Upper and Midfacial Rejuvenation
Samuel M. Lam
Edwin F. Williams III
At first, a chapter devoted to both upper and midfacial rejuvenation rather than an individual chapter for each topic may seem illogical. However, after completing this chapter, the reader should appreciate how these two facial zones are intimately linked. Midfacial elevation may be achieved via a browlift incision, which is the authors’ preferred approach. Alternatively, the midface may be lifted through an extended lower-blepharoplasty incision. This approach is less ideal for reasons that are enumerated herein; however, it is still a viable technique. The authors discourage midfacial rejuvenation via a rhytidectomy incision, because the favored vector of lift is vertical, which cannot be accomplished easily with a laterally based incision.
This chapter covers the pertinent details in brow elevation via a minimal-incision technique that can rejuvenate the upper and midface as a unit. Midfacial rejuvenation is described via a lower-blepharoplasty incision and alloplastic implantation. Eyelid rejuvenation is discussed in the many complex variations that exist to achieve the desired objective: ptosis repair, upper-lid blepharoplasty (with and without medial fat excision), transconjunctival lower-lid blepharoplasty (with and without skin pinch), and transcutaneous skin-muscle flap (with or without midfacial extension). The proper selection of technique is as critical as the execution, and the relevant preoperative considerations are also addressed. Finally, the reader is guided through the postoperative period to care for the patient during the normal postoperative course as well as to formulate the appropriate decision making required if complications arise.
PREOPERATIVE CONSIDERATIONS: PATIENT SELECTION AND RELEVANT ANATOMY
Upper Face (Brow and Eyelid) Rejuvenation
Interestingly, the authors have observed that many patients begin to exhibit brow ptosis about 10 years before any evidence of lower facial jowl formation. Obviously, this finding is not universally present. (On the other hand, submental fullness, as an independent phenomenon, can occur at any age because of heredity, obesity, or aging.) Surgeons in the past have been reluctant to undertake brow elevation because of apprehension over the potential morbidity associated with traditional coronal-type browlifts. Patients in turn have at times expressed some reticence to accept the added recovery time associated with this technique. Newer minimally invasive techniques have been able to restore the upper face with potentially less morbidity (smaller incisions, faster recovery, shorter and temporary scalp anesthesia, and less risk of scarring and alopecia) than the coronal lift while maintaining commensurate longevity and achieving equally favorable aesthetic results. Despite the fanfare that accompanied the midbrow lift, it still may be an arduous task to convince a patient, especially a younger patient, to agree to a brow lifting procedure that involves incisions in a highly visible location. Similarly, the direct browlift (at the eyebrow) has assumed a less prominent role in brow rejuvenation for a host of reasons, including poor scar camouflage, irregular alopecia, and technical difficulty. The authors rely on the “endoscopic” approach (five abbreviated incisions) to rejuvenate the brow, but have eliminated use of all endoscopic equipment and further can achieve midfacial rejuvenation via the same incision by carrying the dissection over the zygomatic arch. Although the endoscopic technique for brow rejuvenation is well known, a more accurate term, “minimally invasive” browlift, which reflects the technique advocated in the text, is substituted for the remainder of this volume.
Unlike the traditional facelift that solely addresses an aesthetic deficit along the lower face, brow and eyelid surgery may restore youth but also correct a functional visual impairment. Furthermore, the somewhat prosaic aphorism still captures the essence of upper facial rejuvenation: “The eyes are the window to the soul.” When an individual engages in conversation or even casually gazes at another, he or she usually fixates on the others’ eyes, which makes upper facial rejuvenation a critical aspect of restoring vibrancy and vitality to an individual that a facelift can less often accomplish. Patients who exhibit brow and eyelid aging often are accused of looking “angry,” “sad,” or “tired”—comments that belie that individual’s true temperament and disposition. These unjustified remarks levied at the patient add another dimension of psychological burden for which the patient may desire a remedy other than correction for the stigma of aging alone.
Patients often present to the physician confused about what they actually want corrected. Often, the mass media has indoctrinated them into equating blepharoplasty with the cure for their woes. However, the surgeon must carefully select between upper-lid blepharoplasty (skin pinch with or without fat removal), lower-lid blepharoplasty (transconjunctival with or without skin removal versus transcutaneous), browplasty, and blepharoptosis repair, or a combination thereof to achieve the proper desired result. This section elucidates this thinking process so that the surgeon will possess a systematic appraisal of the aesthetic and functional deficits that require surgical intervention.
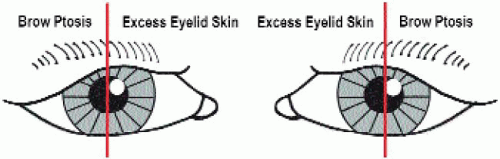
First, a simplified algorithm should be introduced that may facilitate easy analysis (but should be used with discretion and judgment). A vertical line can be drawn through the midpupil. Generally, any tissue ptosis medial to this line may be thought of as upper eyelid in origin and may be corrected with an upper-lid blepharoplasty. Conversely, any ptosis that presents lateral to this imaginary line may be assumed to be principally caused by brow ptosis rather than excessive upper-lid skin (or dermatochalasis) (Fig. 4-1). The fallacy that bedevils many junior surgeons is the same unsophisticated thinking that encumbers patients—that all upper-lid tissue ptosis is a byproduct of redundant eyelid skin rather than brow ptosis. Quite the contrary is true: The brow tends to age chronologically earlier than the onset of upper-eyelid skin redundancy. Furthermore, the absence of a developed lateral depressor brow complex (the orbicularis oculi provides weak counter pull to the brow laterally) as opposed to the well-developed medial depressor brow complex (corrugator and procerus) may contribute to the disproportionate lateral-brow descent. Anatomic studies also have highlighted the weaker development of the lateral-brow musculature that may serve as the principal cause for more significant lateral-brow ptosis, among other factors.1, 2 and 3 If an upper-lid blepharoplasty is performed in lieu of a recommended browplasty, the brow actually may be further depressed; and if excessive upper-lid skin is removed, a browlift may be precluded in the future because of risk of lagophthalmos. Also, an aggressive upper-lid blepharoplasty alone, especially if the adjacent, thicker brow skin is removed together with the thinner upper-lid skin, may result in an unnatural appearance.
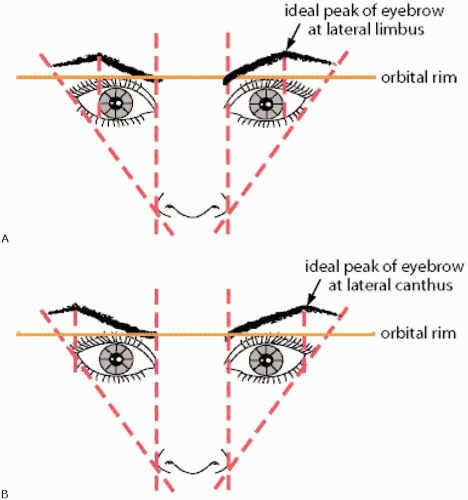
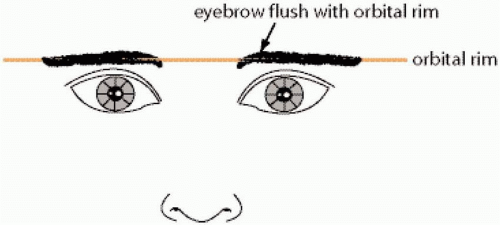
The aesthetic position of the brow always should be recalled when considering a browlift. In the ideal female eyebrow, the eyebrow configuration assumes a tapered contour with a thicker, medial club of the eyebrow narrowing laterally to a fine point. The medial brow should rest at or slightly below the orbital rim with the peak of the eyebrow situated either at the lateral limbus (classical description, Fig. 4-2A) or at the lateral canthus (revised description, Fig. 4-2B) lying above the orbital rim. Laterally, the eyebrow descends somewhat to end at a point drawn through the imaginary line that joins the alar-facial groove through the lateral canthus. The descended brow often assumes a more flattened appearance that resembles the ideal male eyebrow; that is, a straight line that runs along the orbital rim (Fig. 4-3). Because the ideal female brow is arched laterally and the brow descends disproportionately laterally, the primary efforts to raise the brow position should be concentrated laterally. All fixation sutures are laterally based, and no medial suspension is undertaken. This surgical technique properly restores the ptotic brow without unnaturally producing the startled or frightened appearance that is a stigma of an improper browlift.
Another fallacy that has ensnared the neophyte surgeon is the thought that the eyebrow (the hairy portion of the brow) is the exclusive aspect of the brow that requires rejuvenation. Instead, the entire lateral brow complex should be viewed as a unit, which includes both the hair-bearing eyebrow and the adjoining soft tissue. As part of the physical assessment, the surgeon should place his or her thumb along the ptotic lateral brow and lift the tissue upward, carefully observing the improved position of the descended soft tissue and hair-bearing eyebrow. The patient also should be educated about this aesthetic deficit and confronted with the rejuvenated appearance using a mirror while the surgeon gently lifts the ptotic brow. Any excessive eyelid skin that remains after appropriate brow elevation may be pinched with a forceps or between the surgeon’s fingers to illustrate how a concomitant blepharoplasty would further enhance the intended objective. However, if the patient desires only an upper-lid blepharoplasty despite a thoughtful education, the surgeon should plan for a conservative upper-lid skin excision that will not compromise a prospective future browlift or exacerbate the brow ptosis.
After a careful inspection of the lateral brow for signs of ptosis, the surgeon then should pay meticulous attention to the upper lid that lies medial to the imaginary vertical midpupillary line. Again, this area represents principally upper-eyelid pathology—excessive upper-lid skin and/or pseudoherniation of fat (steatoblepharon). The redundant upper-eyelid skin should be pinched with a pair of fine forceps to determine the amount of skin that must be excised to achieve the optimal rejuvenation and demonstrate the intended surgical goal to the patient. Unlike the lower lid, which may have pseudoherniation of fat along the entire border, the upper lid suffers from fat protrusion chiefly medially. The central pocket is less likely to be herniated, and the lateral pocket is comprised entirely of the lacrimal gland, the repair of which lies beyond the scope of this textbook. This medial fat bulge should be noted and explained to the patient so that a proper preoperative plan for fat excision can be established.
The last consideration for upper brow and eyelid pathology that should be studied is evidence of blepharoptosis; that is, levator dysfunction and actual eyelid descent over the pupil. This condition should be differentiated from pseudoptosis that results from excessive upper-eyelid skin (dermatochalasis) that causes the lid to appear descended.
Both true ptosis and pseudoptosis can obscure the visual axis and lead to visual field restriction. Most cases of eyelid ptosis are a result of senility and exhibit the following characteristic hallmarks:
Normal lid excursion (usually 8 to 12 mm), which can be tested by fixating the brow in position with a finger so that brow elevation is eliminated and true lid excursion can be assessed.
High or absent supratarsal lid crease because of disinsertion or weakening of the levator.
Thin, upper-eyelid skin that renders the underlying iris visible through the attenuated skin.
The palpebral fissure should be about 7.5 to 10 mm in distance. However, a more useful measurement is the margin reflex diameter-one (MRD-1), which is defined as the distance from the corneal light reflex (situated at the midpupil during primary gaze) to the upper-lid margin (Fig. 4-4). A normal MRD-1 should be 2.5 to 5 mm, and an abnormal value is considered less than 2 mm. If the lid overhangs the corneal light reflex, then every millimeter below the light reflex is considered a negative value. The MRD-2 is defined as the distance from the corneal light reflex to the lower-lid margin and is important in the evaluation of lower-lid malposition. A normal value of the MRD-2 is 4 to 5.5 mm. If the patient exhibits unilateral ptosis, then the ptotic lid should be elevated to the normal position, during which time the contralateral lid position is observed. Often the contralateral lid is seen to descend because of a central tonic mechanism that maintains lid position until the affected ptotic lid is digitally suspended. This phenomenon is known as Hering’s Law. During assessment of lid ptosis, formal visual-field assessment should be obtained by an ophthalmologist or optometrist. If Hering’s Law appears to be in effect, the ptotic lid should be taped in an elevated position while the contralateral visual field is measured.
Finally, the lower lid should be assessed for its aesthetic qualities. Pseudoherniation of fat, dermatochalasis, and hypertrophic roll of the orbicularis-oculi muscle typically are the targets for rejuvenation. Pseudoherniation of fat can be assessed effectively on the frontal and lateral views and accentuated on upward gaze. Patients with a significant amount of fat protrusion may even show well-demarcated fat pockets (medial, central, and lateral). Dermatochalasis, or excessive lid skin, may be assessed with a simple pinch using forceps to estimate the amount needed for removal. A hypertrophic orbicularis oculi muscle may be evident as a roll of tissue that is exaggerated during muscular contraction such as smiling.
Besides these aesthetic issues, the surgeon must be fully cognizant of the potential for postoperative lid malposition, which may arise even in the most qualified hands. Preoperative evaluation of lid tone and position must be an integral facet to every physical examination before embarking on a surgical undertaking. Lower-lid position should be assessed on primary gaze without digital distraction or other manipulation. If the patient already exhibits scleral show, lateral rounding, or frank ectropion, then a lid shortening procedure such as a tarsal strip, should be entertained. A lid distraction test should be performed in which the lower lid is pulled downward with one finger in order to assess lower-lid laxity. If the lid is in normal position before distraction and can be pulled downward with little resistance, then a lid-shortening procedure should be considered. However, if the lower lid is already malpositioned and moves very little with distraction, then vertical shortening of the lower lid may be present (e.g., an anterior, middle, or posterior lamellar deficiency). Usually, vertical shortening arises because of overzealous blepharoplasty in the past and requires replacement with the appropriate tissue. It is recommended that ophthalmologic guidance be sought if such a deficiency exists. A lid retraction test (or snap test) also should be performed to
test the resilience of the lower lid. The lower lid is pinched between the index finger and thumb and pulled away from the globe. If the lid returns to contact the globe after 1 second or not at all, then poor lid elasticity is diagnosed and a lid-shortening procedure may be indicated. The patient also should be assessed in the lateral position to determine the relative globe to orbital-rim position. A prominent globe and recessed orbital rim predisposes the patient to the potential for postoperative lid malposition. This relationship is known as the negative vector in that the line drawn from the midpupil to the orbital rim on lateral view falls backward from superior to inferior (Fig. 4-5). If a lower lid is tightened in this situation, the lid may actually assume a worse, or lower, position, like an obese man’s belt slipping further down his paunch when the belt is cinched tighter. The mnemonic “big eyes, big trouble” is a worthy phrase that the prudent facial aesthetic surgeon should always heed. A careful ophthalmologic history is also critical (e.g., history of dry eyes, ocular surgery, glaucoma, or prior blepharoplasty). These are all important clues to establish the patient’s candidacy for elective eyelid surgery.
test the resilience of the lower lid. The lower lid is pinched between the index finger and thumb and pulled away from the globe. If the lid returns to contact the globe after 1 second or not at all, then poor lid elasticity is diagnosed and a lid-shortening procedure may be indicated. The patient also should be assessed in the lateral position to determine the relative globe to orbital-rim position. A prominent globe and recessed orbital rim predisposes the patient to the potential for postoperative lid malposition. This relationship is known as the negative vector in that the line drawn from the midpupil to the orbital rim on lateral view falls backward from superior to inferior (Fig. 4-5). If a lower lid is tightened in this situation, the lid may actually assume a worse, or lower, position, like an obese man’s belt slipping further down his paunch when the belt is cinched tighter. The mnemonic “big eyes, big trouble” is a worthy phrase that the prudent facial aesthetic surgeon should always heed. A careful ophthalmologic history is also critical (e.g., history of dry eyes, ocular surgery, glaucoma, or prior blepharoplasty). These are all important clues to establish the patient’s candidacy for elective eyelid surgery.
Besides evaluating the patient for possible eyelid surgery, the surgeon should recall the benefit that botulinum toxin alone may provide in the younger patient, who only exhibits rhytidosis during animation. Please refer to Chapter 8 for a detailed discussion of this treatment modality. Lower-lid resurfacing (CO2 laser or trichloroacetic acid [TCA] peel) also may be frequently incorporated with lower-lid surgery to efface fine rhytidosis.
Midfacial Rejuvenation
One of the most challenging areas in facial rejuvenation surgery is the aging midface. Several approaches have been advocated to address the midface: laterally via a deep-plane rhytidectomy incision, superiorly via a lower-eyelid incision, and supero-laterally via a temporal-brow incision.4, 5, 6 and 7 Despite these varied options, enthusiasm for these procedures has been tempered by the potential complications of each technique. The favored plane of dissection that unites these disparate approaches is subperiosteal, in which the malar fat pad and orbicularis-oculi muscle may be elevated as a unit. Since 1996, the senior author has performed a midface lift via the temporo-parietal browlift incision. However, reluctance has been noted in the literature to endorse this approach fully because of perceived concomitant morbidity. Protracted dissection time, risk to the frontal branch of the facial nerve, temporal wasting, and unnatural elevation of the lateral canthus all have been cited as drawbacks to this surgical approach to the midface.9,10 Because of these touted shortcomings, the authors critically reviewed the technique, outcome, and complications in an objective scientific study that revealed little morbidity combined with dramatic improvement.11
The midface may be an elusive entity to some but may be simply defined as the facial zone that overlies the malar eminence. As one ages, two principal pathologies contribute to an unattractive midfacial appearance: draping of the orbicularis-oculi muscle (festooning) and malar-fat ptosis (malar bagging). These two entities may appear indistinguishable at first glance, because they both manifest as unsightly bulges in the cheek region. However, orbicularis redundancy and ptosis may be effaced when the patient squints and contracts the muscle: This finding may not always be evident. Malar fat descent usually does not respond to contraction of the orbicularis-oculi muscle. This distinction between festooning and malar bagging however may be a bit arcane, because the surgical treatment for both is essentially the same, a midface lift.
INTRAOPERATIVE CONSIDERATIONS: TECHNIQUE AND SALIENT TECHNICAL POINTS
A Jessner’s/TCA peel serves as an effective adjunct for rejuvenation for fine rhytidosis of the lower lid without significant lower-lid redundancy (Figs. 4-6 and 4-7). The peel is performed first, because the patient should be under no or minimal sedation during this part of the procedure. In
addition, the patient should be positioned upright during the peel (inclined about 60 degrees). A detailed review of technique may be found in Chapter 9. CO2 laser resurfacing may be required if deeper etched lines are present, so long as the patient is amenable to the longer recovery period (upward of 3 months versus 2 weeks for the peel). Laser resurfacing may be undertaken before or after blepharoplasty; however, the authors routinely elect to perform laser ablation at the end of all surgical intervention. The surgeon should be extremely wary about performing additional skin excision after lower-lid resurfacing, because the risk of ectropion or vertical lid shortening is increased. After resurfacing, the lid continues to undergo some contraction and may pull away from the globe even without skin removal. The inexperienced surgeon is advised to wait several weeks if uncertain about the extent of additional skin excess and to undertake a pinch of skin as needed in the office setting at this later date.
addition, the patient should be positioned upright during the peel (inclined about 60 degrees). A detailed review of technique may be found in Chapter 9. CO2 laser resurfacing may be required if deeper etched lines are present, so long as the patient is amenable to the longer recovery period (upward of 3 months versus 2 weeks for the peel). Laser resurfacing may be undertaken before or after blepharoplasty; however, the authors routinely elect to perform laser ablation at the end of all surgical intervention. The surgeon should be extremely wary about performing additional skin excision after lower-lid resurfacing, because the risk of ectropion or vertical lid shortening is increased. After resurfacing, the lid continues to undergo some contraction and may pull away from the globe even without skin removal. The inexperienced surgeon is advised to wait several weeks if uncertain about the extent of additional skin excess and to undertake a pinch of skin as needed in the office setting at this later date.
Instrumentation and Equipment
Basic Soft-Tissue Instrument Set
Army-Navy retractors (2)
#3 knife handles (2)
Tonsil clamp
Medicine glass (1)
Suction, 10 French
Small double-pronged hook retractors (2)
Large double-pronged hook retractors (2)
Single hooks (2)
Bayonet forceps (for bipolar cautery)
Brown-Adson forceps (2)
Toothed Adson forceps
Bayonet toothed forceps
Bishop-Harmon toothed forceps
Castro-Viejo toothed forceps
Towel clip
Curved Mayo scissors
Medium Metzenbaum scissors
Serrated scissors
Tenotomy scissors
Iris scissors
Small curved sharp scissors
Needle holders (with scissors built-in) (2)
Needle holders (without scissors) (2)
Straight hemostats (2)
Curved Crile clamps (2)
Curved plane Crile clamps (2)
Converse retractor
Bowl
Freer elevator
(Note: These instruments constitute the basic instruments used on most major facial procedures. Other instrument lists that include a “Basic Soft-Tissue Instrument Set” refer to the preceding catalog of equipment.)
Instrumentation/Equipment for Brow/Midface Lift
Prep Stand:
Nonsterile gloves
10-cc syringe (2), 27-gauge (11/4 inch long) needle (2) with lidocaine 1% and 1:100,000 epinephrine
Hair comb
1/2″ Micropore tape (to bind hair)
Surgical marking pen
Instruments:
Basic soft-tissue instrument set (see the preceding)
Bovie handpiece and tip
Three curved, ebonized brow elevators:
Small, flat dissector
Large, flat dissector
Round dissector
Sutures:
CV-3 Gore-Tex,* Th-26 needle
Other Supplies:
Skin stapler
Laparotomy pads
10-cc syringe (2), 27-gauge (11/4 inch long) needle (2) with lidocaine 1% and 1:100,000 epinephrine
Dressing:
3″ Conforming gauze bandage, or Kling (Johnson & Johnson, New Brunswick, NJ) (3)
Cotton padding
Bacitracin ointment in 5-cc syringe
1″ clear tape
Scissors
Instrumentation/Equipment for Blepharoplasty/Ptosis Repair
Prep Stand:
Nonsterile gloves
1-cc tuberculin syringe (2), 27-gauge (11/4 inch long) needle (2) with lidocaine 1% and 1:50,000 epinephrine
Bowl with eye pads (2) soaked in iced saline
Surgical marking pen
Instruments:
Basic Soft-Tissue Instrument Set
Allis clamp
Castro-Viejo needle holder
Jaeger plate
Hand-held hot-tip wire-loop cautery
Bipolar cord and handpiece
Sutures:
6-0 silk, P-1(P-10, PRE-1) [C1] <EDR-1>** needle (traction suture)
7-0 nylon, P-1 (P-10, PRE-1) [C1] <EDR-1> needle (for wound closure)
5-0 polydioxanone P-3 (P-13, PRE-2) <RE-3>(for ptosis repair)
4-0 polydioxanone PS-3 (P-11, PRE-3) [PC-34] (for an extended skin-muscle dissection to tack the flap to the lateral-canthal periosteum)
Other Supplies:
Steri-Strips (3M, St. Paul, MN) (to hold medial end of lower blepharoplasty suture in place)
Cotton-tipped applicators
Dressing:
Bacitracin ointment
Aquaphor ointment (for lower-lid resurfacing)
N-terface occlusive dressing (for laser resurfacing)
Instrument/Equipment for Malar Augmentation
Prep Stand:
10-cc syringe (2), 27-gauge (11/4 inch long) needle (2) with lidocaine 1% and 1:100,000 epinephrine
Instruments:
Basic Soft-Tissue Instrument Set
Other Supplies:
ePTFE (Gore-Tex) Malar Implant (small, medium, or large)
Dressing:
None
A transconjunctival approach is preferred for the majority of lower-lid blepharoplasties, because the integrity of the orbicularis oculi is maintained, and an external incision is avoided if no skin redundancy exists. Both the skin and muscle sling act to retain the lower-lid position against the globe, and a skin-muscle flap predisposes to a higher likelihood of lid malposition. If a browlift is carried out concomitantly, a transconjunctival blepharoplasty should be performed first, because the brow suspension increases lower-lid tension and makes transconjunctival entry particularly arduous.
The first step in performing a lower-lid blepharoplasty involves proper local anesthetic placement, which is achieved with a mixture of 1% lidocaine to 50,000 epinephrine. The local anesthesia is injected into the conjunctiva in the medial, central, and lateral aspects in the preseptal plane while the conjunctiva is exposed with a Desmarres or wide, two-pronged retractor. Additional local anesthesia may be infiltrated into the lower-lid skin as well if skin excision is planned. The patient should be under sedation or general anesthesia for the infiltration of anesthesia as well as for the actual procedure because transconjunctival surgery may elicit patient discomfort. The anesthesiologist also should be advised that ocular lubrication should not be instilled before a transconjunctival blepharoplasty because the ophthalmic gel tends to obscure the surgical field.
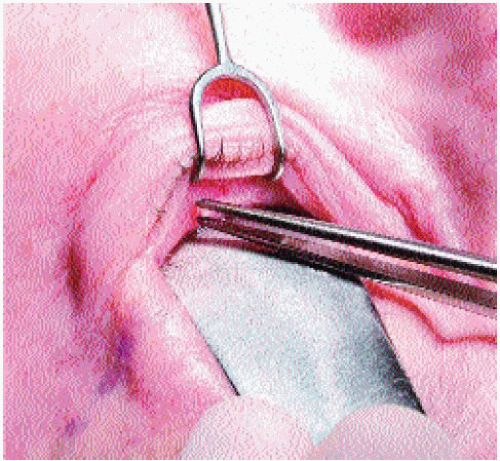
After 10 minutes are allowed to transpire for maximal hemostasis, the Desmarres or wide, two-pronged retractor is properly positioned to retract the lower lid by the first assistant (who is stationed to the right of the surgeon and patient) while the surgeon (above the head of the patient) gently protects the globe and applies countertraction with a Jaeger plate. With a bipolar cautery, the surgeon seals the superficial conjunctival vessels before transconjunctival entry (Fig. 4-8). A hand-held, hot-tip, wire-loop cautery is used to incise the conjunctiva just past 5 mm from the lid margin (i.e., beyond the edge of the tarsal border) (Fig. 4-9).† The
Jaeger plate is removed; the inferior aspect of the transected conjunctival border (i.e., the side closest to the surgeon) is grasped with a Bishop forceps; and a 6-0 silk suture with a P-1 needle is passed through the conjunctiva so that the conjunctival flap can be retracted upward over the globe for protection and retraction (Fig. 4-10). The silk loop is secured with a hemostat and placed on the patient’s forehead resting on a moist 4 4 gauze to provide adequate tension on the conjunctival flap.
4 gauze to provide adequate tension on the conjunctival flap.
Jaeger plate is removed; the inferior aspect of the transected conjunctival border (i.e., the side closest to the surgeon) is grasped with a Bishop forceps; and a 6-0 silk suture with a P-1 needle is passed through the conjunctiva so that the conjunctival flap can be retracted upward over the globe for protection and retraction (Fig. 4-10). The silk loop is secured with a hemostat and placed on the patient’s forehead resting on a moist 4
 4 gauze to provide adequate tension on the conjunctival flap.
4 gauze to provide adequate tension on the conjunctival flap.The surgeon again picks up the inferior (proximal) conjunctival flap with a pair of Bishop forceps carefully observing for the wisp-like adhesions that traverse vertically from the orbicularis oculi (anteriorly) to the septum (posteriorly) and that define the preseptal plane (Fig. 4-11). The dissection is carried out with the hot-tip, hand-held cautery. The authors prefer a preseptal dissection because of a more controlled and natural dissection plane than afforded by postseptal entry. The preseptal dissection plane is defined as the natural cleavage plane that separates the septum and postseptal fat posteriorly from the orbicularis-oculi muscle anteriorly (Fig. 4-12). (Conversely, a postseptal dissection involves direct entry into the postseptal fat without defining the orbital-septal plane.)
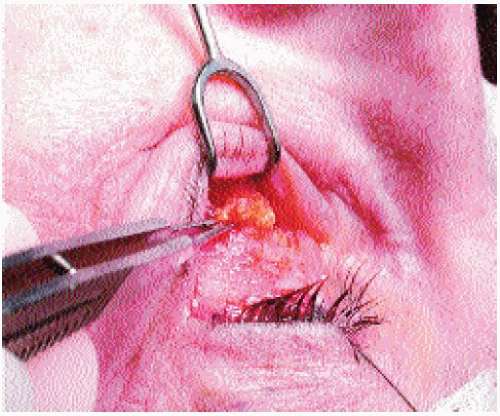
A small puncture is made in the orbital septum over the medial-fat pocket with the hot-tip cautery, and the fat is gently teased out while the other hand applies gentle pressure on the globe (Fig. 4-13). The amount of fat that protrudes is correlated with the preoperative images that should be prominently displayed in the operating suite for reference. These standardized preoperative portraits, particularly the close-up frontal view, act as indispensable guides because the supine patient reveals little information about the amount of herniated fat that is present. If any arcade of vessels traverse the fat to be removed, they can be teased back into the globe with a cotton-tipped applicator rather than clamped and
cauterized. This maneuver may reduce the risk of postoperative retroseptal hemorrhage. No additional local anesthesia is administered to the dissected fat: The authors believe that the few seconds that transpire between anesthetic injection and fat removal do not permit sufficient time for the local anesthesia to function properly. (If the reader should elect to inject local anesthesia postseptally, he or she is reminded of the necessity to use only plain lidocaine to avoid the risk of vasospasm and consequent visual loss.)
cauterized. This maneuver may reduce the risk of postoperative retroseptal hemorrhage. No additional local anesthesia is administered to the dissected fat: The authors believe that the few seconds that transpire between anesthetic injection and fat removal do not permit sufficient time for the local anesthesia to function properly. (If the reader should elect to inject local anesthesia postseptally, he or she is reminded of the necessity to use only plain lidocaine to avoid the risk of vasospasm and consequent visual loss.)
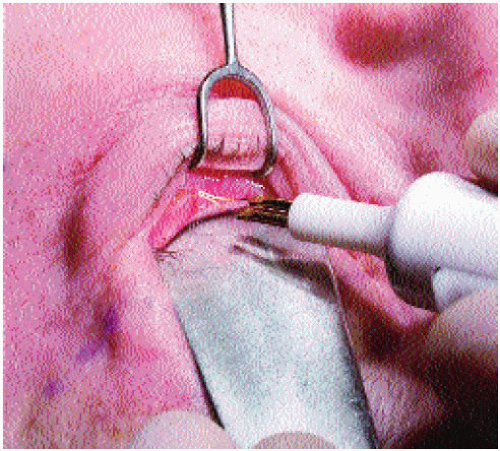
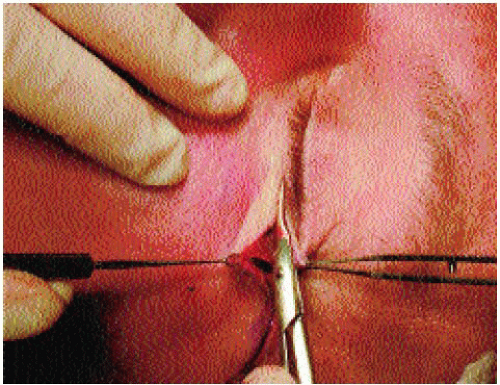
The dissected adipose then is clamped with a hemostat and held in position by the surgical assistant (Fig. 4-14). The surgeon applies bipolar cautery along the clamp (Fig. 4-15) and then excises the fat along the clamp with a pair of
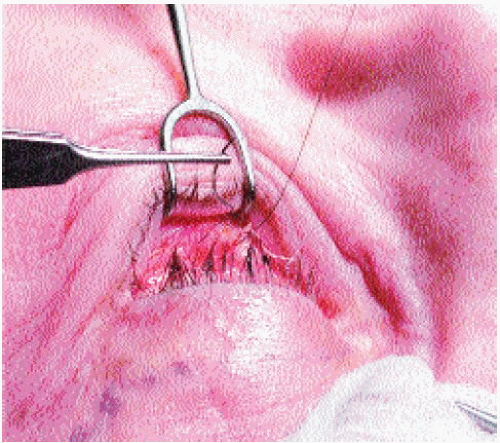
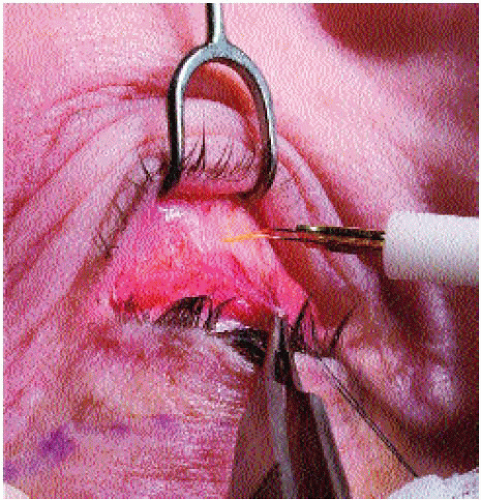
tenotomy scissors (Fig. 4-16). Additional bipolar cautery is applied to the adipose cuff that remains along the hemostat after fat excision (Fig. 4-17). Prior to the assistant’s release of the hemostat tines, the surgeon grasps the remaining fat below the clamp with a pair of Bishop forceps. As the clamp is released, the surgeon carefully observes for any signs of uncontrolled hemorrhage, which is promptly addressed with bipolar cautery (Fig. 4-18). The reader is also reminded about the risk of inadvertent injury to the inferior-oblique muscle, which separates the medial-fat from the central-fat pockets. The surgeon then progresses laterally to the central-fat and lateral-fat pockets in a similar fashion, as dictated by the patient’s pathology. The conjunctiva is left to heal without suture closure. If any skin redundancy is evident, an Allis clamp is used to pinch the excess skin about 1 mm from the lid margin while carefully observing for eyelash eversion. The amount of skin removed is dictated by eyelash position, where the eyelashes should just begin to assume a perpendicular orientation to the skin when the skin is grasped by the Allis. The crimped excess skin then is removed with Bishop forceps and fine iris scissors. Any irregular skin edges are not rectified by additional corrective trimming, because this predisposes to vertical lid shortening and is simply unnecessary for favorable healing. Hemostasis is obtained with hot-tip cautery, and the wound edges are approximated with a running, nonlocking 7-0 polypropylene suture with the medial extent fastened to the skin with a Steri-Strip rather than tied. Leaving the medial end untied allows edema to loosen the suture appropriately and facilitates suture removal. Sutures are removed at 6 days postoperatively.
tenotomy scissors (Fig. 4-16). Additional bipolar cautery is applied to the adipose cuff that remains along the hemostat after fat excision (Fig. 4-17). Prior to the assistant’s release of the hemostat tines, the surgeon grasps the remaining fat below the clamp with a pair of Bishop forceps. As the clamp is released, the surgeon carefully observes for any signs of uncontrolled hemorrhage, which is promptly addressed with bipolar cautery (Fig. 4-18). The reader is also reminded about the risk of inadvertent injury to the inferior-oblique muscle, which separates the medial-fat from the central-fat pockets. The surgeon then progresses laterally to the central-fat and lateral-fat pockets in a similar fashion, as dictated by the patient’s pathology. The conjunctiva is left to heal without suture closure. If any skin redundancy is evident, an Allis clamp is used to pinch the excess skin about 1 mm from the lid margin while carefully observing for eyelash eversion. The amount of skin removed is dictated by eyelash position, where the eyelashes should just begin to assume a perpendicular orientation to the skin when the skin is grasped by the Allis. The crimped excess skin then is removed with Bishop forceps and fine iris scissors. Any irregular skin edges are not rectified by additional corrective trimming, because this predisposes to vertical lid shortening and is simply unnecessary for favorable healing. Hemostasis is obtained with hot-tip cautery, and the wound edges are approximated with a running, nonlocking 7-0 polypropylene suture with the medial extent fastened to the skin with a Steri-Strip rather than tied. Leaving the medial end untied allows edema to loosen the suture appropriately and facilitates suture removal. Sutures are removed at 6 days postoperatively.
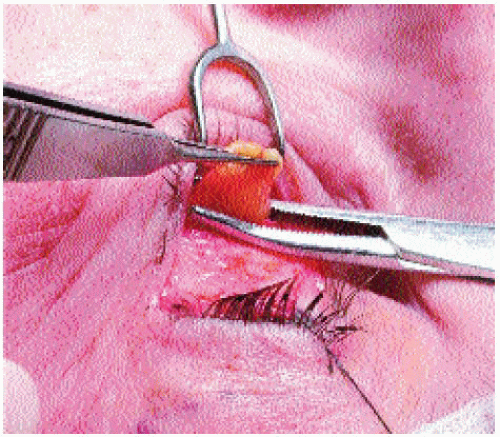 FIGURE 4-14. Lower Transconjunctival Blepharoplasty, Step 7. The dissected adipose is clamped with a hemostat and held in position (away from the skin) by the assistant. |
 FIGURE 4-15. Lower Transconjunctival Blepharoplasty, Step 8. The surgeon applies bipolar cautery along the clamp prior to excision of the excess adipose. |
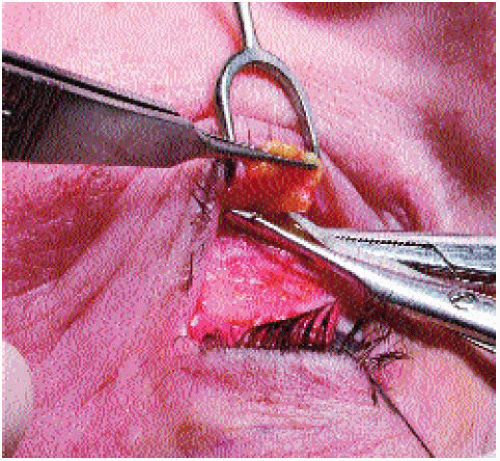 FIGURE 4-16. Lower Transconjunctival Blepharoplasty, Step 9. The excess fat is trimmed with a pair of tenotomy scissors. |
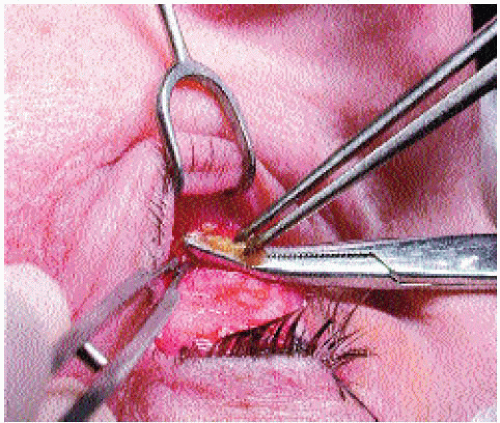 FIGURE 4-17. Lower Transconjunctival Blepharoplasty, Step 10. Additional bipolar cautery is applied to the adipose cuff that remains along the hemostat after fat excision. |
As mentioned, the transconjunctival approach remains the authors’ mainstay for lower-lid blepharoplasty. However, a skin-muscle flap is indicated in certain select conditions that favor this technique. If excessive lower-lid laxity or frank ectropion is present, then a lower-lid shortening procedure (e.g., tarsal strip) may be required. Alternatively, a lateral-canthal fixation suture may be used to suspend the lower lid sufficiently in proper position. Although a transconjunctival blepharoplasty may prevent the onset of postoperative lower-lid malposition, preexisting lower-lid malposition requires correction with a tarsal strip or lateral-canthal suspension. If a tarsal strip or lateral-canthal plication suture is required, then a skin-muscle flap is advised. Furthermore, if the patient suffers from malar descent (festooning or malar bagging) and declines a browlift/transbrow midface lift, then an extended skin-muscle flap may be undertaken instead. For any of these reasons, a skin-muscle type flap may be the approach of choice.
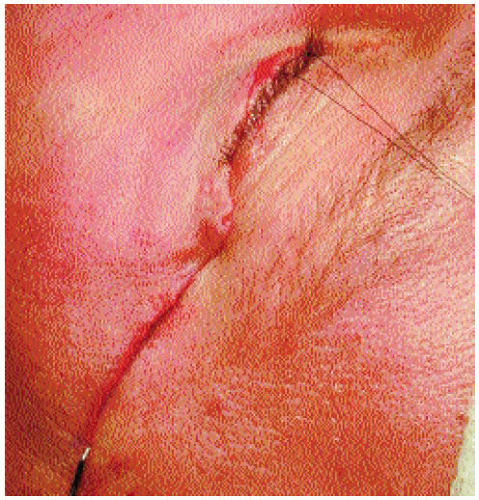
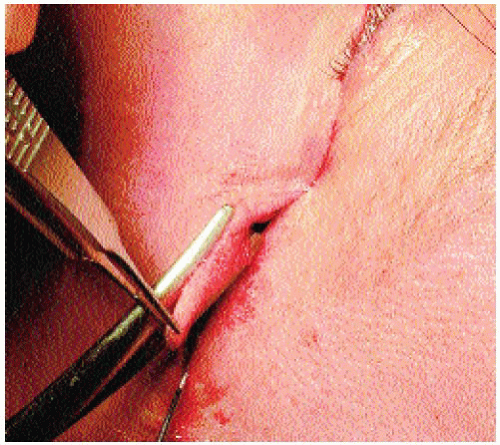
If an extended blepharoplasty is to be carried out, then an extended incision that follows a natural skin crease radiating from the lateral canthus should be marked out with a surgical marking pen. One percent lidocaine with 1:50,000 epinephrine is injected along the line of incision and inferiorly over the area of dissection. The appropriate 10 minutes of hemostatic time is allowed to transpire before the initial incision is made. A No. 15 Bard-Parker blade is used to make the first few millimeters of an incision approximately 1 to 2 mm from the inferior lid margin at the most lateral extent through both skin and muscle. A pair of iris scissors then are inserted through this incipient incision and gently spread to develop the plane of dissection below the skin-muscle flap from lateral to medial. One blade of the scissors then is inserted into the incision with the other blade remaining externally, and in this way the incision is opened laterally to medially as far as required but always lateral to the medial punctum (to minimize risk of medial-canthal web formation) (Fig. 4-19). The bleeding muscle edge then is cauterized with a hot-tip hand-held electrocautery or a bipolar cautery device.
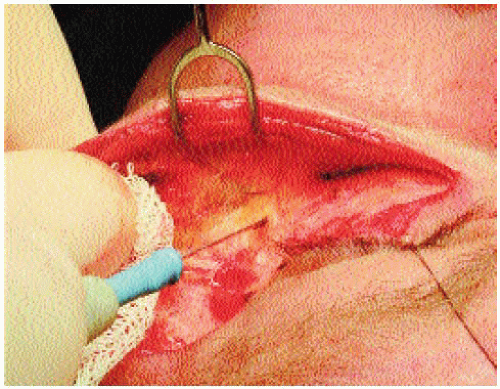
A 6-0 silk suture is passed through the superior aspect of the incision and clamped with a hemostat in order to retract the lower lid upward, protecting the globe and providing countertraction to the elevated skin-muscle flap. Bishop forceps or a wide, double-pronged retractor then is used to retract the skin-muscle flap inferiorly while the hand-held or monopolar cautery dissects the skin-muscle flap from the underlying orbital septum. This flap is carried downward onto the midface under the malar bag/festoon if an extended lower-lid blepharoplasty is intended (Fig. 4-20). If pseudoherniation
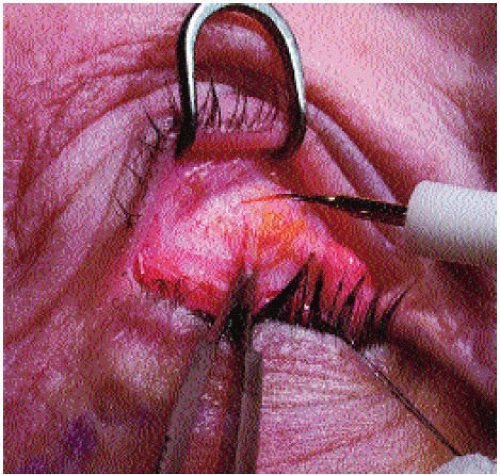
of fat exists, then the orbital septum is entered and the fat clamped and removed as described earlier for the transconjunctival approach. If an extended blepharoplasty is undertaken to efface a malar bag/festoon, then the malar bag/festoon is suspended to the lateral orbital rim using a 4-0 polydioxanone (PDS [Ethicon, Cornelia, GA], Maxon [U.S. Surgical/Davis & Geck, Norwalk, CT]) or CV-4 Gore-Tex suture (Figs. 4-21, 4-22, and 4-23). A single pronged hook is placed into the lateral aspect of the incision to provide proper tension and alignment prior to skin-flap excision (Fig. 4-24). Any excessive skin-muscle flap then is trimmed with curved serrated iris scissors erring on the conservative side to avoid unintended lid eversion and vertical shortening, especially medially (Fig. 4-25). The incision line then is reapproximated with a running, nonlocking 7-0 polypropylene suture. A lateral canthal suspension suture still should be considered for a standard skin-muscle blepharoplasty to lessen the probability of postoperative lid malposition. This suture is placed in a similar fashion as described for the extended technique but often with less vertical elevation. (The midface does not require suspension in this circumstance.)
of fat exists, then the orbital septum is entered and the fat clamped and removed as described earlier for the transconjunctival approach. If an extended blepharoplasty is undertaken to efface a malar bag/festoon, then the malar bag/festoon is suspended to the lateral orbital rim using a 4-0 polydioxanone (PDS [Ethicon, Cornelia, GA], Maxon [U.S. Surgical/Davis & Geck, Norwalk, CT]) or CV-4 Gore-Tex suture (Figs. 4-21, 4-22, and 4-23). A single pronged hook is placed into the lateral aspect of the incision to provide proper tension and alignment prior to skin-flap excision (Fig. 4-24). Any excessive skin-muscle flap then is trimmed with curved serrated iris scissors erring on the conservative side to avoid unintended lid eversion and vertical shortening, especially medially (Fig. 4-25). The incision line then is reapproximated with a running, nonlocking 7-0 polypropylene suture. A lateral canthal suspension suture still should be considered for a standard skin-muscle blepharoplasty to lessen the probability of postoperative lid malposition. This suture is placed in a similar fashion as described for the extended technique but often with less vertical elevation. (The midface does not require suspension in this circumstance.)
 FIGURE 4-21. Lower (Extended Skin-Muscle) Blepharoplasty, Step 3. The malar fat pad is identified and grasped with fine forceps for suspension to the lateral orbital rim. |
 FIGURES 4-22 and 4-23. Lower (Extended Skin-Muscle) Blepharo plasty, Step 4. A 4-0 polydioxanone or 4-0 Gore-Tex suture is used to suspend the malar fat pad to the lateral orbital periosteum. |
If a tarsal strip is to be conducted, then this may be performed after the skin-muscle flap has been properly elevated and in lieu of the described suspension suture. A pentagonal wedge (or Kuhnt-Szymanowski) is not preferred for risk of lid notching. The tarsal-strip procedure is briefly reviewed herein (Fig. 4-26). A lateral canthotomy is undertaken, followed by an inferior cantholysis. After an inferior cantholysis, the lower lid should be freely detached from the globe. The freed lower lid should be retracted supero-laterally so that the lower lid crosses 1 mm above the inferior limbus. The amount of lid excess can be determined with the lid retracted in this way, and the corresponding anterior lamella (orbicularis oculi and skin) should be divided sharply from the posterior lamella to expose the tarsus. The excessive conjunctiva is abraded away with the belly of the No. 15 blade to create the tarsal strip. The tarsal strip then is suspended to its physiologic locus (at Whitnall’s tubercle) through the periosteum with a double-armed 5-0 white Mersilene suture in a vertical mattress configuration. The authors have noted that actual suspension to Whitnall’s tubercle, located in the inner aspect of the orbital rim, causes undue prolonged eyelid distortion and may be avoided by simply tacking the tarsal strip to the anterior-medial border of the orbital rim instead. The excessive tarsal strip then is trimmed away. The lateral canthus is reapproximated to its correct anatomic location using 7-0 nylon. Excess skin and muscle are removed, principally in the lateral aspect of the wound (the same technique as advocated for an extended skin-muscle flap) tapering medially. Skin closure then is completed with a running 7-0 nylon suture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree