions to the patient-care coordinator. Any overflow of calls should be then handled by the patient-care coordinator or other staff member in that order of priority.
The responsibility of the patient-care coordinator begins with the initial patient call. When a cosmetic call is received, the patient should be referred by name to the coordinator. It is important to reinforce the coordinator’s name to the patient in order to encourage a more durable relationship between the two parties. Once the patient has become comfortable
with the coordinator, it is more likely that meaningful dialog will ensue. After the coordinator has been relayed the telephone call, it is then his or her responsibility to transform the discussion into a consultation with the physician. Although many of the patient’s questions can and should be answered during the initial call, the goal should not be to conduct a formal telephone consultation but to exchange enough information to secure an office appointment. Additionally, the coordinator should be selling the primary product of the practice—the physician—to the patient. The coordinator should endeavor to enlighten the patient of the physician’s impeccable credentials and why the physician is best qualified to address the patient’s cosmetic concerns. Additionally, designation of one individual in the office as the primary contact for patient care opens the door for convenient, comfortable reestablishment of that contact at any time. It allows the patient who has never visited the office before to step into that environment and feel an intimate rapport through the established contact with the patient-care coordinator, a relationship that can be nurtured during every return visit. Women tend to value this relationship greatly, which can manifest as a greater likelihood to schedule surgery, return in the future, and refer friends for consultation.
with the coordinator, it is more likely that meaningful dialog will ensue. After the coordinator has been relayed the telephone call, it is then his or her responsibility to transform the discussion into a consultation with the physician. Although many of the patient’s questions can and should be answered during the initial call, the goal should not be to conduct a formal telephone consultation but to exchange enough information to secure an office appointment. Additionally, the coordinator should be selling the primary product of the practice—the physician—to the patient. The coordinator should endeavor to enlighten the patient of the physician’s impeccable credentials and why the physician is best qualified to address the patient’s cosmetic concerns. Additionally, designation of one individual in the office as the primary contact for patient care opens the door for convenient, comfortable reestablishment of that contact at any time. It allows the patient who has never visited the office before to step into that environment and feel an intimate rapport through the established contact with the patient-care coordinator, a relationship that can be nurtured during every return visit. Women tend to value this relationship greatly, which can manifest as a greater likelihood to schedule surgery, return in the future, and refer friends for consultation.
When a prospective cosmetic patient arrives for the appointment, the patient-care coordinator should greet them, explain how the visit will proceed, and assist with any preliminary paperwork. The coordinator should then escort the patient to the consultation room and begin the preconsultation process or turn that responsibility over to another designated staff member (the details of which are discussed in a following section). After the patient’s consultation with the physician, the coordinator assumes responsibility again for the patient. Initially, the physician needs to be comfortable and responsible for determining and discussing fees with the patient. However, as the coordinator gains experience and confidence, he or she is able to engage in the explanation of fee schedules and payment options (Fig. 3-1). These fees should be individualized and totaled for the patient on a personal price sheet that should be placed in the chart with a copy given to the patient. It may be a wise policy to have the patient sign and date the price sheet to acknowledge agreement to the price, payment schedule, and expiration of the quoted price after a particular date. If the patient decides to proceed with surgery, the patient-care coordinator should then schedule a date for the procedure. If the patient defers decision for surgery, the coordinator should offer both the physician and coordinator’s business cards to the patient and welcome the patient to call any time to inquire further or to return for another consultation. Within a few days the coordinator should then compose a follow-up letter thanking the patient for the visit and thereby reinforce the relationship and open communication. The authors feel that telephone calls to the patient after a consultation may be too intrusive or improperly construed as an overly assertive gesture.
Although the staff should be knowledgeable about procedures and the surgeon’s particular background and credentials, the staff should not dispense medical advice. As mentioned in the text, the objective of the telephone conversation with the patient is to answer any preliminary questions or concerns about the physician and related services and, more important, to secure a formal consultation with the physician. The person answering the phone must promote the surgeon and the practice and encourage the prospective patient that a consultation with the surgeon will be worthwhile.
The “Preconsultation”
The preconsultation provides the forum for a member of the staff with intimate knowledge of cosmetic procedures to make preliminary contact with the patient and build on the relationship initiated by the patient-care coordinator. Obviously, the most thorough knowledge that a staff member can possess of a particular procedure would be gained if that individual has already undertaken that procedure himself or herself. The best example of the success that a procedure can afford is living proof. Accordingly, the authors encourage all staff members who would like to undergo cosmetic surgery to do so at cost.
The purpose of the preconsultation session is manifold. The staff can answer some questions about the surgical process, recovery time, expectations, aesthetic objectives, or other concerns before entering the consultation room. This interaction saves valuable time for the physician and also alleviates some fear that the patient may have in addressing
these concerns with the physician. Often, the patient may feel more at ease with an individual of the same gender and age group than with the physician, who may be of a different age or sex. During the preconsultation, the patient may confess dissatisfaction with another surgeon or disdain about a type of rejuvenative procedure that can ultimately help steer the physician away from these pitfalls if he or she knows about them in advance. The staff member then may glean what is principally bothering the patient about his or her aesthetic appearance so that any pertinent information can be relayed to the physician. The preconsultation also can enlighten the patient about various surgical options over which he or she can ruminate before seeing the physician. The preconsultation session can be used to reinforce the physician’s reputation and credentials before the actual consultation. While this process is taking place, information also can be garnered regarding the patient’s expectations both financially and surgically. Invaluable information can be obtained about the patient’s financial standing that may help the physician decide what procedures would be within the patient’s budgetary constraints. The preconsultation also affords the opportunity to determine what digital “morphing” images need to be obtained and rendered before the physician speaks with the patient. Although this saves precious time during the actual consultation, the patient is informed that the physician may or may not decide to use these images based on his or her professional judgment. The preconsultation must remain relatively concise, because the consultation itself may be involved and taxing to the patient.
these concerns with the physician. Often, the patient may feel more at ease with an individual of the same gender and age group than with the physician, who may be of a different age or sex. During the preconsultation, the patient may confess dissatisfaction with another surgeon or disdain about a type of rejuvenative procedure that can ultimately help steer the physician away from these pitfalls if he or she knows about them in advance. The staff member then may glean what is principally bothering the patient about his or her aesthetic appearance so that any pertinent information can be relayed to the physician. The preconsultation also can enlighten the patient about various surgical options over which he or she can ruminate before seeing the physician. The preconsultation session can be used to reinforce the physician’s reputation and credentials before the actual consultation. While this process is taking place, information also can be garnered regarding the patient’s expectations both financially and surgically. Invaluable information can be obtained about the patient’s financial standing that may help the physician decide what procedures would be within the patient’s budgetary constraints. The preconsultation also affords the opportunity to determine what digital “morphing” images need to be obtained and rendered before the physician speaks with the patient. Although this saves precious time during the actual consultation, the patient is informed that the physician may or may not decide to use these images based on his or her professional judgment. The preconsultation must remain relatively concise, because the consultation itself may be involved and taxing to the patient.
Training Questions for the Staff
What is the cost of the procedure/procedures?
The cost of surgery is solely dependent upon the procedure/procedures being performed which is based on a realistic goal to be achieved and is determined after a consultation between Dr. X and the patient. The patient can phone the office for a convenient time to schedule a consultation.
What is the recovery period?
Usually, the recovery period is 7 to 14 days, depending on the patient and the procedure/procedures performed.
Will there be discomfort?
The level of discomfort varies depending on the patient and the procedure/procedures involved. With today’s modern anesthesia techniques, most patients experience minimal if any discomfort. Because it is our goal to achieve the maximum level of comfort for all of our patients, a prescription to relieve discomfort will be provided if necessary.
When can I exercise?
You may exercise approximately 2 days to 3 weeks afterward, depending on the procedure/procedures.
Will there by a significant difference in the way I look after surgery and will people notice?
There should be a significant improvement in your appearance, including a more youthful rested look, bearing in mind that it is our goal to provide you with an improved look based on your natural assets.
How long does the procedure/procedures last before I need surgery again?
The surgery results in an improvement ranging from approximately a few to 10+ years, depending on the procedure/procedures chosen. However, the surgery does not arrest the aging process.
How long before I can wear makeup?
You can start wearing makeup approximately 7 to 14 days after the procedure/procedures.
How much bruising and swelling will occur?
The amount of bruising and swelling depends on the patient and the procedures chosen. However, both preoperative and postoperative recommendations are given to the patient, including care performed by the nursing staff and our clinical aestheticians, that can substantially diminish the bruising and swelling.
Is the physician board certified?
Every staff member should know the surgeon’s board certification status, including when it was obtained, what the proper name of the board is, and what distinguishes that board from other related specialty board certifications. The staff also should know where the surgeon trained and in what field, any honors that the surgeon has accumulated, and other biographic details about which the patient may inquire.
Why does Dr. X perform a certain procedure?
The staff should know what kind of facelift (deep-plane, SMAS [superficial musculoaponeurotic system], etc.) the surgeon practices, and why that technique is the most beneficial for the patient. The staff member should always remember not to denigrate another surgeon’s technique, but simply sell the practice’s surgical philosophy and techniques.
What is Botox?
Botulinum toxin (Botox, Allergan, Inc., Irvine, CA) is a purified toxin that paralyzes the targeted muscles in order to prevent wrinkles in that area. It is only temporary in nature, lasting anywhere from 3 to 8 months, but typically endures for a 6-month period. There are no untoward long-term side effects; however, the procedure should be performed only by qualified physicians who are trained and experienced in its use in order to avoid short-term complications (e.g., brow or eyelid drop and asymmetry). The staff member should know all of the clinical indications for which the surgeon uses Botox (e.g., migraines, axillary hyperhidrosis, etc) and the surgeon should try to enlighten the staff about Botox pricing as well: The Botox preparation is not overly dilute, which may account for lower pricing elsewhere.
What is collagen?
Collagen is a soft-tissue filler that can enhance the fullness of one’s lips, fill in depressions such as acne scarring, and soften deep smile or marionette lines. The patient should know that a test patch is required and that he or she must wait 30 days for a negative result before augmentation can be undertaken. The staff members should know if a test patch is offered free of charge. The benefit of the collagen should be stressed as temporary in nature, lasting between 3 to 8 months, depending on the body’s resorption of the material. Also, if the patient inquires, it should be stated that collagen is derived from a bovine source; for this reason a test patch for hypersensitivity must be conducted first in the antecubital region. A formal didactic session should be carried out by the surgeon to instruct the staff members about the differences between Zyderm I, Zyderm II, and Zyplast; why the physician selects one type of collagen over another; and other related properties and clinical uses for collagen.
What kind of payment options are available?
The staff member should know what credit cards are accepted, whether cash is acceptable, how far in advance a personal check must be written before a procedure, and whether any financing is offered. Current discount or other promotional pricing should be known and extended to the patient if the surgeon has endorsed the policy. Deposits, return of deposits, and cancellation policies must be clearly understood and communicated to the patient if asked. Consultation fees, if charged, should be disclosed; also, it should be understood by every staff member whether these fees are deducted from surgery. The surgeon and office manager must ensure that current pricing is communicated to every staff member.
I am quite unhappy with the surgical result.
Any concern or dissatisfaction a patient expresses regarding a surgical outcome must be communicated to the surgeon immediately. Rather than try to handle the situation over the telephone, it is usually wise to have the patient come to the office for direct inspection by the surgeon. This tends to build rapport and ensures that any problems can be addressed promptly and accurately. In addition, as advocated elsewhere in this book, the patient’s name, nature of the complaint, and date all should be recorded in a notebook so that the surgeon can follow the patient’s progress and ensure that ongoing rapport is not lost.
I decided to cancel my consultation.
Rather than simply allow this to happen, the diligent staff member should gently seek the reason that the patient is canceling the appointment. In addition, the staff member should try to establish whether the patient could select an appropriate alternative date for consultation.
Where does Dr. X perform his or her surgery? What kind of anesthesia is offered?
The staff member should know basically where the surgeon elects to perform a procedure, whether in the office or a surgery center, but not be dogmatic in telling the patient where the surgeon is likely to do so unless obviously clear. For instance, if the surgeon typically performs lower-eyelid surgery in the office, he or she may decide to do so in an ambulatory surgery facility because of the patient’s health status or comfort level. The location and general directions to the surgical facility also should be given, and the phone number of the facility should be readily available. The type of anesthesia that is possible in the office or surgery center should be known as well (e.g., local anesthesia, intravenous sedation, monitored anesthesia care, or general anesthesia).
What can I do before or after surgery? What restrictions will there be on activity and so on before or after surgery?
Every staff member should be well acquainted with the routine preoperative and postoperative care and restrictions that are outlined in the appended forms at the end of the chapter. For instance, use of aspirin-related products, herbal medications, certain vitamins, alcohol, tobacco, and so on should be abstained from. During the preoperative phone confirmation call, the patient should be reminded to wear a button-down shirt that does not have to be pulled over the bandaged head, not to wear fingernail polish that can interfere with the pulse-oximetry reading, not to engage in heavy cardiovascular exercise the morning of surgery, and not to eat food that morning. In summary, every staff member should be well versed with the stated policies for routine preoperative and postoperative care. Any questions or concerns that cannot be readily answered should be directed to the physician. No matter what the level of medical training, the staff must understand fully that they are not medical physicians and should never offer formal, medical advice without the physician’s assent or knowledge.
The Dynamics of an Effective Consultation
Just as the goal of the initial phone contact is to book a consultation, the goal of the consultation process is to convert a
visit into a surgical case. Ideally, every consultation produces a surgical case. However, this goal is neither feasible nor realistic. Although the ambitious goal of a surgeon is to convert every consultation, the surgeon comes to realize over time that certain patients are simply not good surgical candidates, either physically or mentally. Like traditional medicine, the surgeon must establish a diagnosis and recommend appropriate surgery based on the clinical findings. However, unlike traditional medicine, the surgeon must endeavor to follow the patient’s concerns carefully without prematurely interjecting his or her own opinions. If the patient asks for the surgeon’s professional opinion, the surgeon should refrain from commentary until the patient professes an initial aesthetic complaint. For instance, if the surgeon should state that the patient’s neckline requires rejuvenation, the patient may express resentment or confusion over this advice if he or she was principally interested in rhinoplasty or brow surgery alone. Another clinical scenario may prove illustrative: If the patient asks what should be done to improve her skin, the surgeon may immediately respond that carbon dioxide laser treatment is the best option. The patient may then reply that she has already undergone laser therapy without much benefit. Instead, the surgeon should inquire a bit more about the patient’s past experiences and projected expectations before a quick reply.
visit into a surgical case. Ideally, every consultation produces a surgical case. However, this goal is neither feasible nor realistic. Although the ambitious goal of a surgeon is to convert every consultation, the surgeon comes to realize over time that certain patients are simply not good surgical candidates, either physically or mentally. Like traditional medicine, the surgeon must establish a diagnosis and recommend appropriate surgery based on the clinical findings. However, unlike traditional medicine, the surgeon must endeavor to follow the patient’s concerns carefully without prematurely interjecting his or her own opinions. If the patient asks for the surgeon’s professional opinion, the surgeon should refrain from commentary until the patient professes an initial aesthetic complaint. For instance, if the surgeon should state that the patient’s neckline requires rejuvenation, the patient may express resentment or confusion over this advice if he or she was principally interested in rhinoplasty or brow surgery alone. Another clinical scenario may prove illustrative: If the patient asks what should be done to improve her skin, the surgeon may immediately respond that carbon dioxide laser treatment is the best option. The patient may then reply that she has already undergone laser therapy without much benefit. Instead, the surgeon should inquire a bit more about the patient’s past experiences and projected expectations before a quick reply.
The primary goal of the consultation is to gather and exchange information. However, this task must be undertaken in a caring manner with the utmost caution not to offend the patient. The possibility of offending the patient and therefore losing him or her as a customer may arise because of recommending surgery too liberally or conservatively. Thoughtful attention to the patient’s desires and constant feedback are required to adjust the conversation accordingly. Once the patient’s preliminary concern is solicited (e.g., “my eyes look tired”), the surgeon should delve into the motivation and expectation that the patient has regarding this aesthetic complaint. After the patient has been permitted to articulate some basic concerns about his or her aesthetic interests, the surgeon can offer a tentative recommendation based on an expeditious and targeted examination. Feedback about the patient’s understanding and agreement should be elicited before moving forward with the discussion. If the patient assents to the general line of thinking, then the surgeon may continue to elaborate more fully. Constant interaction and adjustment of the discussion must take place to ensure that the conversation is progressing in accordance with the patient’s expectations. Nevertheless, the surgeon must direct the conversation at times, even redirecting it if need be. For example, if the patient exhibits only minimal jowling along the jaw line but notable brow ptosis, the surgeon can introduce the idea of a browlift judiciously if the patient appears receptive to this idea. Although the surgeon must remain sensitive to the patient at all times, he or she should not hesitate to offer the patient an educated opinion that may step somewhat outside of the patient’s initial concerns so long as the patient appears to demonstrate the right temperament to accept these suggestions. The patient may achieve the maximal rejuvenation possible and see a more dramatic benefit by undergoing the procedure the surgeon advises. With experience, the physician will know when and how to direct the conversation. In certain circumstances, the physician should exercise caution when introducing other aesthetic flaws about which the patient has not yet remarked. For instance, drawing attention to a prominent nasal hump of an aging face is rarely indicated when unsolicited, even if the nose is suffering from the effects of aging; suggesting the removal of an unsightly mole may prove disastrous. These kinds of concerns may be safely addressed once the patient introduces them. As a general guide, the surgeon should remain within the sphere of the patient’s general complaint; that is, only speak about the aging face if that is the principal concern of the patient (with the aging nose as an exception for inclusion).
It is important to focus the patient during the consultation. A great deal of information must be exchanged, and patient fatigue may become an issue. As mentioned, the preconsultation aids in focusing the consultation. Once the patient’s principal concern is recognized, the physician must manage to accomplish a brief, targeted physical examination, recommend appropriate procedure(s), and describe the precise nature of the surgical endeavor. However, details about the risk involved with surgery may be better deferred to a separate session. (See the following section on Preoperative Counseling.) Selection of an appropriate candidate for surgery is a critical skill that must be developed. Refusal to operate on unsuitable individuals, especially those with unrealistic expectations, will prove to be a prudent decision in the end. If the surgeon once undertakes elective surgery on an unreasonable or (worse yet) litigious patient, then he or she will hesitate to repeat this costly error in the future. A good admonition is only to agree to proceed on one’s own terms rather than acquiesce to the patient’s every caprice. Often, patients are not ready to book surgery at the time of consultation because of deficient financial or mental preparedness. Therefore, the surgeon should try to convert patients to surgery who have reasonable expectations, psychological readiness, and the financial resources for elective surgery. A practical estimate for this figure is approximately 50% to 60% of all consultations. In a maturing practice (5 to 10 years of clinical practice), the objective should be to schedule enough consultations in a given week with an estimated conversion rate to fill the operating schedule for 2 to 4 weeks in advance. A schedule that falls below this quota will permit valuable operating time to be left idle. In a mature practice (10 to 15 years of clinical experience), booking beyond this period, approximately 1 to 2 months in advance, avoids fluctuations in monthly revenue. With this objective in mind, patients will not turn away because of a prolonged waiting period but perceive that the surgeon is in demand because of the need for advanced
booking. Nevertheless, bountiful surgical volume is a welcome problem.
booking. Nevertheless, bountiful surgical volume is a welcome problem.
Preoperative Counseling
Preoperative counseling initially takes place during the consultation. Risks, benefits, and alternatives are briefly explained to the patient, but the focus throughout remains on the aesthetic objectives of surgery. If the patient is interested in scheduling surgery at the conclusion of the session, then a date should be chosen for the procedure, and either a partial (deposit) payment should be collected or the entire amount to reserve the scheduled surgical date. Also at the time of the initial consultation, a separate session should be scheduled during which formal, preoperative counseling may be undertaken. Because the consultation process may be quite taxing to the patient, this separate appointment can permit the patient some time to regain composure and concentration to digest the extensive amount of information that must be conveyed during the preoperative counseling meeting. In addition, the surgeon need not be present throughout the entire preoperative counseling session and thereby be alleviated the burden of the added time commitment.
During the preoperative counseling session, one must explain in detail the exact risks the surgery entails in more graphic terms than were expressed at the time of consultation. The two negative aspects of the surgical endeavor that must be truthfully and carefully explained to the patient are the material risks and surgical limitations. Material risks include all major complications that can, but only infrequently, occur (e.g., facial nerve paralysis), or minor complications that more commonly occur (e.g., milia after resurfacing or prolonged ecchymosis and edema). The surgeon should relay all of this information systematically, sincerely, and clearly but without labored commentary that might otherwise engender undue trepidation on the part of the patient. In addition, surgical limitations must be forthrightly stated, which include the unattainable goal of symmetry, specific anatomic constraints, and reasonable cosmetic/functional improvement. After all of these details have been elaborated, the patient must be granted the opportunity to ask any pertinent questions about the stated limitations, risks, benefits, and alternatives before a formal, informed consent is obtained. The patient then is given the informed consent and left undistracted during careful review of the written document and then signature. The authors have relied on a standardized, detailed dictation “macro” that elaborates all of the material risks and limitations for each procedure and that is incorporated into a typewritten preoperative evaluation note. Although many legitimate alternatives exist for medico-legal documentation, the surgeon always should ensure that some form of written documentation exists that outlines all of the potential negative consequences that may follow surgery.
After the consent is properly obtained, the surgeon should conduct a more formal history and physical examination that covers all aspects of the patient’s health and family history in order to determine how extensive a preoperative medical evaluation is required to ensure patient safety during the operation. Guidelines for requisite laboratory studies, related radiographic imaging, cardiac evaluation, and preoperative medical clearance lie beyond the scope of this textbook and should be determined on an individual basis.
After this portion of the preoperative counseling session is completed, the surgeon may delegate the rest of the work to a reliable staff member who can dutifully complete the remaining tasks. The entire surgical process, from arrival at the surgery center through the postoperative recovery period, is explained to the patient as part of preoperative counseling. Details of postoperative care may be overwhelming for the patient at this point, particularly for the individual who will undergo resurfacing, and is best left to the postoperative period. However, the patient should understand clearly the appointed time of arrival, location of surgery, and other related information. For instance, the patient should know that no fingernail polish should be worn on one finger to accommodate the pulse-oximetry meter or that a button-down shirt is preferred in order to avoid the difficulty of a pullover shirt after facial surgery. All of these details are printed in the preoperative instruction sheet (included at the end of this chapter), which should be explained to the patient line by line. Other salient concerns include perioperative use of aspirin, aspirin-related products, herbal medications, or vitamins that can adversely affect hemostasis or exacerbate photosensitivity. Again, the reader is referred to the specific documents that cover these details (appended at the end of this chapter). After everything has been explained to the patient, prescriptions handed over, and postoperative appointments scheduled, the patient should sign a preoperative checklist sheet that states that he or she has been thoroughly counseled, given the opportunity to ask any questions, and has understood all of the presented material. All standardized photographs also should be taken at this session.
The Role of Digital Imaging
Digital imaging has become an indispensable and sole means for photographic documentation, retrieval, and presentation in the authors’ practices. This section expounds on how digital imaging can be effectively incorporated into a plastic surgical practice at every level so that 35-mm film may be entirely abandoned. Although technology continues to evolve rapidly, certain basic tenets that relate to setup and execution remain steadfast and are included herein. Some of the material presented will become obsolete, and the reader is referred to the latest periodicals, the Internet, or other reliable sources for updated advice on these matters. Forthcoming sections discuss the effective use of digital morphing and photography separately.
Although 35-mm film has become the standard of professional plastic surgical communication and documentation, digital imaging has quickly made incursions into this exclusive domain. The initial set-up costs for digital imaging clearly exceed that of 35-mm photography, but that margin is diminishing daily. In addition, the savings that accrue over time in terms of expended cost, labor, and time over conventional film will manifest clearly in a relatively short time frame. Paper and ink consumables for ink jet printing remain relatively expensive but fall short of 35-mm transparency film purchases. More important, the time needed to catalog 35-mm film when it returns from the photography laboratory translates into excessive staff labor that could be redirected more profitably elsewhere. Retrieving and reviewing standard transparency film can also be a labor-intensive effort. The added sorting and storage space for film-based photography can also prove burdensome. Over time, film in whatever format fades, scratches, or (even worse) gets lost; whereas digital imaging remains in pristine condition and can be infinitely backed up even in remote locations in order to prevent against theft, loss, or force majeure. The unmatched flexibility of the digital medium should be considered in that electronic communication between physicians can be facilitated and the capacity for digital morphing is possible. Also, because images can be immediately reviewed on the digital viewfinder or computer monitor, the chance of a poor outcome is reduced and the ability to use that information immediately for patient communication is enhanced. Hopefully, the reader has been persuaded that digital imaging offers a viable, photographic medium for a plastic surgical practice.
Two principal input devices exist to capture an image digitally: digital cameras and scanners. Digital cameras have become increasingly affordable, and advanced features can be found even on budget-conscious models. A thorough discussion of the requisite features and options of a digital camera that would be necessary for a plastic surgical practice cannot be persuasively undertaken given the risk of obsolescence of the material presented. Nevertheless, certain fundamental considerations are addressed. The pixel war continues to wage, and resolution quality always has been a preeminent concern. The poor image resolution that accompanies the digital format is the major drawback of digital imaging that diehards of the film medium cite. Although ISO 50 speed film may provide exceptional quality, the grain-versus-pixel debate carries little meaningful value in the world of plastic surgery. Most images obtained on a routine basis never become enlarged beyond an 8- -10 inch printed format. Even so, no consensus exists as to the equivalent conversion of a film grain to a digital pixel, and estimates have fallen anywhere from 2 to 80 million pixels to achieve parity with a high-quality 35-mm print. The true bottom line is that digital cameras provide superb image quality and ultimately conserve time, labor, and expense.
-10 inch printed format. Even so, no consensus exists as to the equivalent conversion of a film grain to a digital pixel, and estimates have fallen anywhere from 2 to 80 million pixels to achieve parity with a high-quality 35-mm print. The true bottom line is that digital cameras provide superb image quality and ultimately conserve time, labor, and expense.
 -10 inch printed format. Even so, no consensus exists as to the equivalent conversion of a film grain to a digital pixel, and estimates have fallen anywhere from 2 to 80 million pixels to achieve parity with a high-quality 35-mm print. The true bottom line is that digital cameras provide superb image quality and ultimately conserve time, labor, and expense.
-10 inch printed format. Even so, no consensus exists as to the equivalent conversion of a film grain to a digital pixel, and estimates have fallen anywhere from 2 to 80 million pixels to achieve parity with a high-quality 35-mm print. The true bottom line is that digital cameras provide superb image quality and ultimately conserve time, labor, and expense.The key to consistent photography is use of the same camera for all preoperative and postoperative photographs owing to the nuances in the way a digital camera captures an image. Each camera possesses a different dynamic range; that is, the ability to capture the darkest blacks to the lightest whites and all of the intervening colors as well. Color accuracy (discussed under scanners) also can vary significantly among digital cameras. The exact methods by which the reader can achieve consistent, reproducible photographs digitally are discussed in a following section.
Scanners provide a method by which 35-mm film (transparencies, negatives, and prints) can be converted over to the digital medium. For film transparencies or negative exposures, dedicated film scanners so far have provided the optimal conversion quality to digital in terms of accurate translation of color, resolution, and restoration of imperfections in the source image (scratches, color fade, or other noise). In lieu of a film scanner, a flatbed scanner provides versatility and affordability: besides transparencies and negatives, printed images and text also can be transformed into the digital medium. Generally, four parameters exist that define a scanner’s optical reproduction quality: optical resolution, bit depth, color accuracy, and optical density. Optical resolution simply refers to the number of pixels per inch (ppi). Pixels per inch is a linear measurement and is different from dots per inch (dpi; also linear), which a printer outputs. Bit depth or color bit depth refers to the maximum number of colors that each pixel of an image can display. For convenience, color depth is defined in terms of power of 2. A black-and-white image, for instance, has two colors or 2 to the first power; therefore, it is termed a one-bit image. At the other end of the spectrum, an RGB True Color image may display 16.7 million colors, which is equivalent to 2 to the 24th power, or 24 bits. Most consumer output devices, printers, and monitors are limited to 24 bits. However, scanners can be 30, 36, or even 42 bits. These scanners actually create a better image. Color accuracy refers to the overall ability of a scanner to reproduce faithfully the original colors of the scanned image. The standard developed by the International Color Consortium (ICC) has allowed testers to measure precisely the “Delta E,” or variance of the scanned from the original color. A Delta E of one correlates to the barely perceptible difference between colors seen in a controlled lighting situation by an experienced viewer. Good Delta Es fall below 10, and poorer values may exceed 30. The fourth major specification for a scanner is optical density (OD), and generally is not a descriptor of lower-end models. Optical density refers to the brightness that a scanner is able to capture. Optical density is measured in a logarithmic fashion. Therefore, a scanner with a 3.6 OD has 10 times the brightness of one with a mere 2.8 OD. Generally, OD is not as critical when scanning text or prints but greatly influences the quality of a scanned negative or slide. If a scanner does not boast an OD rating, then one should consider the OD to fall between 2.8 and 3.0. It is recommended
that a minimum of 3.2 OD be present for transparencies and 3.4 OD for negatives.
that a minimum of 3.2 OD be present for transparencies and 3.4 OD for negatives.
The image must be stored appropriately to permit rapid and easy retrieval once it has been captured. Archiving programs abound, each with touted claims of superiority. More advanced software programs permit attachment of “metatags” to an image (e.g., “crooked nose,” “Susan Smith”) that facilitate the search for these titles during routine image retrieval or academic research. A simple, reliable method that dispenses with dedicated archiving software is placement of patient images into a folder labeled by the date that the image was taken (e.g., 03-11-6) with the year as the leading value to maintain chronologic integrity, which in turn is placed into a folder with the patient’s name (Smith, Susan). All of these images should be backed up on a routine basis to avoid any potential loss owing to a host of unforeseen factors.
After the image has been captured and stored, it can then be outputted via two main techniques, a printer, or a digital projector. Three main types of printers exist on the market today: the laser printer, ink jet printer, and dye-sublimation printer. The ink jet printer remains the mainstay of printing affordable, photographic-quality images but still can extort a high toll for the price of consumables (ink and paper). Nevertheless, the cost of these consumables can be markedly reduced by printing only select photographs for the patient. Generally, the authors print a set of photographs for the patient at 1 week or 1 month in order to show the patient the difference between before-and-after surgery. Of note, these images can be an excellent marketing tool, because enthusiastic patients often show their colleagues and friends the remarkable transformation that has occurred in their appearance. Color laser printers have decreased in price and can provide a cost savings if a heavy volume of printing is projected. The quality of a color laser print typically falls short of the photographic potential of a color ink jet print produced on specially treated paper. However, the cost per page of a laser color print is markedly less than for an ink jet print because of the less expensive consumables used for laser printing (ink and paper). Finally, dye-sublimation printers provide unparalleled quality in even-tone transition that can mimic film photography but may not truly be necessary. Their versatility is also limited, because only photographs of a certain prescribed size may be output and text-based copy cannot be effectively reproduced. Nevertheless, prices for these printers have continued to fall to consumer-friendly levels, and their widespread distribution may be imminent.
As film transparencies have been replaced with digital equivalents, old slide projectors have given way to the advent of digital projectors. Digital presentations are more elegant than film-based presentations in that subtle animation and edited video clips can be embedded into the lecture. In addition, any aspect of the talk can be updated or altered easily at any time without added expense or labor. Portable projectors are a handy way of presenting seminars on-site or off-site. There are many types of projectors available on the market today, all of which can provide excellent image reproduction, including cathode ray tube (CRT) projectors, liquid crystal display (LCD) projectors, digital light projectors (DLP), and plasma display panel (PDP) projectors. Another factor to consider is “native,” or uncompressed and unexpanded, resolution level of one of the following grades: VGA (640  480), SVGA (800
480), SVGA (800  600), XGA (1,024
600), XGA (1,024  768), SXGA (1,280
768), SXGA (1,280  1,024), and UXGA (1,600
1,024), and UXGA (1,600  1,200). Cathode ray tubes that use an analog-based technology, do not have a native resolution level, but are considered resolution independent, which means that they can handle most computer monitor resolutions without needing to be matched to the monitor’s exact resolution. Digital projectors, on the other hand, must be matched to the monitor’s resolution. Ideally, they should match the monitor resolution exactly. However, if several computers with different monitor resolutions are to be used with one projector, then the projector should be matched with the highest resolution screen. A minimum of SVGA for simple graphic presentations is recommended, but an SXGA is preferred for improved resolution and display of more detailed images. The other major parameter that defines a projector’s quality is the brightness, defined in ANSI lumens. A minimum of 300 to 500 ANSI is recommended for dimly lit rooms; a 1,000-ANSI minimum is recommended for well-lit rooms; and larger venues such as auditoriums demand a minimum of 1,500 ANSI. The contrast ratio—which refers to the range of brightest whites to darkest blacks that a projector can display—also affects image quality and can range from a low value of 100:1 to a high value of 2,000:1. Zoom lenses can aid in changing the projected image size without the cumbersome need for physically repositioning the unit. Digital keystone correction refers to the ability of the projector to correct any distortions that may be displayed when the projector is aimed at a wall from an angle.
1,200). Cathode ray tubes that use an analog-based technology, do not have a native resolution level, but are considered resolution independent, which means that they can handle most computer monitor resolutions without needing to be matched to the monitor’s exact resolution. Digital projectors, on the other hand, must be matched to the monitor’s resolution. Ideally, they should match the monitor resolution exactly. However, if several computers with different monitor resolutions are to be used with one projector, then the projector should be matched with the highest resolution screen. A minimum of SVGA for simple graphic presentations is recommended, but an SXGA is preferred for improved resolution and display of more detailed images. The other major parameter that defines a projector’s quality is the brightness, defined in ANSI lumens. A minimum of 300 to 500 ANSI is recommended for dimly lit rooms; a 1,000-ANSI minimum is recommended for well-lit rooms; and larger venues such as auditoriums demand a minimum of 1,500 ANSI. The contrast ratio—which refers to the range of brightest whites to darkest blacks that a projector can display—also affects image quality and can range from a low value of 100:1 to a high value of 2,000:1. Zoom lenses can aid in changing the projected image size without the cumbersome need for physically repositioning the unit. Digital keystone correction refers to the ability of the projector to correct any distortions that may be displayed when the projector is aimed at a wall from an angle.
 480), SVGA (800
480), SVGA (800  600), XGA (1,024
600), XGA (1,024  768), SXGA (1,280
768), SXGA (1,280  1,024), and UXGA (1,600
1,024), and UXGA (1,600  1,200). Cathode ray tubes that use an analog-based technology, do not have a native resolution level, but are considered resolution independent, which means that they can handle most computer monitor resolutions without needing to be matched to the monitor’s exact resolution. Digital projectors, on the other hand, must be matched to the monitor’s resolution. Ideally, they should match the monitor resolution exactly. However, if several computers with different monitor resolutions are to be used with one projector, then the projector should be matched with the highest resolution screen. A minimum of SVGA for simple graphic presentations is recommended, but an SXGA is preferred for improved resolution and display of more detailed images. The other major parameter that defines a projector’s quality is the brightness, defined in ANSI lumens. A minimum of 300 to 500 ANSI is recommended for dimly lit rooms; a 1,000-ANSI minimum is recommended for well-lit rooms; and larger venues such as auditoriums demand a minimum of 1,500 ANSI. The contrast ratio—which refers to the range of brightest whites to darkest blacks that a projector can display—also affects image quality and can range from a low value of 100:1 to a high value of 2,000:1. Zoom lenses can aid in changing the projected image size without the cumbersome need for physically repositioning the unit. Digital keystone correction refers to the ability of the projector to correct any distortions that may be displayed when the projector is aimed at a wall from an angle.
1,200). Cathode ray tubes that use an analog-based technology, do not have a native resolution level, but are considered resolution independent, which means that they can handle most computer monitor resolutions without needing to be matched to the monitor’s exact resolution. Digital projectors, on the other hand, must be matched to the monitor’s resolution. Ideally, they should match the monitor resolution exactly. However, if several computers with different monitor resolutions are to be used with one projector, then the projector should be matched with the highest resolution screen. A minimum of SVGA for simple graphic presentations is recommended, but an SXGA is preferred for improved resolution and display of more detailed images. The other major parameter that defines a projector’s quality is the brightness, defined in ANSI lumens. A minimum of 300 to 500 ANSI is recommended for dimly lit rooms; a 1,000-ANSI minimum is recommended for well-lit rooms; and larger venues such as auditoriums demand a minimum of 1,500 ANSI. The contrast ratio—which refers to the range of brightest whites to darkest blacks that a projector can display—also affects image quality and can range from a low value of 100:1 to a high value of 2,000:1. Zoom lenses can aid in changing the projected image size without the cumbersome need for physically repositioning the unit. Digital keystone correction refers to the ability of the projector to correct any distortions that may be displayed when the projector is aimed at a wall from an angle.Digital Morphing Software
Digital morphing software allows a surgeon to alter a patient’s image digitally to provide an envisioned surgical outcome. Although this medium can be used effectively for patient communication, it must be properly harnessed to maximize its benefit but minimize confusion and limit liability. Digital morphing is only appropriate in select facial cosmetic surgery. Because any kind of photographic imaging is only a two-dimensional medium, conveyance of three-dimensional information using digital imaging may be poor or inaccurate. For example, digital translocation of tissue may not be readily apparent on the frontal view, because flesh color is moved on top of each other from one part of the face to another. Instead, profile views can be particularly informative when the tissue is moved against the uniform blue background. For instance, the nasal profile can be augmented, rotated, or refined using the digital imager quite effectively
(Fig. 3-2A,B). Similarly, a hypoplastic chin, submental fullness, or platysmal diastasis may be very easily depicted with the digital imager (Figs. 3-3A,B; 3-4 A-C; and 3-5 A,B). More important, the patient often fails to appreciate his or her own profile view; therefore, the digital imager provides valuable information that can convince the patient of a cosmetic benefit that would otherwise be incommunicable. The frontal view, on the other hand, still can be used for select purposes in digital morphing. A browlift result can be approximated using digital subtraction techniques between two digital photographs, one showing the native ptotic brow position, and the other the manually lifted brow position (Fig. 3-5 C, D). The brow must be overcorrected somewhat to eliminate the redundant upper-eyelid skin by pulling upward on the brow manually until all of the excess soft tissue and skin have been effaced—a process that typically imparts a startled expression. In order to correct this unnatural appearance, the brow then should be readjusted downward somewhat. Despite the benefit that digital imaging may afford for the patient entertaining brow rejuvenation, simple use of a hand-held mirror and manual elevation of the brow may be a more direct, natural-appearing, and effective technique (Fig. 3-6). Effacement of wrinkles similarly can be very difficult to undertake given the stated limitation with flesh-on-flesh alterations; or worse, digital resurfacing may promise the patient too much (especially the acnescarred patient), or look bizarrely artificial with a smeared, textureless appearance. Although nasal changes can be appreciated best on lateral view, the width and attitude of a nasal tip, alae, or dorsum can be adjusted or straightened on frontal view using digital imaging with meaningful results. In summary, digital morphing software must be used only in the select cases (e.g., the profile view), in which it would prove beneficial to convince the patient of a cosmetic benefit to surgical intervention.
(Fig. 3-2A,B). Similarly, a hypoplastic chin, submental fullness, or platysmal diastasis may be very easily depicted with the digital imager (Figs. 3-3A,B; 3-4 A-C; and 3-5 A,B). More important, the patient often fails to appreciate his or her own profile view; therefore, the digital imager provides valuable information that can convince the patient of a cosmetic benefit that would otherwise be incommunicable. The frontal view, on the other hand, still can be used for select purposes in digital morphing. A browlift result can be approximated using digital subtraction techniques between two digital photographs, one showing the native ptotic brow position, and the other the manually lifted brow position (Fig. 3-5 C, D). The brow must be overcorrected somewhat to eliminate the redundant upper-eyelid skin by pulling upward on the brow manually until all of the excess soft tissue and skin have been effaced—a process that typically imparts a startled expression. In order to correct this unnatural appearance, the brow then should be readjusted downward somewhat. Despite the benefit that digital imaging may afford for the patient entertaining brow rejuvenation, simple use of a hand-held mirror and manual elevation of the brow may be a more direct, natural-appearing, and effective technique (Fig. 3-6). Effacement of wrinkles similarly can be very difficult to undertake given the stated limitation with flesh-on-flesh alterations; or worse, digital resurfacing may promise the patient too much (especially the acnescarred patient), or look bizarrely artificial with a smeared, textureless appearance. Although nasal changes can be appreciated best on lateral view, the width and attitude of a nasal tip, alae, or dorsum can be adjusted or straightened on frontal view using digital imaging with meaningful results. In summary, digital morphing software must be used only in the select cases (e.g., the profile view), in which it would prove beneficial to convince the patient of a cosmetic benefit to surgical intervention.
Despite its benefits, digital morphing software can be a two-edged sword. Liability remains a key reason why many surgeons have not adopted this technology. Fear that an envisioned result may be misinterpreted as a promise of guarantee has hindered even the brave. However, care can be taken to educate the patient that morphing only provides a method of communication and does not represent any claims that the surgical results will approximate the digitally conceived image. Patients are asked to sign a waiver that states their acknowledgment of this fact, which becomes incorporated into the medical record. Further, no altered image is ever given to the patient to take home or saved in the hard drive; therefore, no record is retained of the retouched image. As an important side note, if the patient has already decided on surgery, the surgeon should not endeavor to
show the patient the digitally morphed image at that point. Doing so may convince the patient that surgery is not indicated and thereby jeopardize the transaction.
show the patient the digitally morphed image at that point. Doing so may convince the patient that surgery is not indicated and thereby jeopardize the transaction.
 FIGURE 3-4. A-C: The patient is shown with the projected benefit of a chin augmentation, submentoplasty, and facelift on the digital imager (B) and 2 months after surgery (C). |
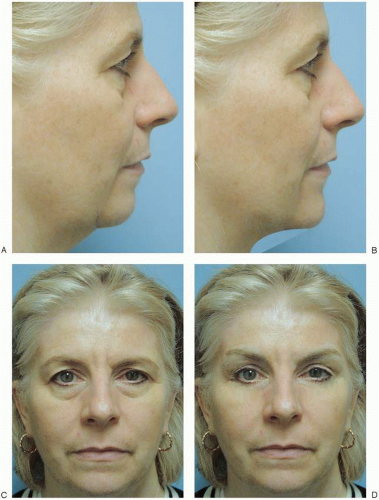 FIGURE 3-5. A,B: The lateral view of the patient shows the projected benefit that a submentoplasty and facelift will give the patient using the digital imaging software (B). Of note, the patient’s brow ptosis is not digitally corrected on the lateral view because of difficulty in accomplishing this objective. C,D: On frontal view, the patient is shown before and after digital modification of her brow ptosis. Of note, the jowling and neck region are left unretouched because of the difficulty in conveying this information on frontal view. If the patient would like to see a simulation of how a facelift/submentoplasty would appear on frontal view, the surgeon should simply lift the tissues manually and show the benefit to the patient in a hand-held mirror.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|







