Cutaneous Rejuvenation
Samuel M. Lam
Edwin F. Williams III
Although the principal focus of this book is surgical, incision-based, intervention for the aging face, a thorough understanding of cutaneous resurfacing modalities also must be sought to offer the patient the most complete rejuvenative regimen. Patients who only exhibit actinic damage, such as superficial dyschromias and textural skin changes, without actual ptosis of tissues are more suitable candidates for resurfacing than traditional lifting procedures. In addition, resurfacing may be effectively combined with lifting procedures for patients who exhibit both tissue ptosis and photodamage if flap integrity may be ensured (e.g., with subperiosteal elevation of the brow the skin may be safely resurfaced concurrently) or deferred for several months until flap vascularity is restored.
The facial aesthetic surgeon must not only master the technical aspects of some of the myriad resurfacing modalities that abound but know when to select a particular technique and further when to combine techniques to achieve maximal benefit for the patient. The authors stress the importance of careful selection of a few, reliable techniques that have proven efficacy rather than the quixotic quest to implement all of the techniques available today.
As important as technical mastery is the commensurate understanding of the complicated and often confusing postoperative management of the resurfaced patient, which involves an intensive, almost daily encounter to guide the patient successfully through the process. To date, no text has lucidly revealed this aspect of patient care in a pragmatic, detailed, and systematic fashion. Complications such as dermatitis and (rarely) scarring during the postoperative period may arise and must be swiftly identified and treated to minimize adverse outcomes.
This chapter concludes with a primer on basic skin care and rejuvenative topical agents, such as tretinoin-based products, for those patients who are not yet ready for any surgical therapy or those who would like to maintain the longevity of their surgical result. Physicians often relegate this type of care to the aesthetician and disavow the necessity to learn more about skin care. However, the physician should be partly responsible for this knowledge at minimum, because he or she must decide when it is safe for the resurfaced patient to use camouflaging products and effectively answer simple queries regarding which products may be appropriate for the newly resurfaced skin.
PREOPERATIVE CONSIDERATIONS: PATIENT SELECTION AND RELEVANT ANATOMY
Before considering what technique would be appropriate for a particular patient, the surgeon must have a well-structured understanding of the types of resurfacing modalities available. Basically, cutaneous resurfacing may be divided into two principal categories: nonablative and ablative therapy. The former represents a recent advance in resurfacing that promotes dermal remodeling via collagen synthesis without any epidermal effacement. Accordingly, the epidermis is entirely untouched during nonablative therapy; therefore, no benefit is obtained for the photodamaged outer skin. Instead, limited fine-to-moderate rhytidosis may be addressed with multiple treatment sessions over a period of several months to permit sufficient time for collagen-dermal remodeling to occur. Similarly, because the epidermal layer is maintained intact, the patient experiences no downtime and is subjected only to a brief, painless treatment session that leaves no residual edema, ecchymosis, or erythema. Again, it should be emphasized that this new technique must be selectively employed in the suitable patient with the individual fully cognizant of the inherent limitations for facial rejuvenation.
The authors have investigated the potential benefit of this newer technique in a blinded, prospective, histologic analysis using a porcine model.1 The results of this study were quite revelatory: The histologic specimens harvested from the nonablative, pulsed-dye laser-treated skin demonstrated statistically significant collagen remodeling in both a quantitative (collagen band width, nuclei per high-powered field) and qualitative (overall dermal thickness) fashion as compared with untreated skin. The dermal depth could not be quantitatively measured because the thickness exceeded the punch-biopsy instrument in all the laser-treated (both ablative and nonablative) skin. Further, the degree of collagen remodeling favorably compared with that of ablative, carbon dioxide laser-treated areas. However, this preliminary
data must be cautiously assessed, as these results were obtained in an animal model; human clinical trials are warranted to establish the precise role that nonablative therapy should play in facial rejuvenation.
data must be cautiously assessed, as these results were obtained in an animal model; human clinical trials are warranted to establish the precise role that nonablative therapy should play in facial rejuvenation.
The early clinical trials have been somewhat equivocal. Fitzpatrick’s study showed a statistically significant aesthetic improvement in patients’ hemifaces that were treated with a nonablative, pulsed-dye laser as compared with a placebocontrolled (cryogen spray alone) side.2 All photographic analyses were conducted in a blinded, prospective method. These findings were further corroborated with histologic samples taken from each side that revealed significant collagen synthesis on the treated side compared with the controlled, untreated side. Despite histologic improvement, one study showed limited clinical patient satisfaction.3 However, other studies have corroborated the benefit of nonablative techniques for mild to moderate skin pathologies.4, 5, 6, 7 and 8
The authors have found that the best results obtained with this technology may be obtained in patients with mild to moderate fine rhytidosis, particularly in the periocular region (e.g., crow’s feet at the lateral canthus and crepelike wrinkles that traverse below the eye). The ideal candidate for this treatment strategy is the younger individual (in his or her thirties) who exhibits minimal photodamage (dyschromias and other epidermal damage) with fine, periocular rhytidosis. These patients are also very well suited to botulinum toxin (BTX) injections, which may be used in combination or independently of nonablative laser therapy. Patients who exhibit more marked rhytidosis, actinic damage, or ptotic tissues do not significantly benefit from this technique and should be dissuaded from undertaking nonablative therapy.
Cutaneous, ablative resurfacing represents the more traditional method of facial skin rejuvenation in which the entire outer layer of the epidermis is removed along with a partial thickness of the underlying dermis to effect a favorable aesthetic result. Ablative resurfacing may be undertaken via three principal methods: mechanical abrasion, chemical exfoliation, and laser therapy. Each modality has its own unique characteristic benefits and drawbacks, and at times combination of these techniques may offer the patient the most favorable means of obtaining the desired objective. Mechanical abrasion may range from the least invasive microdermabrasion (which effectively acts as a nonablative method of facial rejuvenation) to the more aggressive technique of dermasanding to fully ablative dermabrasion. The latter offers precise control of uneven cutaneous contour and texture and is particularly well suited in the acne-scarred skin. Although acne scarring does not strictly fall within the confines of the topic of the aging face, a discussion of this clinical scenario is conducted, because treatment of this pathology clearly illustrates the role of effective combined resurfacing. Similar to the varied mechanical methods of resurfacing, chemical peeling agents differ in their potency from the light glycolic and Jessner’s solutions to the more invasive higher-strength trichloroacetic acid (TCA) and phenol mixtures. Thirty-five percent TCA and phenol prove their incontestable benefit to reverse significant photoaged skin with moderate rhytidosis. Laser therapy for facial rejuvenation may be entirely nonablative (as discussed in the preceding) via laser and light therapies intended for this purpose, such as the intense pulsed-light devices or the pulsed-dye laser adjusted to lower fluences. Alternatively, traditional ablative lasers such as the CO2 laser efface the epidermis to effect the desired rejuvenation and may be more appropriate for severely photodamaged skin. The other ablative laser that has been widely advocated, the Erbium:YAG (Er:YAG) laser, has theoretical advantages over the CO2 laser, including less thermal injury and more specific collagen photothermolysis, but has fallen short in practical usage because of poor hemostasis and limited effect. Therefore, the authors do not advocate use of this particular type of laser whether as an adjunct to the CO2 laser or alone, as there is no real perceived advantage that the Er:YAG offers over comparable chemical peeling.
However, any ablative resurfacing modality carries with it considerable morbidity, which includes risk of hyperpigmentation and hypopigmentation, dermatitis, perioperative edema, protracted erythema, milia and acne outbreaks, physical discomfort, an involved cleaning and occlusive regimen, need for solar protection, and the most dreaded outcome, potential scarring. Despite these limitations, ablative resurfacing achieves remarkable success in rejuvenating severely photodamaged skin and is still a mainstay of therapy for those patients who require intensive rejuvenation and who are willing to accept the expected recovery period. All patients are thoroughly counseled that the postoperative period will be complex and should fully comprehend that their appearance will be analogous to that of a burn victim. Patients are informed of their expected postoperative appearance at the outset so that they may be psychologically well equipped to handle the temporary disfigurement. Proper preoperative counseling is an essential element to successful postoperative care.
The various resurfacing techniques that are available today offer the aesthetic facial surgeon an unprecedented ability to achieve a desired cosmetic outcome. However, every resurfacing technique should not be viewed as flawless or universal in its clinical benefit. The reader is advised to avoid a “compartmentalized” perspective in which every cutaneous problem is solved by a single technique. As addressed in the following, each modality has inherent drawbacks as well as distinct advantages, which offer the patient the optimal result if appropriately combined with other resurfacing techniques.
An important consideration is that resurfacing cannot address all cutaneous problems, namely, skin redundancy or volume excess. If the patient presents with dermatochalasis, or excessive upper-eyelid skin, the surgeon should remove
the redundant skin to restore a youthful countenance. Similarly, brow ptosis or cheek jowling should be corrected with a brow lift or rhytidectomy, respectively. Steato-blepharon, or pseudoherniation of fat of the eyelids, is amenable to fat removal or repositioning. Deep or fine rhytids, which are the product of continuous facial motion, may be better served with a paralytic agent (e.g., botulinum toxin). However, the authors admit that ablative (and even nonablative) resurfacing has been observed to yield a more tightened facial appearance by virtue of the collagen stimulation.
the redundant skin to restore a youthful countenance. Similarly, brow ptosis or cheek jowling should be corrected with a brow lift or rhytidectomy, respectively. Steato-blepharon, or pseudoherniation of fat of the eyelids, is amenable to fat removal or repositioning. Deep or fine rhytids, which are the product of continuous facial motion, may be better served with a paralytic agent (e.g., botulinum toxin). However, the authors admit that ablative (and even nonablative) resurfacing has been observed to yield a more tightened facial appearance by virtue of the collagen stimulation.
When deciding which resurfacing technique to employ, one should reflect on three key guidelines: (a) the subunits of the face; (b) the depth of the facial pathology; and (c) the Fitzpatrick skin grade of the patient.9 The face may be divided into so-called subunits (perioral, periocular, nasal, brow, and cheek), which tolerate different resurfacing modalities to varying degrees. For example, the lower eyelid tends to withstand the pigmentary ablation of the CO2 laser better than the jaw line. It has been noted that the line of demarcation between hypopigmented face and pigmented neck may become more pronounced over the years as the facial skin continues to undergo some progressive depigmentation. Therefore, full-face laser resurfacing should be undertaken with caution, especially considering the protracted erythema that the patient must bear. The depth of the facial lesion (scar, rhytid, etc.) should be considered when deciding what resurfacing modality may be best suited. For example, deep acne scarring may be more effectively addressed with dermabrasion than TCA peel. Finally, the patient’s Fitzpatrick score has significant impact on the short- and long-term tendency toward hyperpigmentation and hypopigmentation. Accordingly, laser resurfacing should be used with greater restraint in darker-skinned individuals, especially when considering the greater disparity in color (lighter face and darker neck) that may arise along the jaw line.
Generally speaking, any kind of resurfacing should not be carried out concurrently with a surgical procedure in which the resurfaced area is undermined. However, the authors have achieved favorable results with minimal morbidity in select patients (nonsmokers, nondiabetics) in which a shorter, cutaneous flap is dissected and a lighter end point of the chemical peel (less frosting) is achieved or only a single CO2 pass is undertaken. In addition, the peel and laser are feathered gently toward the distal aspect of the flap to limit risk of flap compromise. However, caution always must be exercised if combined surgery and resurfacing are performed and may not be advisable, especially to the neophyte surgeon. As a rule, patients who have undergone a surgical undermining procedure should wait at least a period of 9 months before being resurfaced. Similarly, a patient who recently underwent aggressive resurfacing procedure should expect to wait 9 months before a surgical undermining procedure.
Besides an assiduous assessment of the patient’s aesthetic deficits, the surgeon must review a pertinent clinical history that may adversely contribute to the patient’s outcome. Clearly, conditions that inhibit proper wound healing should be assessed, which include prior history of keloid or hypertrophic scarring, tobacco use (of any kind), diabetes mellitus, and active and ongoing acne. Of note, the authors have not witnessed any adverse scarring even in patients who have a history of hypertrophic or keloid scarring if resurfacing is confined to the face, because the unique healing properties of the face limit the potential for these exuberant forms of scarring. Also, if the patient continues to engage in daily and protracted sun exposure, this activity, especially in the postoperative period, should be highly discouraged for risk of poor healing, scarring, dermatitis, and marked hyperpigmentation. Patients who have considerable bodily actinic damage should be advised that their rejuvenated face might not appropriately match the advanced nature of the sun-damaged skin of their body; and this disparity might prove troublesome to them if proper preoperative advice is not delivered. As is well known, the most significant medicine that is an absolute contraindication to ablative resurfacing is use of isotretinoin (Accutane) for any duration over the prior year. The reduction of the pilosebaceous glands that this medication engenders predisposes the patient to the very real risk of uncontrolled scar formation. Also, patients who have undergone prior undermining of their skin (e.g., a rhytidectomy or brow lift) are at a slightly increased risk of scarring owing to injury to the regenerative pilosebaceous glands. The very rare cases of scarring that the authors have witnessed have all occurred in patients who have undergone a prior facial surgical procedure in which cutaneous undermining was undertaken. Nevertheless, the physician should not unduly frighten the patient regarding this limited risk but should remain vigilant in the postoperative period for this potential outcome.
As part of the preoperative regimen, an oral antiviral medication is commenced 2 days prior to the actual procedure if resurfacing is planned in the perioral region. If the patient manifests a herpetic outbreak despite prophylaxis (which is rare), he or she remains on the antiviral medication at twice the dosage for an additional week from the onset of the outbreak. Usually, herpetic lesions may be distinguished from acne or milia in the timing of onset (typically 6 to 7 days postoperative), characteristic clustering and vesicular nature of the lesions, and intense burning sensation in the affected areas. If the patient manifests these symptoms, the authors instruct the patient to contact the office immediately so that proper intervention may be initiated. Perioperative antibiotics that target the skin flora, such as cephalexin, are also routinely implemented in patients for a 1-week duration postoperatively although their proven efficacy may be debated. In the past, hydroquinone and retinoic acid were dispensed to the patient a few weeks prior to the planned procedure for daily topical application, but
this regimen has since been abandoned. Alster’s study of 100 prospectively evaluated and controlled patients showed no benefit of either agent in the reduction of postinflammatory hyperpigmentation—which corroborates the authors’ empirical observations. Her rationale for this lack of efficacy was attributed to the removal by the peel or laser of all superficial melanocytes that were treated by the preceding topical agents.10
this regimen has since been abandoned. Alster’s study of 100 prospectively evaluated and controlled patients showed no benefit of either agent in the reduction of postinflammatory hyperpigmentation—which corroborates the authors’ empirical observations. Her rationale for this lack of efficacy was attributed to the removal by the peel or laser of all superficial melanocytes that were treated by the preceding topical agents.10
Ideal Candidates for Resurfacing
Nonablative
Younger patient (thirties)
Fine periocular rhytidosis
Limited photodamage
Limited tissue ptosis (also consider adjuvant Botox)
Ablative
Chemical peel (Jessner’s/35% TCA)
Any age with epidermal photodamage
Mild to moderate rhytidosis
Limited perioral rhytidosis
Limited tissue ptosis
Laser resurfacing
Generally older patient with deeper rhytidosis not amenable to chemical peel (e.g., perioral or glabellar rhytidosis)
Consider limiting laser resurfacing to discrete subunits (best-tolerated areas are the periocular, perioral, and glabellar regions) because of risk of hypopigmentation, especially demarcated at the jaw line, and morbidity of laser resurfacing
Combined resurfacing for acne and rhinophyma
Patients understand the longer recovery time (several months of erythema)
Mechanical dermabrasion
Depressed surface irregularities (e.g., acne scarring)
Rhinophyma
In conjunction with scar revision (6 weeks after)
Deeper wrinkles (perioral) in lieu of laser resurfacing
Instrumentation and Equipment for Chemical Peel (Fig. 9-1)
Jessner’s Solution*
(Resorcinol 14 g, salicylic acid 14 g, lactic acid 14 cc, QS ethanol 100 cc)
35% TCA solution
100% Acetone (may be purchased at a local hardware store)
Cotton-tipped applicators
Cotton balls
Nonsterile gloves
Cooling fan
Balanced saline solution (for eye flush if chemical peel inadvertently enters the eye)
Intravenous Versed sedation (optional but recommended)
INTRAOPERATIVE CONSIDERATIONS: TECHNIQUE AND SALIENT TECHNICAL POINTS
Nonablative Laser Therapy (Pulsed-Dye Laser)
As mentioned, various devices that emit broadband light or, alternatively, true lasers, have been used as a nonablative instrument. The authors have had extensive experience with the pulsed-dye laser and have found that this type of laser has an unparalleled safety profile and is well tolerated by the patient (Fig. 9-2A,B). In addition, the pulsed-dye laser also may be used to eradicate superficial vascular ectasias, such as cherry angiomas or spider veins (Fig. 9-3). Because the epidermis should be protected during treatment, a cooling spray should be employed (20 ms duration, 20 ms prior to laser emission), which is equipped with Candela pulsed-dye laser models. In the cited animal study, the authors noted that the only variable that did not negatively affect collagen remodeling was the use of the cryogen spray, which did serve to limit the risk of epidermal hyperpigmentation. Therefore, cryogen spray is advocated in nonablative therapy. Increasing fluence, spot size, and pulse duration statistically affected the amount of collagen remodeling. Nevertheless, practically speaking, a safe parameter for nonablative laser resurfacing that virtually ensures limited to no ecchymosis, edema, or discomfort but still achieves a favorable clinical improvement is a 10-mm spot size, set at 4 J/cm2 with use of the cryogen spray.
Proper laser precautions should be observed (e.g., posted laser signs, eye protection, and trained staff). Both physician and staff should don appropriate laser goggles tailored to the 585- to 595-nm wavelength. Because the laser needs to pass in close proximity to the patients’ eyes to address the periocular
rhytids, it is advisable to have the physician hold the patients’ eyes firmly shut with the nondominant hand rather than use protective eyewear for the patient. The patient should be forewarned that the laser light is quite bright, especially when passed near the eye, even when the eye is completely closed. In addition, the patient may be gently startled by the cooling spray that immediately precedes laser delivery and should be informed of the initial laser pulse. Of note, one to two passes of the laser are sufficient for each treatment session. Full-face laser treatment also may be performed if the patient exhibits fine rhytidosis elsewhere that is amenable to nonablative therapy. Generally, three to four treatment sessions administered at 1-month intervals are advocated to achieve maximal benefit for the patient. As emphasized, proper patient selection and education are prerequisites to patient satisfaction.
rhytids, it is advisable to have the physician hold the patients’ eyes firmly shut with the nondominant hand rather than use protective eyewear for the patient. The patient should be forewarned that the laser light is quite bright, especially when passed near the eye, even when the eye is completely closed. In addition, the patient may be gently startled by the cooling spray that immediately precedes laser delivery and should be informed of the initial laser pulse. Of note, one to two passes of the laser are sufficient for each treatment session. Full-face laser treatment also may be performed if the patient exhibits fine rhytidosis elsewhere that is amenable to nonablative therapy. Generally, three to four treatment sessions administered at 1-month intervals are advocated to achieve maximal benefit for the patient. As emphasized, proper patient selection and education are prerequisites to patient satisfaction.
For patients with epidermal actinic damage, even those who are still quite young (i.e., in their thirties), who have mild to moderate rhytidosis, chemical exfoliation with combined Jessner’s/35% TCA proves to be a reliable and effective treatment modality. This section discusses the technical aspects involved in achieving a uniform, safe, reproducible result.
Unquestionably, vigorous and thorough cleansing of the skin with 100% acetone is a critical first step to ensure that an even peel is attained. The acetone solution should be applied with a 4  4 gauze, which more effectively abrades the skin than a cotton ball or a cotton-tipped applicator can. The purpose of the acetone is twofold: to remove the outer layer of oil and function as a keratolytic of the stratum corneum, both of which may serve as physical barriers to attain a deep and uniform peel. The patient should be informed that the application of acetone might be somewhat unpleasant because of the noxious odors and vigorous application.
4 gauze, which more effectively abrades the skin than a cotton ball or a cotton-tipped applicator can. The purpose of the acetone is twofold: to remove the outer layer of oil and function as a keratolytic of the stratum corneum, both of which may serve as physical barriers to attain a deep and uniform peel. The patient should be informed that the application of acetone might be somewhat unpleasant because of the noxious odors and vigorous application.
 4 gauze, which more effectively abrades the skin than a cotton ball or a cotton-tipped applicator can. The purpose of the acetone is twofold: to remove the outer layer of oil and function as a keratolytic of the stratum corneum, both of which may serve as physical barriers to attain a deep and uniform peel. The patient should be informed that the application of acetone might be somewhat unpleasant because of the noxious odors and vigorous application.
4 gauze, which more effectively abrades the skin than a cotton ball or a cotton-tipped applicator can. The purpose of the acetone is twofold: to remove the outer layer of oil and function as a keratolytic of the stratum corneum, both of which may serve as physical barriers to attain a deep and uniform peel. The patient should be informed that the application of acetone might be somewhat unpleasant because of the noxious odors and vigorous application.The Jessner’s solution, which is comprised principally of alpha hydroxy acids (see preceding text box), acts to complete the keratolytic process. Jessner’s solution may be applied with relative impunity as the liberal application usually only penetrates into the outer epidermal layer. Often, a light frost may be evident but only indicates a reversible salt deposition rather than the irreversible blanching that ensues owing to protein coagulation when the actual TCA peel is applied. Unlike the TCA peel, no visual change of the skin color is targeted, because the superficial nature of the Jessner’s solution usually does not impart any color change. The patient does not require any sedation for this part of the procedure, because the Jessner’s solution usually only engenders a mild tingling sensation and only rarely frank discomfort.
Like application of TCA, the subunit principle is followed with application of Jessner’s solution. First, attention is paid to the lower eyelid/periocular region in the same fashion as described for the TCA peel. The patient is placed in an upright position, inclined approximately 60 degrees from the horizontal. This semiinclined orientation minimizes inadvertent entry of solution into the eyes during application over the lower-eyelid region while maintaining patient comfort. The assistant gently holds cotton-tipped applicators at both the lateral and medial canthi in order to prevent tears from unevenly diluting the peeled area and, more important, to minimize peel solution from entering the eye via capillary conduction. A bottle of balanced-saline solution (BSS) should always be on the table side should the patient report any ocular irritation or burning. (If the patient does complain of ocular discomfort, the surgeon should recline the patient to a supine position and gently flush the eyes with BSS with the stream targeted at the medial canthus. This method minimizes reflex closure of the eye that would impair proper ocular irrigation.) The Jessner’s solution is applied with a cotton-tipped applicator
in the lower eyelid region and with a cotton ball for the remainder of the face. It is important that the cotton ball be squeezed semidry before applying the solution to avoid unintentional trickle of solution onto the neck. Furthermore, the used cotton-tipped swabs and cotton balls should be promptly discarded into the waste bin so that confusion does not arise as to which cotton ball was used for which peel solution.
in the lower eyelid region and with a cotton ball for the remainder of the face. It is important that the cotton ball be squeezed semidry before applying the solution to avoid unintentional trickle of solution onto the neck. Furthermore, the used cotton-tipped swabs and cotton balls should be promptly discarded into the waste bin so that confusion does not arise as to which cotton ball was used for which peel solution.
After each lower-eyelid/periocular region has been treated, the surgeon should advance in a systematic fashion by subunit from forehead/temple region, right-cheek region, left-cheek region, the upper-lip/lower-lip/chin region, and then nasal region. The order is not important, but it is recommended that the surgeon proceed in the same order every time to ensure that no area is repeeled or missed. The nasal and upper-lid areas are relatively recalcitrant to significant rejuvenation with a peeling agent but are treated nonetheless to achieve a complete and uniform peel. However, the upper-lid area is treated very superficially given the attenuated skin in this area and the attendant risk of scarring. Also, the cheek and chin subunits should be gently feathered for about a centimeter onto the neck to curtail an abrupt transition. If a lifting procedure is entertained concurrently or independently, the transposition of ptotic tissues upward may result in the unpeeled area of the neck also moving upward into the facial region.
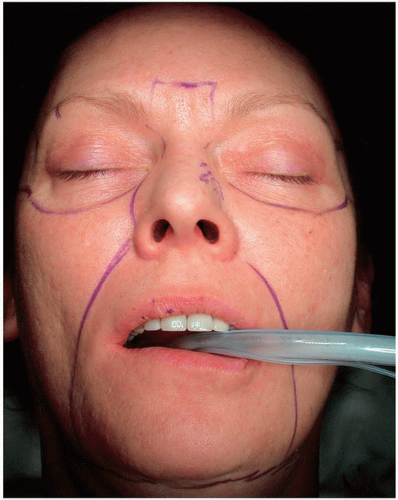
After the Jessner’s has been completed, the TCA may be applied immediately. First, the patient is marked out along subunits with a surgical marking pen, as the application of TCA must rigorously conform to the subunit principle to avoid overtreatment, undertreatment, or retreatment of areas (Fig. 9-4). If the patient is marked out before the Jessner’s solution, the marked areas are lost or markedly diminished by the Jessner’s peel. Before the patient is sedated, the lower-eyelid area is again treated first with the same technique and patient positioning described in the preceding for the Jessner’s application (Fig. 9-5A-C). Although the patient will experience noteworthy burning discomfort, the lower-eyelid application must be undertaken with the patient fully awake or only minimally sedated so that he or she may report any ocular burning due to entry of peeling solution into the eyes. In order to offset the burning sensation, a cooling fan is held by the second assistant at the level of the patient’s waist and aimed tangentially upward toward the face: A more direct gust may cause undesirable tearing and reflexive blinking.
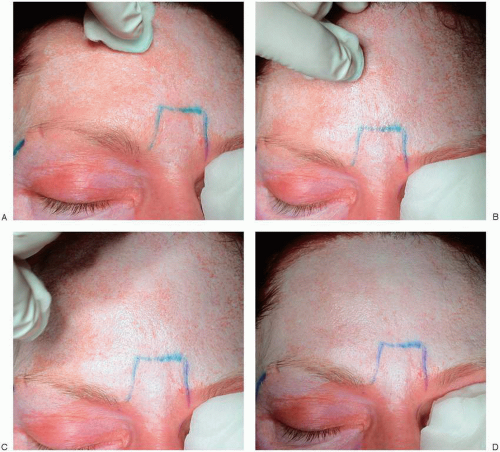
Unlike with Jessner’s application, the blanched appearance of the skin is a critical factor in determining when the desired end is achieved. The skin first assumes a mild erythema as the papillary dermis is entered, then a light frost, to finally a more complete, opaque white (Figs. 9-6A-D and 9-7A-C). After a few minutes, the skin may begin to regress back to a light erythema, fooling the physician into thinking that the area is undertreated. The return to erythema is a major reason that the subunit principle should be adhered to in order to avoid retreatment of areas known to be treated already. Generally, the end should be a completely uniform frost but not excessively opaque, which may risk scarring. Experience dictates proper depth of the peel, and review of the enclosed DVD further enhances education. As mentioned, the upper eyelids should be only lightly treated (light frost), because this particular area exhibits much thinner skin. The nose and forehead tend to withstand a deeper peel, but a deeper peel generally is not effective for the nasal area in any case. If the peeled area appears to have been overtreated, immediate application of gauze impregnated with water should be undertaken to dilute the peel solution and retard the action of the peel.
The authors advocate application of the TCA peel to discrete areas of deep rhytidosis first, if such areas are present, before evenly applying the solution to the entire subunit because the edema and frost that follow a coat of TCA effectively camouflage the linear areas of rhytidosis. Immediately after the subunit is treated, the area is covered with a gauze soaked in iced water in order to minimize patient discomfort
and terminate the chemical process. Iced pads may be reapplied as necessary to maintain patient comfort.
and terminate the chemical process. Iced pads may be reapplied as necessary to maintain patient comfort.
The neck and décolletage area may be treated with a lighter TCA peel (e.g., 15% to 25%). However, the reader is cautioned that aggressive and repeated application of a lighter-strength TCA eventually equals that of a higher concentration. The desired color change should be a light and semitranslucent white and not assume a completely opaque appearance.
After the peeling is complete, Aquaphor ointment (Beiersdorf, Wilton, CT) is generously applied over all peeled areas of the face with a tongue depressor. As the epidermis remains intact for several days, no occlusive dressing is required.
As discussed in the preoperative section of this chapter, CO2 laser resurfacing should be reserved for deeper rhytidosis, particularly the perioral rhagades, and for patients who are willing to contend with the longer recovery period (Fig. 9-8). Deeper rhytids of the glabella and perioral areas are only minimally addressed with a Jessner’s/TCA peel, and patients should recognize that limitation. An alternative to the laser is the phenol peel, but the authors have more limited experience with this peeling technique, which is not discussed herein. The reader is advised to be facile with various resurfacing techniques that have different advantages but not to feel obligated to master the Byzantine number of techniques available today.
 FIGURE 9-7. TCA Peel, Step 4. A: The next subunit is treated in a similar fashion. B,C: The ideal end point is shown as a uniform but not excessively opaque white. |
As of the last few years, the authors have been reluctant to subject patients to a full-face laser except in the rarer instances when deeper, panfacial rhytidosis mandates use of this modality. The facial areas that tend to be best suited for laser resurfacing are the glabellar, lower eyelid, and perioral regions. If the laser is applied only to discrete areas of the face, then a chemical peel should be considered in the adjacent areas to blend in the areas of resurfacing. Obviously, all areas should be peeled first before laser is applied to adjacent areas to avoid uncontrolled depth of the peel in areas that have been laser resurfaced. Like the TCA peel, the laser is generally applied by subunit so that adjacent TCA-peeled areas may blend effectively with the laser-treated areas. The laser is set at the recommended start-safe parameters that correspond with a power density for tissue ablation (10 J/cm2). The laser is held perpendicularly to the skin but aimed tangentially at the perimeter of the resurfaced area to camouflage the transition with the peeled areas. The second pass of the CO2 laser is undertaken to effect greater collagen remodeling and dermal ablation and is applied almost exclusively in a tangential fashion to minimize excessive thermal injury and depth of resurfacing. Beyond these enumerated technical considerations, laser resurfacing is technically much less demanding than chemical exfoliation and does not require further elaboration in this section. Unlike the TCA peel, the resurfaced areas are fully denuded of epidermis and require both Aquaphor ointment and an occlusive dressing to facilitate reepithelialization and principally to lessen discomfort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree