41 Scaphoid Pinning/ORIF
Abstract
Scaphoid pinning or open reduction internal fixation (ORIF) is utilized in the treatment of displaced scaphoid fractures. It is increasingly being used in minimally or nondisplaced fractures. The scaphoid is the most commonly fractured carpal bone with unique anatomy and qualities which complicate treatment. Nonunion of the scaphoid can have severe functional consequences, and therefore acute fractures warrant prompt treatment. Cast treatment can be very effective for nondisplaced fractures but requires prolonged immobilization. Surgical fixation, when indicated, can obtain high rates of union. Fixation may proceed from either volar or dorsal, each with its merits and pitfalls. Observance of fracture management principles, including anatomic reduction, compression, and soft tissue handling are of the utmost importance. In this chapter, we highlight several key considerations in scaphoid fracture fixation, and certain tips to aid in success.
41.1 Description
There are several methods of operative fixation for scaphoid fractures. The bone can be approached dorsally or volarly via formal open reduction and internal fixation (ORIF) or miniopen percutaneous fixation. There have been multiple techniques and various screw designs described for internal fixation—most often, a cannulated, headless compression screw is used. The scaphoid’s unique anatomy and shape can present challenges to fixation.
41.2 Key Principles
The goals of scaphoid fixation are to preserve vascularity, achieve anatomic articular reduction, generate compression and maximal biomechanical stability across the fracture site through a centrally placed implant, and restore intercarpal alignment to preserve wrist kinematics.
41.3 Expectations
Nondisplaced or minimally-displaced scaphoid waist fractures can be treated by cast immobilization, usually with a thumb spica. Treatment usually requires 8 to 12 weeks of immobilization, and if initiated promptly, can result in union rates of 88 to 95%. 1 , 2 The disadvantages of cast immobilization are frequent office visits to assess cast fit, recurrent X-rays to assess fracture alignment, prolonged immobilization with associated potential skin breakdown, and joint stiffness. Displaced fractures as well as proximal pole fractures carry a higher rate of nonunion with rates as high as 50%, and are therefore generally indicated for open reduction internal fixation (ORIF). 2
Union rates of nearly 100% have been obtained using percutaneous fixation of nondisplaced and minimally displaced scaphoid fractures. 3 Operative fixation has also been shown to have faster time to union (7 vs. 12 weeks) and faster return to work (8 vs. 15 weeks) when compared to cast immobilization. 4 However, this study was conducted in a controlled military setting and generalization to a broader population is limited. A recent meta-analysis showed heterogenous results in favor of surgical treatment regarding time to union and range of motion; however, there was also a trend toward increased complications. 5
41.4 Indications
Indications for operative management include:
Displaced fractures-defined as having 1 mm of radiographic gapping or displacement, scapholunate angle>65 degrees, or a radiolunate angle>15 degrees. 2 , 6
Open fractures.
Complex fractures—associated with perilunate dislocations or distal radius fractures. 6 , 7
Proximal pole fractures.
Relative indications for fixation include a nondisplaced or minimally displaced waist fracture in an athlete, manual laborer, or patient who would otherwise not tolerate prolonged cast immobilization. While surgical treatment is a favorable option, there are limitations to the current literature and more rigorous studies are required. Ultimately, this should be a decision that is made with the patient after discussion of the risks and benefits. 5
41.5 Contraindications
Scaphoid fixation is contraindicated in patients with radiocarpal degenerative arthritis in which a salvage procedure may be better indicated.
41.6 Special Considerations
The scaphoid’s unique anatomy needs to be considered carefully. It is a curved bone, with a volar–ulnar concavity and an axial twist with the distal tubercle being pronated relative to the proximal end. This can make screw positioning difficult, and fluoroscopic imaging deceptive and difficult to interpret. The body is predominantly covered in articular cartilage, and vascular inflow is limited to the dorsal surface at the waist, scaphoid ridge, and volar distal pole. Seventy to eighty percent of blood flow enters via the dorsal carpal branch of the radial artery. The proximal pole relies solely on retrograde blood flow, making healing more tenuous increasing the rates of delayed union, nonunion, and avascular necrosis of the fracture fragment. 1
Fixation can be performed from either a dorsal or a volar approach. The volar approach works well for middle and distal third fractures as the fixation is retrograde. During open procedures, there is excellent exposure of the waist, allowing for reestablishment of length, alignment, and angulation. It offers the distinct advantage of preservation of the dorsal blood supply. Drawbacks of the volar approach are that it requires disruption of the important extrinsic radiocarpal ligaments, central implant placement is technically difficult and needs some degree of disruption of the scaphotrapezial joint, and proximal pole fractures cannot be captured reliably.
Advantages of the dorsal approach are access to the proximal pole, preservation of the scaphotrapezial joint and extrinsic volar ligaments, and ease of central screw placement compared to the volar approach. Drawbacks include increased risk of insult to the dorsal vascular supply, and some degree of difficulty in correction of sagittal deformity.
41.7 Operative Treatment
41.7.1 Special Instructions, Positioning, and Anesthesia
All procedures are performed supine with a hand table and tourniquet in place along with fluoroscopy. The authors like to have a wrist roll made to aid in either extension or flexion.
The procedure may be performed under general anesthesia or under sedation with local or brachial plexus block.
41.7.2 Tips, Pearls, and Lessons Learned
Preservation of blood supply is paramount, especially as proximal pole fractures have a higher rate of avascular necrosis. This concept is particularly important when an open dorsal approach is utilized, as it places the main vascular inflow at risk. 1 , 6
During a volar approach, it is essential that the extrinsic ligaments be repaired. Often, a zigzagor s-shaped capsulotomy will facilitate a tension-free closure (► Fig. 41.1).
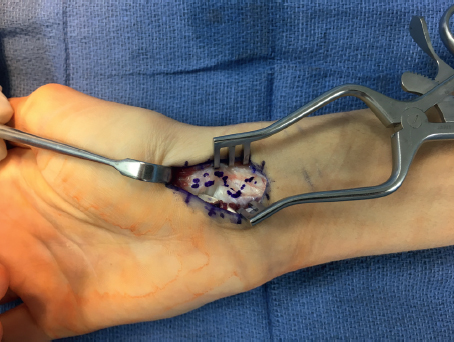
During a volar approach, the ideal guide wire starting point is within the scaphotrapezoid joint. As such, some of the trapezium may have to be removed with a Rongeur. In addition, a transtrapezial approach to screw placement can help improve positioning. Obvious concerns of these methods incudes disruption of the articular cartilage and eventual degenerative changes.
Measure screw length with the K-wire in subchondral bone on the opposing side and the measuring guide sitting flush with scaphoid. This can be difficult from a volar approach, with the trapezium blocking access to the starting point. Select a screw at least 2.5 mm shorter (we prefer 4mm shorter) than the measurement to avoid fracture distraction and screw prominence.
During a dorsal approach, after measurement and prior to reaming, the K-wire may be driven into the trapezium to maintain reduction and prevent incidental pullout of the guide wire during reaming (► Fig. 41.2).
Medullary compression screws should be placed within the central 1/3rd of the scaphoid in both AP and lateral radio-graphs. This has been shown to have 43% stiffer construct and improved alignment and range of motion compared to eccentric placement. 8 Central placement has also been shown to have decreased time to union when compared with eccentric screw placement (► Fig. 41.3). 9
Cannulated screw technique has been found to have a higher rate of central placement when compared to an external reference guide. 9
Fluoroscopic guidance may be used to ream over the guide wire to reach subchondral bone without penetrating the joint.
After appropriate alignment has been obtained and a central K-wire has been placed for a cannulated screw, it may be useful to place a second K-wire, eccentrically across the fracture site as an antirotation pin prior to screw insertion. Alternatively, if the first pass of a K-wire ends eccentrically, this should be left in place as an additional visual cue to place a second K-wire centrally and the first will take on the function of an antirotation pin (► Fig. 41.4).



The screw should be placed by hand, and the guide wire removed prior to the final turns to optimize compression. 7
Screw heads should be countersunk to prevent chondrolysis, especially within the radioscaphoid joint. 6
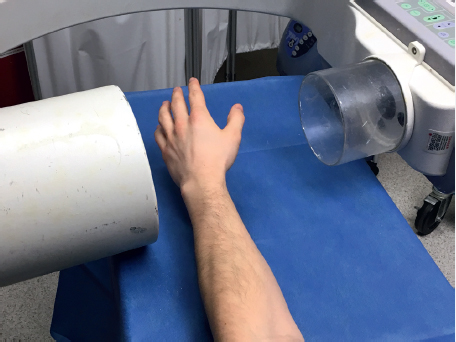
The most sensitive radiographic view to evaluate penetration into the radioscaphoid joint has been found to be 60 degrees of pronation from neutral, with the transducer beam parallel to the floor (► Fig. 41.5). 10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree