6 Correction of the Deviated, Twisted Nose
Pearls
Precise preoperative clinical analysis of external and internal nasal structures is the cornerstone of a successful corrective rhinoplasty.
It is essential to have a sufficient preoperative discussion between the patient and the surgeon about the surgical options and what can be corrected.
Facial asymmetry should be thoroughly evaluated preoperatively, and the patient should be informed of the results of the evaluation.
The surgeon should consider cosmetic improvement of the deviated nose as well as its functional restoration.
Dorsal deformities frequently accompany a deviated septum, and the most important step in corrective rhinoplasty is to create a straight septum along the midline.
The stability of a reconstructed nose is determined by the strength of the straightened septum, which originates from the integrity of the keystone area, reinforcement of the Lstrut, and affixation to the anterior nasal spine.
All extrinsic and intrinsic deforming forces should be evaluated and relieved intraoperatively with meticulous manipulation of each osteocartilaginous framework.
Bony deviation is corrected with accurate osteotomies based on detailed evaluation of each bony pyramid.
The preferred techniques for correction of the lower twothirds of a deviated nose are use of a spreader graft and septal extension graft.
Deformed osteocartilaginous frameworks should be managed in a conservative manner to the extent possible.
Postoperative care and followup are as important as the surgery.
Introduction
In rhinoplasty, correction of a crooked or twisted nose remains one of the most challenging surgeries. Nasal asymmetry is related to facial attractiveness, patient satisfaction, and quality of life.1,2 Deformities include not only aesthetic problems but also functional consequences, and thus correction of these coexisting problems should be accomplished simultaneously. The nasal anatomy of a patient with a twisted nose may be related to a bony pyramid deformity, septal deviation, asymmetry of the upper and lower lateral cartilages, or various combinations of these. The problem can be congenital, or acquired secondary to trauma or previous surgery. Furthermore, patients often have baseline facial asymmetry, and this affects the outcomes of corrective rhinoplasty. Because an anatomic reconstruction carries the risk of weakening the supporting bony and cartilaginous skeleton, a thorough understanding of nasal anatomy and physiology, precise preoperative and intraoperative analysis, the surgical knowledge and skill to perform a tailored surgical procedure, and meticulous postoperative management are all essential for correction of a twisted nose. In addition, the surgeon should be skillful and competent to perform a revision surgery if needed.
Patient Evaluation
A thorough social and medical history should be obtained from the patient and entered into the medical record. In particular, the obtained information should include smoking status, occupation, degree of concern with facial appearance, nasal trauma, previous nasal surgery, and co-morbidities such as allergic rhinitis and chronic rhinosinusitis.
Physical Examination
Examination of the External Nose
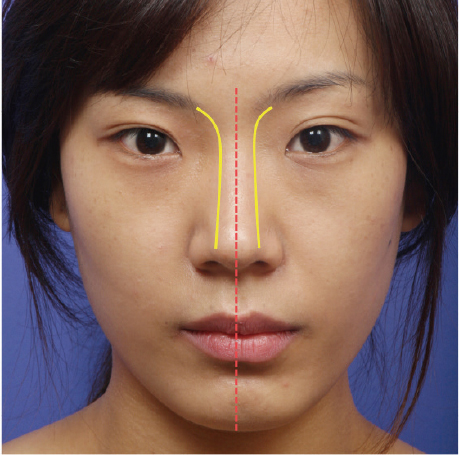
The initial step for successful correction of a deviated nose is a systematic physical examination that analyzes existing aesthetic problems and underlying anatomic deformities. When drawing a straight line from the midglabellar area to the menton, the nasal bridge and tip should be bisected symmetrically in an ideal nose. Additionally, the nasal dorsum should be outlined by two symmetric brow tip aesthetic lines extending from the medial supraciliary ridges to the tip-defining points (Fig. 6.1). Using this method, the degree and type of nasal deviation can be evaluated.
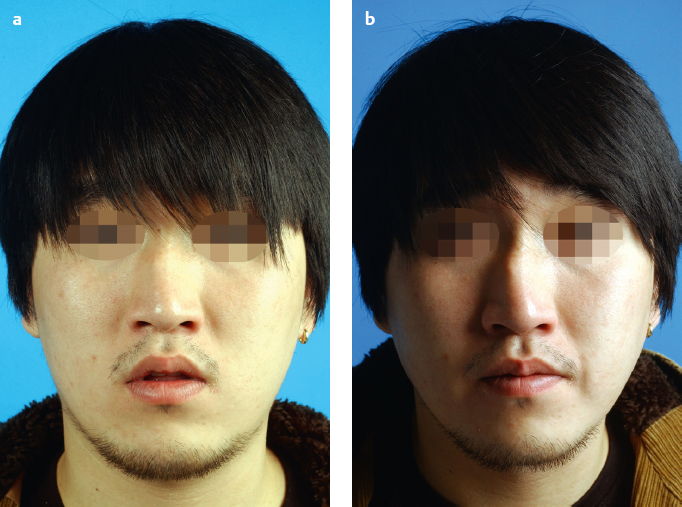
If the deviation is ambiguous, a bird’s-eye view or lateral illumination is helpful to identify any subtle deformity more clearly (Fig. 6.2 and Fig. 6.3). Then meticulous palpation of each anatomic element, including the bony pyramid, upper and lower lateral cartilages, cartilaginous dorsum, and columella, should be performed to evaluate size, shape, symmetry, and resilience. Facial asymmetry is not rare in patients with a deviated nose, and most patients become extremely conscious of their facial appearance after surgery.3 Therefore, any minor asymmetries should be described preoperatively to prevent patients from attributing them to surgery. The common causes of facial asymmetry are listed below.

Common causes of facial asymmetry include:
Difference in facial width
Asymmetric eyebrows
Orbital level difference
Off-center anterior nasal spine
Lateral placement of the piriform aperture
Nonhorizontal alar base
Maxillary or mandibular hyper-/hypoplasia
Malar prominence or recession
Examination of the Internal Nose
A patient with a deviated nose should be assessed for the presence of nasal obstruction. Through endoscopic examination of the nasal cavity and nasopharynx, patency of the external and internal valves, septal deviation, an inferior turbinate condition, adenoid hypertrophy, and any abnormal findings must be evaluated preoperatively.4 These alterations should be somewhat predictable preoperatively by several tests, such as acoustic rhinometry and paranasal computed tomography. If there is anything that could cause nasal obstruction, it should be managed during corrective rhinoplasty.
Examination of the Nasal Skin and Soft Tissue Envelope
The clinical analysis of external nasal deformities should include an evaluation of the skin–soft tissue envelope (SSTE). If the patient has a thick SSTE, it will take longer for the edema to subside and will disrupt the postoperative aesthetic outcome.5 In contrast, a thin SSTE is likely to reveal small remnant deformities underneath the skin.
Medical Photography
Standardized photographs are essential in the preoperative facial evaluation to confirm the clinical analysis of the nose and the face. Frontal, lateral, oblique, basal, and bird’s-eye views are the basic photographs that should be obtained. Medical photographs enable the identification of important facial findings that may have been missed during initial inspection and allow for comparison of the postoperative outcome and preoperative status.6
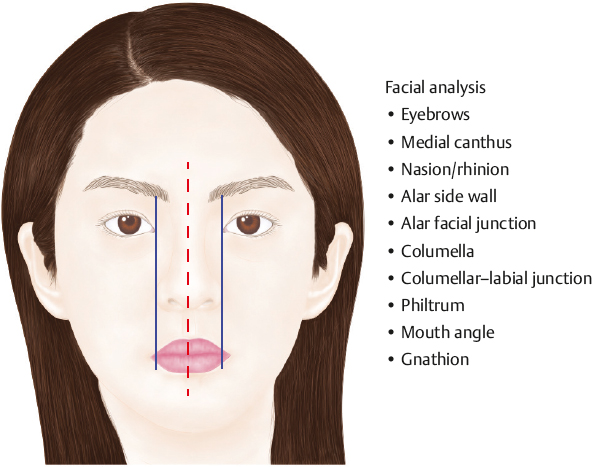
Fundamental facial analysis includes measurements and evaluation of proportions of the eyebrows, medial canthus, nasion, rhinion, alar sidewall, alar facial junction, columella, columellar-labial junction, philtrum, mouth angle, and gnathion (Fig. 6.4).
Surgical Planning
The next step is planning the surgical procedure based on clinical analysis. The surgical plan may consist of correction of the deformity and reinforcement of the framework. The appropriate approach and surgical techniques should be determined according to the deformities of each anatomic element. If use of a graft technique is anticipated, the surgeon should know the materials preferred by the patient before the surgery.7 Patients must be informed about the pros and cons of each graft material, including autologous (septal, conchal, or costal cartilage), allograft (fascia lata, alloderm), and artificial materials (Gore-Tex, silicone).8
Patient Interview and Selection
Once the surgeon has developed a plan, there should be a discussion with the patient about the details of the procedure and expected surgical outcome. Because there can be discrepancy in the definition of an optimal outcome between the perspectives of the surgeon and the patient, the surgeon should explain the results of the analysis and the expected outcome of surgery based on the photographs. Additionally, the surgeon should explain the potential differences between surgical goals and ultimate outcomes.
The final step of the preoperative evaluation is patient selection, and this is as important as the clinical assessment. Patients who have a realistic expectation for the surgery and an understanding of the surgical limitations are good surgical candidates. Surgeons should pay particular attention to detect poor surgical candidates who show excessive concern about minor deformities or have unrealistic expectations.
Surgical Techniques
Choice of Approach
The choice between endonasal and external approaches depends on the surgical plan and the surgeon’s preference.6 Although preoperative clinical analysis may enable selection of a particular approach, patients who undergo the endonasal approach must be informed of the possibility of conversion to an external approach for more complete correction. In general, the endonasal approach can be applied for cases with subtle deformities of the upper or middle vault, and for patients with keloid, who require avoidance of unpredictable contractures associated with an open approach.9 Meanwhile, an external approach is preferred for the management of deviation of the lower twothirds and severe asymmetries of the nasal bone, and some cases require maximal exposure, mobilization, and reshaping. Through bilateral marginal incisions connected to a transcolumellar inverted-V incision, complete exposure of the nasal tip and midvault in the supraperichondrial plane can be achieved. To approach a bony pyramidal deformity, an extended dissection in the subperiosteal plane is essential.
Correction of Deviation
Although there have been various classifications for the deviated nose,3,4,10,11 they all originated from the need for statistical analysis of outcomes rather than a clinical guideline for surgery. The deviated nose needs to be analyzed according to each anatomic domain (upper, middle, and lower third) and reciprocal relationships from a perspective of aligning to the midline.
Upper-Third Deviations
Deviation of the upper one-third of the nose is caused by asymmetry and hump of the bony pyramids. Through meticulous palpation and computed tomography, the size, shape, and symmetry of each bony pyramid should be evaluated. In cases of minor deformities, the bony dorsum can be corrected by a camouflage or rasping technique. A patient who has only a deviated bony dorsum is likely to have a history of nasal trauma or a humped bony pyramid.12 Generally, most bony pyramidal deviations entail a deflected middle third of the nasal dorsum.
Camouflage
This technique can be applied to a patient who has a localized depression or asymmetry of the bony pyramid. Crushed septal cartilage is the preferred graft material. The material is placed under a periosteal flap to reduce mobility and visibility. The skin over the bony dorsum is relatively thin; therefore, the surgeon must be certain to conceal the contour of the graft on the skin.13
Rasping
In some cases with bony pyramidal deformities, rasping can be a convenient surgical modality. If the bony pyramid has a symmetric arch but the dorsal profile is deviated or deformed, the rasp can be solely applied to correct the deformities. In many cases, rasping is used to trim the dorsal contour before bony pyramidal reconstruction of asymmetrical nasal bones through osteotomies. It should be noted that rasping must be performed carefully with consideration of how the bony pyramid will be positioned after the reconstruction.
Osteotomy
The osteotomy is one of the most essential but difficult techniques of corrective rhinoplasty. It involves cutting the nasal pyramid bones to correct a deviation. Without osteotomies, the deviated bony dorsum cannot be completely corrected. The osteotomy is a blind procedure, with no direct visualization of cutting lines; therefore, it is challenging to learn. Thus, surgeons should make an effort to gain reliable and reproducible surgical skills.
To avoid unnecessary complications, it is essential to have sound knowledge of the basic anatomy of the bony dorsum before performing an osteotomy. The bony dorsum is composed of the frontal bone, nasal bone, and frontal process of the maxilla; and these structures are joined together. The characteristics of the bone, especially changes in thickness, should be understood. Generally, the nasal bone is thicker in men than in women. It is thickest at the nasofrontal suture line (5 to 6 mm) and then becomes progressively thinner toward the lower margin (2 to 3 mm).14,15 The lateral wall of the bony dorsum consists of the nasal bone and the frontal process of the maxilla, and the thickness of the lateral process is less than 2.5 mm.
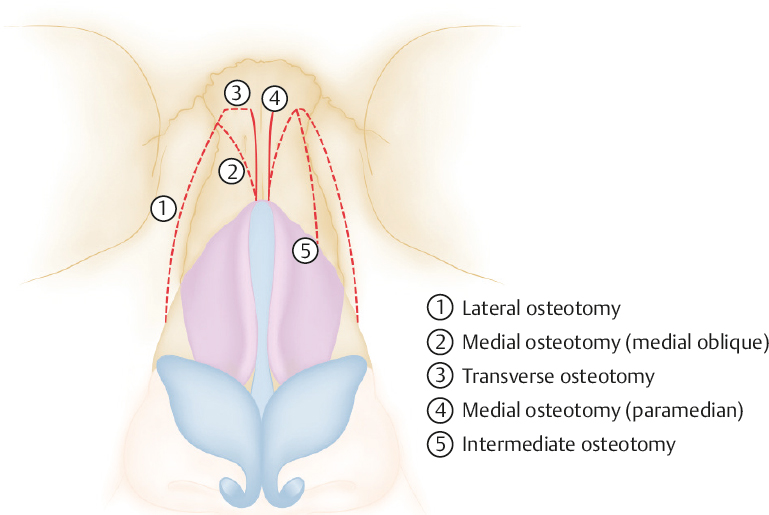
There are various types of osteotomy, including medial (medial oblique, paramedian), lateral, transverse, intermittent, and double lateral (Fig. 6.5). Though osteotomies are usually performed underneath the soft tissue envelope, a percutaneous external approach can be used for lateral and transverse osteotomies. Puncture site visibility after percutaneous osteotomy is negligible.16 To produce an accurate fracture line despite anatomic difficulties, the tip of the osteotome should always be sharp.
Lateral Osteotomy
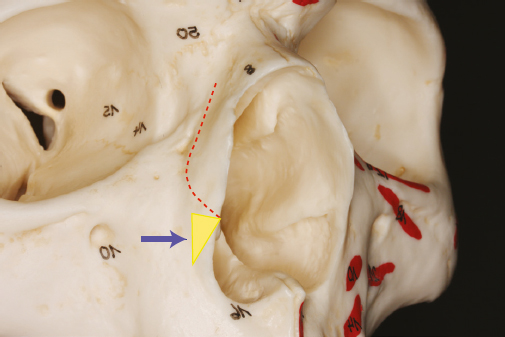
The purpose of the lateral osteotomy is to cut the nasal dorsum from the side wall. It enables the surgeon to obtain complete mobility of the nasal bones and then reposition them on the midline. As shown in Fig. 6.6 , the lateral osteotomy makes a continuous curved fracture line on the lateral aspect of the bony pyramid with an osteotome and hammer. Endonasal osteotomy is frequently performed using the vestibular approach. First, a small linear incision is made with a no. 15 blade on the lateral endonasal wall at the anterior margin of the inferior turbinate. Then iris scissors are inserted to dissect the soft tissues in the subperiosteal plane along the lateral rim of the piriform aperture. The dissection only needs to be wide enough to insert a guarded osteotome (curved or straight). When determining the start point of a lateral osteotomy, Webster’s triangle, which is a small triangular portion of the frontal process of the maxilla, should be preserved because the inferior turbinate inserts into this structure. Otherwise, the internal valve may be compromised (Fig. 6.6). The triangle can be preserved by starting the osteotomy at the slightly anterosuperior point of the piriform aperture edge.17 Through cautious palpation of the guard tip, the lateral osteotomy can be continued along the designated osteotomy line. The osteotomy should stop at the level of the intercanthal line and approximate the upper margin of medial osteotomy.
In some patients who have a severe asymmetric contour or excessive convexity of the lateral bony wall, a single lateral osteotomy is not enough to construct a symmetric nose. In these cases, an additional osteotomy on the deformed lateral bony wall is useful to produce a symmetric and natural concavity of the lateral nasal wall (double osteotomy). The fracture line should be parallel to the lateral osteotomy and approximate the nasomaxillary suture line.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








