84 TFCC Outside-In Repair
Abstract
Triangular fibrocartilage complex (TFCC) is an intra-articular wrist structure with a significant role in stabilization, rotation, translation, and load transmission of the wrist. TFCC tears are traumatic but it can be degenerative. The initial treatment for these tears is always conservative and involves wrist immobilization for 6 to 12 weeks. Those patients that fail conservative treatment can be treated with arthroscopic repair or debridement, depending on whether the tear is central or peripheral.
84.1 Introduction
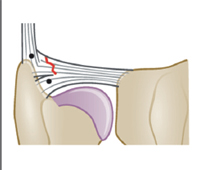
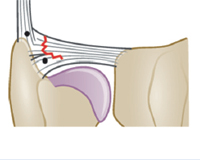
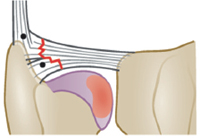
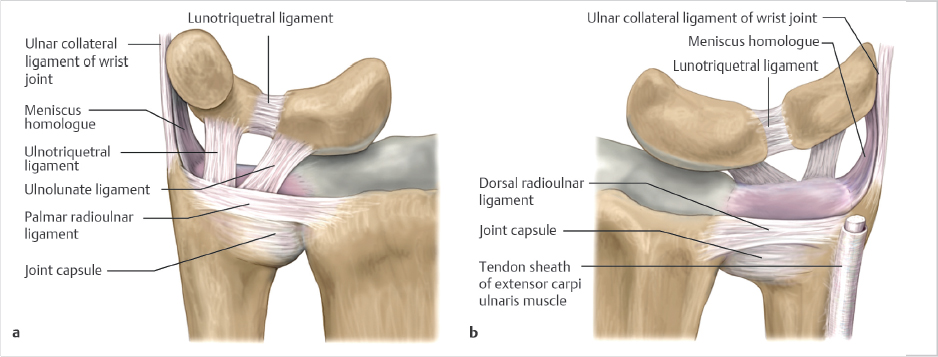
The triangular fibrocartilage complex (TFCC) is an intra-articular wrist structure that has a significant role in stabilization, rotation, translation, and load transmission of the wrist. 1 The TFCC was traditionally described by Palmer and Werner in 1981 to consist of five structures; an articular disk, volar and dorsal radioulnar ligaments, a meniscus homologue, the ulnar collateral ligament (UCL), and the subsheath of the extensor carpi ulnaris (ECU) 2 (► Fig. 84.1). The articular disk is bordered by the superficial and deep radioulnar ligaments, which insert on the ulnar styloid horizontally and vertically on the fovea ulnaris and base of the ulnar styloid, respectively 1 , 2 (► Fig. 84.2). The TFCC also inserts onto the lunate and triquetrum as the ulnolunate and ulnotriquetral ligaments. 2 Ahn et al also described a constant perforation of the meniscus homologue, termed the “prestyloid recess,” which is a normal anatomical structure. 2
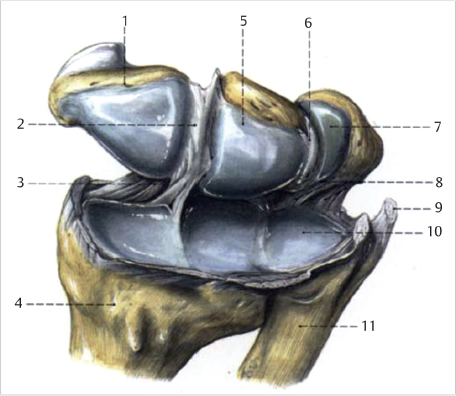
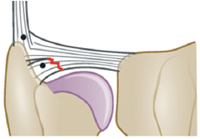
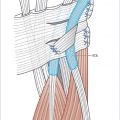
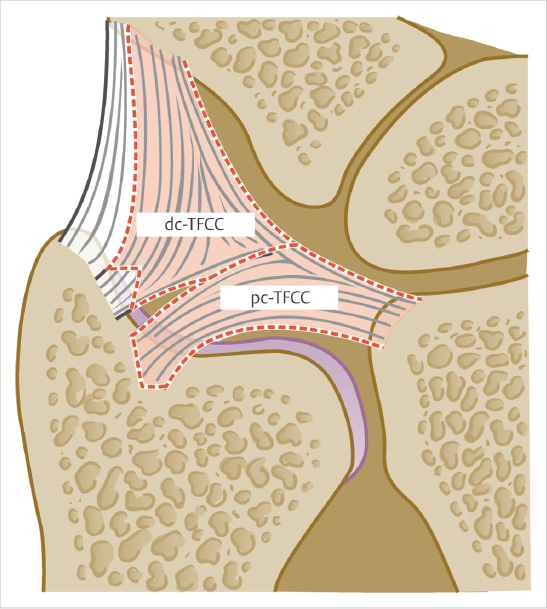
In addition, Atzei et al described three distinct components of the ulnar aspect of the TFCC, consisting of the proximal triangular ligament, distal hammock structure, and UCL. They proposed a treatment-oriented classification system based on these components, which has been endorsed by the European Wrist Arthroscopy Society (EWAS). The proximal triangular ligament represents the proximal component of the ulnar TFCC (pc-TFCC) and is synonymous with the ligamentum subcruentum or deep radioulnar ligaments. The distal component of the ulnar TFCC (dc-TFCC) is composed of the UCL and distal hammock structure (► Fig. 84.3). 3 The integrity of these structures dictate treatment options, as will be described below.
84.2 Key Principles
The TFCC receives its blood supply from the dorsal and palmar radiocarpal branches of the ulnar artery and also from the anterior interosseous artery. 1 It should be noted that the microvasculature of the TFCC is similar to the meniscus of the knee. It has been established that 10 to 40% of peripheral TFCC has a rich vascular supply, and the central region is relatively avascular. 1 , 4
84.3 Description
The mechanism of injury of TFCC tears can be classified as traumatic or degenerative. The majority of TFCC tears are traumatic, and commonly involve a fall onto an outstretched hand with the wrist in an extended, supinated position or a violent traction, twisting injury. 1 , 3 , 4 , 5 TFCC injuries also commonly occur in association with distal radius fractures, with studies reporting an incidence of 60% in intra-articular distal radius fractures. 6 , 7 In contrast, degenerative TFCC tears are the result of ulnar impaction syndrome with or without a component of ulnar positive variance.
TFCC tears commonly cause decreased grip strength and impaired wrist function, especially during powerful rotatory wrist movements. 1 , 8 Patients often have pain with palpation in the ulnar snuffbox, which is ulnopalmar to the ECU tendon at the wrist. 1 If distal radioulnar joint (DRUJ) instability is present in association with TFCC tears, patients often report spontaneous “giving way” of the wrist during resisted rotatory forearm movements. 3
Physical examination of TFCC injuries should include DRUJ ballottement test both in the clinic and under anesthesia to evaluate DRUJ stability. Ahn et al described a provocative ulnar grind test by dorsiflexing, axial loading, and ulnar deviating or rotating the wrist. Pain with this maneuver suggests a TFCC tear. 2 A positive ulnar foveal sign, which is point tenderness just palmar to the ECU tendon is also indicative of a TFCC tear. 3 Radiographs and MRI may be able to identify bony abnormalities and TFCC tears but are not able to accurately predict the size or location of the tear. 2 , 3 Wrist arthroscopy remains the gold standard for diagnosis of TFCC tears. 3
84.4 Special Considerations
Palmer et al described the classification of TFCC tears in 1989, and divided them into traumatic type 1 and atraumatic or degenerative type II tears. 2 Type 1a tears are located at the avascular central region and are the most common. If management with immobilization fails, arthroscopic debridement can provide symptomatic relief. Type 1b involves tears at the base of the ulnar styloid, type 1c involve the ulnotriquetral or ulnolunate ligaments, and type 1d tears are tears of the radial attachment. Type 1b-1d tears are initially managed conservatively, with good results with arthroscopic or open repair of type 1b and 1c tears which fail nonoperative management. Type 1d tears involve the avascular region; however, some authors report successful repair as well. 2 When conservative management or arthroscopic debridement is unsuccessful, degenerative tears of the TFCC are generally treated with variations of ulnar shortening or salvage procedures, depending on ulnar variance. 2
In 2009, Atzei et al subclassified type 1b tears into five classes, and proposed management options for each subtype. 3 This classification was endorsed by EWAS, and is based on distal or proximal ulnar TFCC lesions as well as reparable or irreparable lesions. 3 Atzei et al also incorporated the previously described trampoline test 9 and the hook test into their classification, which are described in detail below.
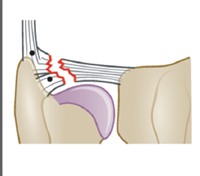
The trampoline test assesses the peripheral TFCC by using a probe to apply a compressive force across it (► Fig. 84.4). A positive test is seen when the TFCC loses its normal rebound tautness and is soft and compliant, indicating a peripheral TFCC tear. 2 , 3 However, the trampoline test is not always sensitive nor specific as some patients may have a more lax TFCC causing a slower rebound of the trampoline test which would lead to false positives. We recommend using the trampoline test as an adjunct to surgical decision-making. If the patient has failed nonoperative treatment and has a TFCC tear on MRI, an equivocal or positive trampoline test would be an indication for surgical repair or reconstruction.
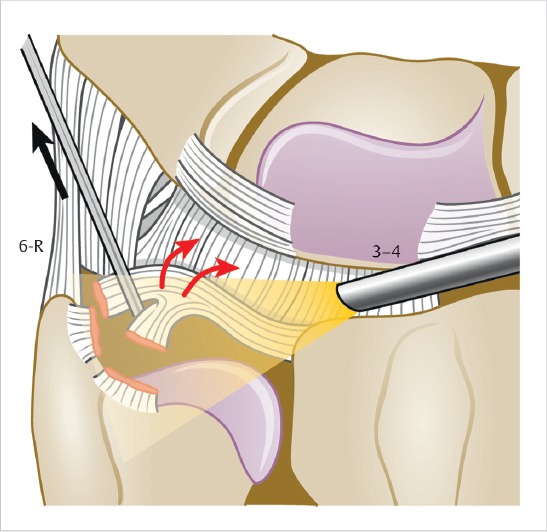
The hook test assesses the pc-TFCC and is performed by applying radial traction to the ulnarmost border of the TFCC. If the TFCC displaces upwards and radially, this indicates a tear of foveal insertion of the TFCC or pc-TFCC tear. 1 , 3
The Atzei classification of type 1b TFCC tears is described in ► Table 84.1. Briefly, Class 1 lesions have a reparable isolated dc-TFCC tear, a normal hook test and respond well to capsular suture repair. Class 3 lesions are reparable isolated pc-TFCC tears with a positive hook test and should be treated with foveal reinsertion. Class 2 and Class 4 tears are complete tears, but are either reparable and treated with foveal fixation or irreparable and need tendon graft reconstruction, respectively. Class 5 is any ulnar styloid base tear associated with DRUJ arthritis and requires salvage procedures. 1 , 3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree