31 Hair Transplantation
Key Concepts
Male pattern androgenic alopecia is a hereditary problem due to the effects of dihydrotestosterone on the terminal hairs. The use of 5α-reductase inhibitors to stop testosterone conversion to dihydrotestosterone can reduce hair loss.
Hair transplantation is a viable option for hair restoration. Best results are seen in men who are over 25 years of age, with stabilized hair loss, coarse, wavy hair, and minimal contrast of skin and hair color. Donor-site density and scalp laxity also influence results.
Follicular unit transplantation is the gold standard in hair transplant surgery, producing natural, lasting results. Variations of the technique include donor strip harvesting and follicular unit extraction.
Introduction
Human concern with hair loss dates back to prehistoric times. Primitive remedies for baldness were quite imaginative, ranging from camel dung to stump water. Ancient Egyptians used castor oil to promote hair growth. Bhringaraj and amla oils were used in Asia. Since then, significant advancements in hair restoration have occurred.
In 1882, autologous hair transplantation was first shown to be feasible in animals by J. Dieffenbach, a German doctoral student. Fifty years later, Okuda described the first hair transplants in humans.1 He used punch grafts to treat alopecia in burn victims. However it was not until the 1950s, when Dr. Norman Orentreich described the first hair transplant for male-pattern baldness using punch grafting, that attention was given to hair replacement surgery.2 This treatment was based on the principle of donor dominance, which states that hairs maintain their innate ability to grow as they would have in their donor site.
Early transplants involved large numbers of hairs in each graft, sometimes referred to as plugs. Unfortunately, this could lead to an apparent “doll′s head” appearance. To obtain more natural-appearing results, smaller grafts were developed, called minigrafts, which included three or more hair follicles, and micrografts, which had one to two hair follicles. J.T. Headington is credited with describing the follicular unit as an anatomical entity, and his work gave credence to using smaller grafts. In 1988, Dr. Robert Limmer performed the first pure follicular unit transplantation.3 Since that time, the procedure has become the gold standard in hair transplant surgery, producing natural, lasting results.
Background: Basic Science of Procedure
All hair follicles are formed by gestational week 22. At this time, there are 5 million follicles on the body, of which 1 million are on the head, and 100,000 are on the scalp. As the size of the body increases with age, no new hair follicles are added, and the density of the existing follicles decreases.
The hair follicle is derived from both the ectoderm and the mesoderm. The hair matrix cells and the melanocytes originate from ectoderm, whereas the arrector pili, dermal papilla, follicular sheath, and blood vessels are mesodermal derivatives. The primary hair germ begins as an epithelial bud that protrudes into the dermis and is driven by the dermal papilla. Together, the papilla and the epithelial cells make up the hair bulb. The components of the hair follicle include the sebaceous gland and duct, the apocrine gland and duct, and the attachment point of the arrector pili muscle ( Fig. 31.1 ).4
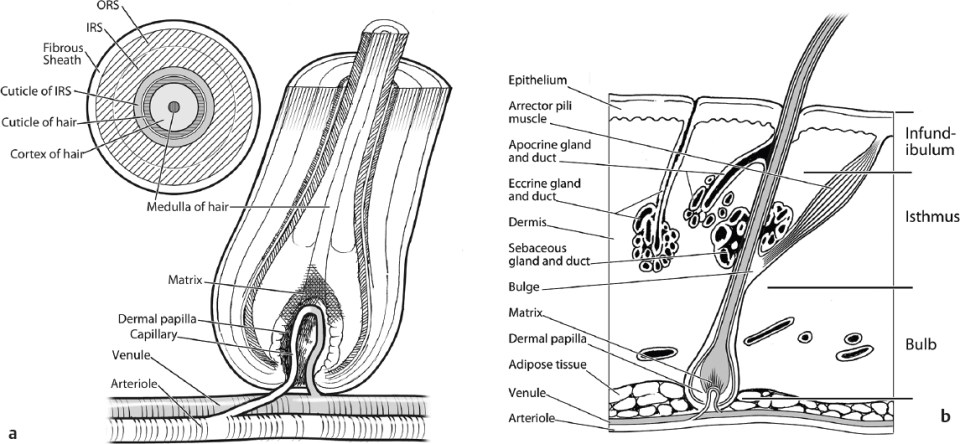
The hair follicle can be divided into three parts. The superior portion is the infundibulum, which runs from the entrance of the sebaceous duct to the follicular ostium. Apocrine cells may empty into the infundibulum. The middle portion extends from the insertion of the arrector pili muscle to the sebaceous duct and is called the isthmus. The inferior portion is the bulb, which extends from the base of the follicle to the insertion of the arrector pili muscle. It contains melanocytes and the hair matrix with cells responsible for hair growth. The hair bulb surrounds the papilla, which influences the activity within the hair matrix. Keratinization of cells within the hair matrix forms the hair shaft. Vellous hair lacks the innermost portion of the shaft, the medulla. A follicular unit is composed of one to four terminal hairs, with or without several villous follicles, associated sebaceous glands, the arrector pili muscles, and a common vascular and neural plexus, and is surrounded by a connective tissue sheath ( Fig. 31.2 ).
The follicular life cycle has three phases: anagen, catagen, and telogen ( Fig. 31.3 ). The anagen phase is the phase of active growth, which lasts ~ 3 to 4 years. Most hairs in the scalp are in the anagen phase. The catagen phase is a 2 to 3 week involutional stage in which the inferior portion of the follicle ascends to the level of the attachment of the arrector pili muscle. The telogen phase represents a resting period and lasts ~ 3 months. With aging, the number, rate of growth, and diameter of hair shafts decline. In predisposed individuals, the terminal hairs on the adult scalp can undergo involutional miniaturization (become vellus), and the percentage of telogen hairs increases.
Alopecia
There are multiple causes of hair loss, including trauma, burns, neoplasms, autoimmune disorders, chemotherapy, and dermatologic conditions. However, the most common form in both men and women is androgenic alopecia. Androgenic alopecia can present as male-pattern androgenic alopecia (MPAA), female-pattern androgenic alopecia (FPAA), or diffuse androgenic alopecia. Other causes of hair loss that can mimic pattern hair loss include acute and chronic telogen effluvium, diffuse or reverse ophiasis alopecia areata, and early cicatricial alopecia.
Telogen effluvium is characterized by massive hair loss as a result of early entry of hairs into the telogen phase,5 often secondary to emotional or physiological stresses. A variety of causes exist, including eating disorders, fever, childbirth, chronic illness, major surgery, anemia, severe emotional disorders, crash diets, hypothyroidism, and drugs.6 Hair loss lags the inciting event by ~ 3 months. Anagen effluvium is the pathological loss of anagen hairs. Classically, it is caused by radiation therapy to the head and systemic chemotherapy, especially with alkylating agents.7


Alopecia areata is an immunologically driven condition, often triggered by stress, that causes patchy hair loss, which can range from diffuse thinning to extensive areas of baldness with “islands” of retained hair. On exam, the hair will have an exclamation point appearance, becoming narrower along the length of the strand closer to the base. The diffuse form mimics telogen effluvium and FPAA.
Cicatricial alopecias involve inflammation directed at the upper part of the hair follicle, which leads to destruction of the stem cell and the associated sebaceous gland. The hair follicle is then replaced with scar tissue, and permanent hair loss results. Causes include lichen planopilaris, frontal fibrosing alopecia, central centrifugal alopecia, lupus, pseudopelade (Brocq), folliculitis decalvans, tufted folliculitis, and dissecting cellulitis. There are also many infectious and inflammatory causes of alopecia. Some of the more common infectious causes include dermatophytes and syphilis. These present with a patchy “moth eaten” alopecia.8 Hair loss in trichotillomania is typically patchy, as compulsive hair pullers tend to concentrate the pulling in selected areas. Often, short stubble hairs are present.
Pathophysiology
MPAA has been recognized as an androgen-dependent hereditary disorder since the 1940s.9 MPAA was noted to be absent in men castrated before puberty, but developed in 12 castrated men who were treated with testosterone. Men who lack androgen receptor expression also do not develop MPAA.10 However, it is dihydrotestosterone (DHT) that plays the dominant role in MPAA. DHT causes terminal hairs in the frontal and vertex/crown areas to become vellus, while at the same time causing vellus hairs to become terminal in the beard, mustache, chest, and upper pubic region. The enzyme responsible for converting free testosterone into DHT is 5α-reductase. Of the two isoforms of 5α-reductase, type II is expressed in androgen-dependent tissues, such as the prostate and hair follicle, and plays a role in MPAA. Men with deficiency of 5α-reductase do not develop MPAA.11
Men with androgenic alopecia typically have higher levels of 5α-reductase, lower levels of total testosterone, higher levels of unbound/free testosterone, and higher levels of total free androgens, including DHT.12 Current forms of medical treatment for MPAA aim to inhibit 5α-reductase activity. Men should be warned that anabolic steroids or supplemental androgens may increase hair loss. MPAA is caused by the genetic sensitivity of hair follicles to DHT, causing the hairs to miniaturize and have a shorter lifespan, therefore preventing the individual from producing hair normally. Approximately 50% of all men are affected by MPAA, and there is a strong hereditary predisposition. The inheritance pattern is most likely polygenic.13 Sons of men with MPAA have an increased frequency of MPAA, whereas sons of nonbalding men have a decreased risk of MPAA.14,15 There is a maternal effect on MPAA, but it is less defined.
Clinical hair loss in classic male-pattern baldness follows a well-defined pattern, consisting of hair recession in the frontotemporal region and loss of hair at the vertex. These areas of loss gradually enlarge and coalesce until the entire front, top, and vertex of the scalp are bald. The stages of hair loss were originally described by Hamilton16 and then modified by Norwood ( Fig. 31.4 ).17 The Norwood classification is as follows: Class I represents an adolescent or juvenile hairline resting on the upper brow crease. Class II hairline is 1.5 cm above the upper brow crease with some temporal recession. This is a mature hair line. Class III is the earliest stage of male hair loss and is characterized by a deepening temporal recession. Class III vertex represents early hair loss in the vertex. Class IV is continued hair loss in the frontal and vertex regions, but with a solid band of hair across the top separating the front and vertex. Class V is continued balding in the frontal and vertex regions with thinning of the bridge of hair separating the two areas. Class VI is the complete loss of the connecting bridge of hair, with a resulting single large bald area on the front and top of the scalp. The hair on the sides of the scalp remains relatively high. Class VII patients have extensive hair loss with only a rim of hair around the sides and rear. The Norwood Class A patterns are characterized by a front-to-back progression of hair loss, without the connecting bridge across the top of the scalp and a more limited hair loss on the vertex, even when advanced.
Usually, women do not suffer classic male-pattern baldness, but 30 to 40% of women are affected by hair loss. Women more commonly have diffuse central thinning18 or frontal accentuation,19 otherwise known as the “Christmas tree” pattern. Although the entire scalp is at risk of alopecia, recession at the temples is less likely than in men, and women tend to maintain the position of their hairlines. Female-pattern alopecia was classified by Ludwig in 1977 into three stages: mild, moderate, and extensive ( Fig. 31.5 ).18 Stage I is mild, with thinning in the crown but preservation of the frontal hairline. Stage II patients have significant widening of the midline part and noticeably decreased volume. Type III patients have diffuse thinning with a see-through look on the top of the scalp.
The role of androgens in FPAA is less straightforward. As already described, FPAA differs in distribution from MPAA. This is due to the fact that aromatase breaks down testosterone to estrogen and prevents the effects of DHT. The affected women typically do not have signs of hyperandrogenism and do not respond to treatment with 5α-reductase inhibitors.20 There is a smaller subset of women who present with a more typical male pattern of hair loss. These women may be suffering from hyperandrogenism and need to be evaluated for other signs or symptoms of hyperandrogenism, including hirsutism, moderate to severe or treatment-refractory acne, irregular menses, infertility, and galactorrhea. Women with male-pattern hair loss in the presence of signs of hyperandrogenism may respond to treatment with finasteride or cyproterone acetate.21,22 In addition, a family history should be obtained from the patient, although it may not be as clear as with males.


Medical Treatment
Before therapy is offered, a correct diagnosis must be made. Infections and autoimmune conditions must be identified and treated. Laboratory evaluation in men with androgenic alopecia is minimal. One may consider thyroid testing if the hair loss is diffuse and not following the typical MPAA pattern. Men on a strict vegetarian diet may be deficient in iron, and an iron evaluation may be warranted.
Women should have their thyroid-stimulating hormone (TSH) and serum ferritin levels tested. Deficiencies in either can cause telogen effluvium.23,24 Iron deficiency can interfere with medical treatment of FPAA.25 Women with clinical signs of hyperandrogenemia should undergo serological studies. These tests should include free and total testosterone and dehydroepiandrosterone sulfate. If galactorrhea is present, prolactin levels should be checked.
A scalp biopsy is indicated in men with female-pattern hair loss, diffuse hair loss, or scalp changes consistent with cicatricial alopecia. Women benefit from a scalp biopsy to exclude chronic telogen effluvium, diffuse alopecia areata, or cicatricial alopecia.
The topical and oral treatments for androgenic alopecia are numerous. Of these, topical minoxidil (Rogaine, McNeil-PPC, Lititz, PA) and oral androgen modifiers have been found to be effective. Minoxidil, a piperidinopyridine derivative initially used as a vasodilator to treat hypertension, was noted to increase hair growth in 70% of the patients taking the medication for hypertension. The action of minoxidil is not fully understood, but it might increase blood flow to the scalp or stimulate hair follicle growth through growth factor modification. Topical minoxidil applied every night in a 2 or 5% solution has been shown to be effective over 4 to 6 months.26 Discontinuation of treatment leads to loss of gained hair over 3 to 4 months.27 Initially, patients may observe an increase in hair loss because hairs are induced into anagen and telogen hairs are shed. Minoxidil is safe for use by both men and women, although the 5% solution may cause unwanted facial hypertrichosis in females. Therefore, it is recommended for women to use the 2% solution. Minoxidil used within days of hair transplantation can delay the typical shedding seen after hair transplantation and may shorten the period needed for hair grafts to regrow. There are minimal side effects associated with minoxidil use, and they are typically dermatologic in nature. The 5% solution is more likely than the 2% solution to cause scalp irritation, dryness, scaling, itching, or redness.
Drugs that interfere with type II 5α-reductase, such as finasteride, have been approved by the U.S. Food and Drug Administration (FDA) to treat hair loss in men. These medications, such as Proscar (Merck, Whitehouse Station, NJ), were originally used to treat prostate hypertrophy and were incidentally noted to improve hair loss. They work by reducing production of DHT, thus limiting the action of DHT on scalp hair follicles, but having no intrinsic steroid activity. Recommended dosage of finasteride (Propecia, Merck) is 1 mg daily.28 Increases in hair counts are seen within the first year of use; following this, there is a plateau of hair growth, but there is also a continued decrease in hair loss. The decreased DHT levels also reduce prostate-specific antigen (PSA), and it is recommended that any PSA value should be doubled for men taking finasteride.29 In men, side effects are limited to decreased libido, erectile dysfunction, and decreased ejaculate volume. These were noted in 1.8% of men ages 18 to 41 versus 1.1% in those on placebo and were reversible with cessation of medication.30
Because DHT is necessary for embryonic sexual differentiation and virilization of the male embryo, finasteride is contraindicated in women of childbearing age. No risk is seen to the fetus or the mother from semen of men taking finasteride.31 A 1 year, double-blind, placebo-controlled, randomized, multicenter trial of finasteride in postmenopausal women did not show increase in hair growth or decrease in the progression of hair thinning.20 Better results are seen in women with a male pattern of hair loss and evidence of hyperandrogenism.32 All women of childbearing age using 5α-reductase inhibitors or antiandrogens need to use effective birth control. Oral contraceptives have the additional benefit of lowering serum androgens.
Spironolactone is an aldosterone antagonist employed in clinical practice as a potassium-sparing diuretic used to treat high blood pressure. Spironolactone is used off-label to treat alopecia and hirsutism in females. It decreases production and blocks the effect of androgens at the cellular level. Birth defects are possible with this medication, and a form of birth control is recommended when taking this medication. Small, uncontrolled studies with spironolactone show efficacy of spironolactone in women who have hyperandrogenism.33 The minimum effective dose to treat hair loss is 100 mg daily. Doses above 100 mg a day are associated with uterine bleeding and a possible risk of developing breast cancer.34
In Europe, cyproterone acetate is approved for women with alopecia, high ferritin levels, or clinical evidence of hyperandrogenism. It is an androgen receptor–binding molecule that competes with DHT. Combining 100 mg cyproterone acetate with 50 µg ethinyl estradiol on days 5 to 25 of the menstrual cycle helps decrease side effects. Combination products of oral contraceptives and a small amount of cyproterone acetate exist but are not available in the United States.
Grooming
No patient undergoing hair restoration surgery should ignore the benefits of hair styling. A consultation with a hair stylist can maximize the effect of the transplantations, and most patients benefit from the use of a hairstyling blow dryer. Those with thin, straight hair can benefit from a permanent body treatment. The use of topical scalp concealers such as COUVRé or Toppik hair-building fibers (Spencer Forrest, Los Angeles, CA) can give additional benefit by deflecting light away from thin areas.
Surgical Treatment
The basic principle in hair restoration surgery is to redistribute the existing hairs to give the scalp the appearance of increased hair density. This can be achieved through transplantation, flaps, or scalp reductions. Hair transplantation has become the gold standard of hair restoration surgery. Initial methods involved the use of punches to remove large areas of donor hair and to place them in the areas of alopecia. Currently, smaller transplants are used to provide a more natural result.
Patient Selection
Although almost every patient is a candidate for some form of hair replacement procedure, there are certain factors that make some patients better surgical candidates.35 These factors include age, pattern of alopecia, heredity, hair density in donor area/fringe, hair and skin color, hair texture, and scalp laxity. Very few absolute contraindications to surgery exist, especially if one does not count lidocaine allergy, active autoimmune, inflammatory or infectious disease, and inadequate health status to undergo this type of surgical procedure.
Age
No minimum age limit exists for hair replacement, but experience has demonstrated that patients younger than their early twenties may be less content with the results gained. Waiting for the patient to mature tends to dissipate unrealistic expectations of hair density and allows the patient to accept a more mature hairline. It also allows the surgeon to better evaluate the progressive nature of the patient′s alopecia and to determine the final pattern of hair loss. Younger patients with premature alopecia also tend to have progressive hair loss and less impressive gains from restoration surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








