6 Medium-Depth Chemical Peels
Key Concepts
Both the potential benefits and the potential deleterious side effects of resurfacing are directly related to the depth of skin injury created by the resurfacing modality.
It is frequently better to be more conservative rather than more aggressive in the utilization of resurfacing techniques.
It is usually best to use antiviral prophylaxis in all patients for full-face and perioral resurfacing.
Introduction
Facial enhancement through the use of chemical peels has existed since at least 1550 bc, when Egyptians used caustic preparations for skin-peeling procedures.1 Originating from these archaic formulations have evolved more modern agents developed to denature the protein framework of the skin and produce controlled wounding of the papillary/upper reticular dermis for cosmetic and noncosmetic indications.2 In 1882, Paul G. Unna described the actions of salicylic acid, resorcinol, trichloracetic acid (TCA) and phenol on the skin.1 “Skinning” or peeling of the face continued to be practiced using several agents and, by the 1960s, the modern era of peeling advanced with the development of modified phenol solutions by Baker and Gordon.3 This integral aspect of cosmetic surgery has subsequently grown to include the use of a number of modified phenol preparations, various TCA concentrations, and α-hydroxy acids.1
Background: Basic Science of Procedure
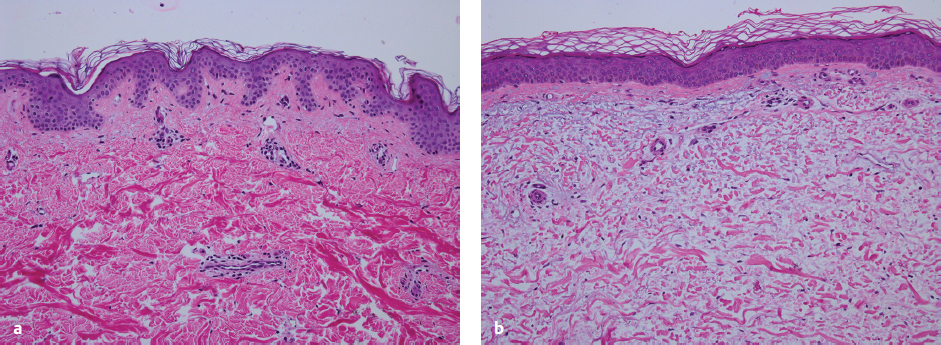
Photoaging principally refers to the effects of long-term ultraviolet (UV) exposure and sun damage superimposed on intrinsically aged skin.4 The negative effects of sun exposure on the skin can be exhibited by dyspigmentation, laxity, sallow color, wrinkles, telangiectasia, leathery appearance, and cutaneous malignancies.4,5 Histopathologically, there are abnormalities in collagen and elastin and ground substance breakdown and resynthesis.5 The cell population increases and becomes disorganized, with an abundance of collapsed and elongated fibroblasts, whereas elastin quantity decreases ( Figs. 6.1a,b ).6 Chemical peeling addresses this disorganization through limited wounding and subsequent healing, with collagen and elastin synthesis and cellular reorganization that ultimately result in more youthful and appealing skin. If the wounding proceeds to the epidermal basement membrane, where melanocytes lie, the wounded skin heals with a lighter, more even pigment. As wounding continues through the papillary dermis to the upper reticular dermis, deposition of new collagen, elastin, and glycosaminoglycans can result in a reduction of fine rhytids.7 Results become more pronounced the deeper the peel progresses.
Chemical peels can be used to treat a variety of cosmetic and noncosmetic skin issues. They can alter the effects of skin aging, stimulating neocollagenesis and correcting pigment.1 The desquamating properties of chemical peels can assist in acne treatment.8 The removal of melanin is effective in managing melasma and lentigines.9 Other indications for chemexfoliation include actinic keratoses, rhinophyma, xanthelasma, and syringoma ( Table 6.1 ).10
Rhytids (fine, medium, deep) |
Scars (traumatic, acne, varicella) |
Xanthelasma |
Pigmentary irregularities (i.e., melasma) |
Actinic keratosis (i.e., rhinophyma) |
Syringoma |
Classification of Peels
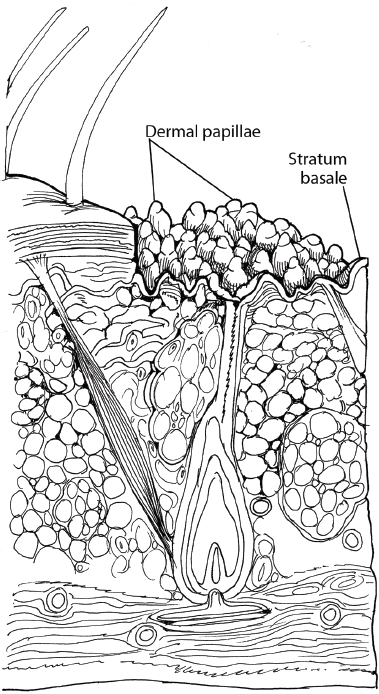
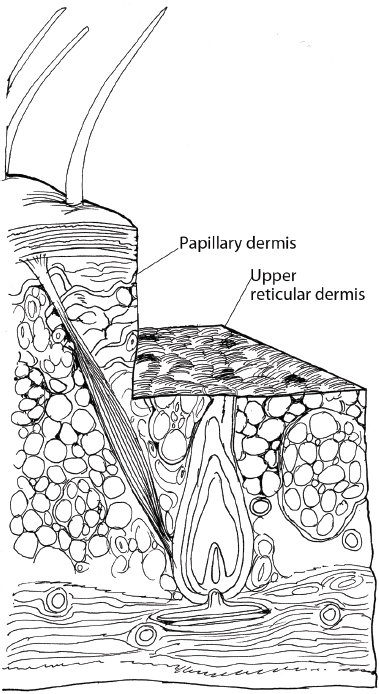
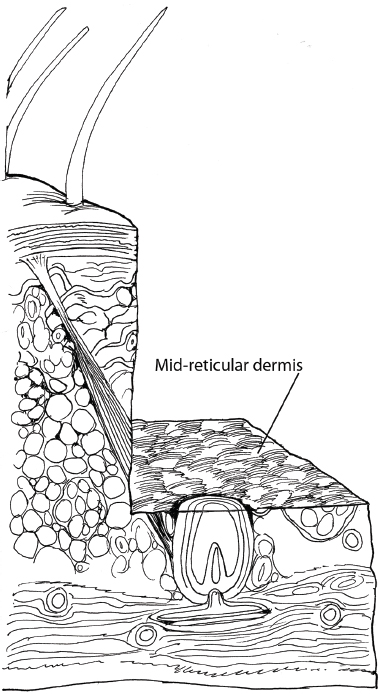
The expected depth of wounding is one way to categorize chemical peels. Superficial peels principally affect the epidermis ( Fig. 6.2 ), acting as exfoliants and removing the stratum corneum and superficial aspects of the epidermis. There is little cellular necrosis or stimulation of epidermal growth. Medium-depth peels typically extend to the papillary dermis and the upper part of the reticular dermis ( Fig. 6.3 ). Induction of inflammation within the papillary dermis occurs down to a depth of 0.60 mm. Deep peels generally extend down to the midreticular dermis11,12 and create an inflammatory response that induces production of new collagen and ground substances ( Fig. 6.4 ). The increase in ground substance results in an increased dermal volume and younger-looking skin. Reduced melanocyte activity and new collagen and anchoring fibril deposition result in a reduction in wrinkling and skin roughness.5 These depths of penetration are approximate and will vary depending on patient factors, the surgeon′s application technique, and the pre- and posttreatment of the skin.
The Medium-Depth Peel: 35% Trichloracetic Acid and Jessner′s Solution
TCA is a frequently used agent for chemical resurfacing of the face,10 treating a wide array of facial conditions in varying concentrations. At sufficient concentrations, the application of TCA will result in the disruption of the epidermis and dermis, thus stimulating regeneration of the dermal and epidermal elements.7 This catalyst is frequently used in combination with other agents that enable a deeper penetration, particularly Jessner′s solution. Composed of salicylic acid, ethanol, lactic acid, and resorcinol, Jessner′s solution is a keratolytic that breaks intracellular bridges between keratinocytes ( Table 6.2 ).13,14 TCA can be used as a superficial-, medium-, or deep-peeling instrument depending on the concentration employed.14,15 This chapter specifically addresses the use of the 35% TCA and Jessner′s medium-depth peel.
Salicylic acid 14 g |
Resorcinol 14 g |
Lactic acid (85%) 14 mL |
95% Ethanol (sufficient to make 100 mL) |
Source: Data from Alam et al.14 |
Pertinent Anatomy
The layers of the facial skin include the epidermis and the dermis. The deepest component of the epidermis is the basal cell layer, or stratum basale, which consists of undifferentiated proliferating cells and melanocytes ( Fig. 6.5a,b ). As cell migration advances upward, the process of cell differentiation is noted. Above the basal layer lies the stratum spinosum, which is composed of keratinocytes. Photoaged skin is characterized by loss of the orderly maturation of these keratinocytes.4 As cells differentiate further, they form the stratum granulosum, where additional keratin is synthesized. Also known as the granular cell layer, this layer has lamellar granules that contain polysaccharides, glycoproteins, and lipids that hold the stratum corneum cells together. The major physical barrier, or stratum corneum, lies most superficially and consists of devitalized, keratin-filled cells.
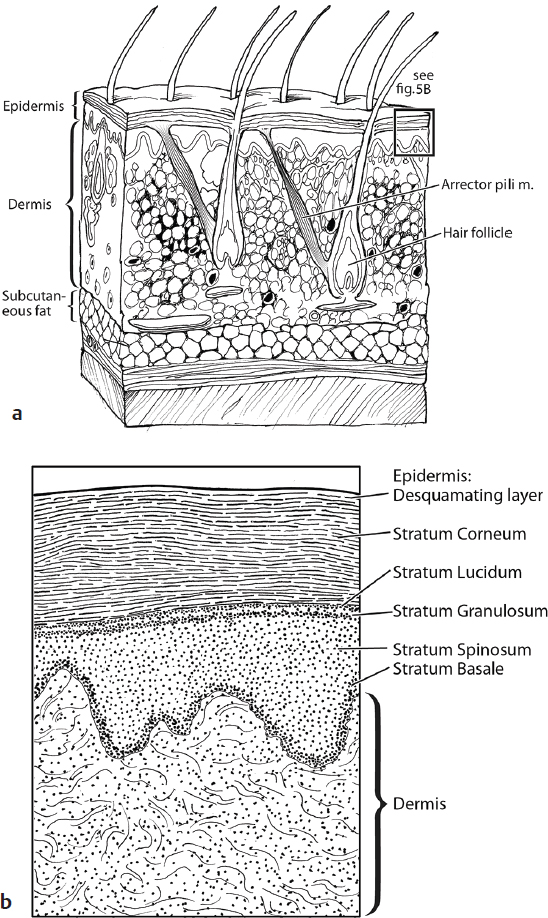
The reticular dermis is the deepest layer of the dermis and has thick and densely packed collagen fibers and the highest content of elastic fibers in the skin.16 Above the reticular dermis lies the papillary dermis, which consists of fine and loosely arranged collagen fibers. Collagen fibrils in the papillary dermis become disorganized in aging skin. The resultant fine wrinkles are a prominent feature of both aged skin and photoaged skin.4 Scarring from acne can result in thicker and more abundant collagen that is disorganized and stretched.17
Patient Selection
Proper patient selection is important to obtain cosmetically superior results and minimize complications. The photoaging classification system developed by Glogau18 ( Table 6.3 ) and the Fitzpatrick skin-type classification19,20 ( Table 6.4 ) are valuable references when assessing patients. These classification systems guide what depth peel is optimal and can predict the risk of postoperative complications. Specific complications are of concern when addressing patients with advanced Fitzpatrick skin types; patients with Fitzpatrick skin types III through VI may become hyperpigmented after peeling with superficial and medium-depth peels, but hypopigmented after undergoing deep peels.
Potential contraindications to chemical peeling of the face include pregnancy, breastfeeding, peeling within 6 months of isotretinoin treatment, skin infection, and active herpetic lesions ( Table 6.5 ). The level of peel must also be taken into consideration when judging risks. Relative contraindications to chemexfoliation include patient compliance issues, postoperative and preoperative care, sun exposure, smoking habits, and other compromising comorbidities. The experience of the physician in managing patient characteristics and expectations will aid in achieving optimal results.
Darker Fitzpatrick skin types (III–VI) |
History of keloid |
History of herpes infections |
History of diabetes mellitus or prior facial irradiation |
Unrealistic patient expectations |
Telangiectasias |
Anticipation of inadequate photo protection |
Significant hepatorenal disease |
Human immunodeficiency virus (HIV) |
Immunosuppression |
Poorly treated emotional instability or mental illness |
Ehlers-Danlos syndrome |
Scleroderma or collagen vascular disease |
Accutane treatment (within 6–12 months prior) |
Breastfeeding |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree