39 Secondary Rhinoplasty
Introduction
Revision rhinoplasty has become a commonplace procedure. As the number of rhinoplastic surgeons has expanded, and the depth of experience has diminished, it is not unusual to see revision rate as high as 15–20% after primary procedures. 1 Factored into this rate is the phenomenon that patients expect near perfect results—a trend created by the media and optimistic advertisements by the surgeons themselves. This atmosphere of unrealistic expectations certainly adds to the demand for revision rhinoplasty.
Rhinoplasty as a procedure presents certain problems unique to facial surgery. The combination of skin and soft tissue, cartilage, bone, and mucosa brings together a mix of tissue with varying healing characteristics. This puts the onus on the surgeon to predict how these tissues will heal in concert with each other. Although mostly predictable, even a well-performed rhinoplasty operation may result in an unfavorable result. With experience the rhinoplastic surgeon must learn to anticipate healing patterns, and thus minimize the need for revision surgery.
In the history of rhinoplasty, especially in the early 20th century, most techniques were reductive in nature. The early works of Roe 2 and Joseph 3 specifically addressed altering the nose to reduce prominence in the dorsum and tip. Combined with an emphasis on intranasal incisions at all costs, these techniques often led to inaccurate and uneven resection of nasal structures. The results were often not apparent for years, due to the prolonged tissue edema and patients unfamiliar with expected results. In fact, during the first twothirds of the 20th century functional sequelae were often not reported.
The latter part of the century has brought a better understanding of the relation between nasal form and function. Rhinoplasty techniques are now less aggressive, with an emphasis on preservation of key structures. Aesthetic norms are now more widely recognized, which together with structural preservation helps prevent the notorious ski-sloped, pinched tip results that were so common up into the 1970s. The reintroduction of the open rhinoplasty technique has allowed for more accurate modifications in some cases. The open approach, however, has created some new problems as the surgeon tends to be more inclined to make more alterations. In general, the more alterations in a nose, the more likely complications are to occur.
Analysis
The first order of business in evaluating a revision rhinoplasty patient is to determine what surgery has been done in the past, and by what techniques. It is important to determine the number and timing of past procedures, and also how the patient feels about the current status. Questions should be asked about the original nose, function before and after the surgical interventions, and what the expectations of further surgery are. Operative notes may be helpful and should be requested. If the previous surgery was more than 10 years before the consultation, it may be difficult to obtain these records.
The patient interview is also vital to determine if the patient has realistic expectations. There is a subset of patients who will never be satisfied with any result and thus keep seeking revision surgery for even small, insignificant physical traits. Patients with body dysmorphic disorder are not good candidates for surgery and must be identified as early as possible to avoid further complications. 4 The experienced surgeon learns how to spot these patients and steer them to more appropriate psychological consultation. 5
Physical diagnosis is the other key to successful revision nasal surgery. An accurate assessment of the aesthetic and functional problems will help the surgeon determine the best course of action. Therefore, a detailed internal and external nasal examination is essential during the initial, and subsequent, consultations. Specific areas to examine include the nasal septum, turbinates, and internal valves. Externally the upper, middle, and lower vaults with their associated anatomical components must be individually assessed. The status of the skin–soft tissue envelope must be evaluated with regard to thickness and rigidity. Old scars should be documented. In revision rhinoplasty patients the stability of the nasal valves is often in question. The surgeon should determine if pathology exists in the internal valve, external valve, or both. This area is frequently overlooked by rhinoplasty surgeons. Not all patients with nasal obstruction have problems limited to the septum and turbinates.
Therefore a thorough aesthetic, functional, and psychological assessment must be obtained before deciding if a patient is a proper candidate for revision rhinoplasty surgery.
Timing of Revision Surgery
Most revision rhinoplasty patients present more than 1 year after the initial surgery. This occurs due to several factors. Most surgeons will accurately point out to patients that the soft tissue takes at least 1 year to mature, reassuring their patients that in time certain deformities will diminish. This is often true, but not universal. Many patients are satisfied for a number of years before deformities become more obvious, often associated with functional problems. This patient group demonstrates graphically that the final results of rhinoplasty may actually encompass 10–15 years or longer. Serial photographs taken over a 20- to 30-year period clearly show continuous soft tissue changes and movement of cartilaginous structures. This phenomenon of “shrink wrapping” of the skin–soft tissue envelope has been well described. 6
Though it is usually wise to wait 1 year for the initial soft tissue edema to resolve, an exception to the rule is for a gross deformity, which has no chance to improve. A significant saddle nose or severe loss of tip support are examples of problems that will likely get worse while waiting a full year. The added factors of scar contraction and loss of tissue planes will only make the correction more difficult at a later date. Therefore, for some deformities, the correction should be undertaken as soon as the problem is recognized.
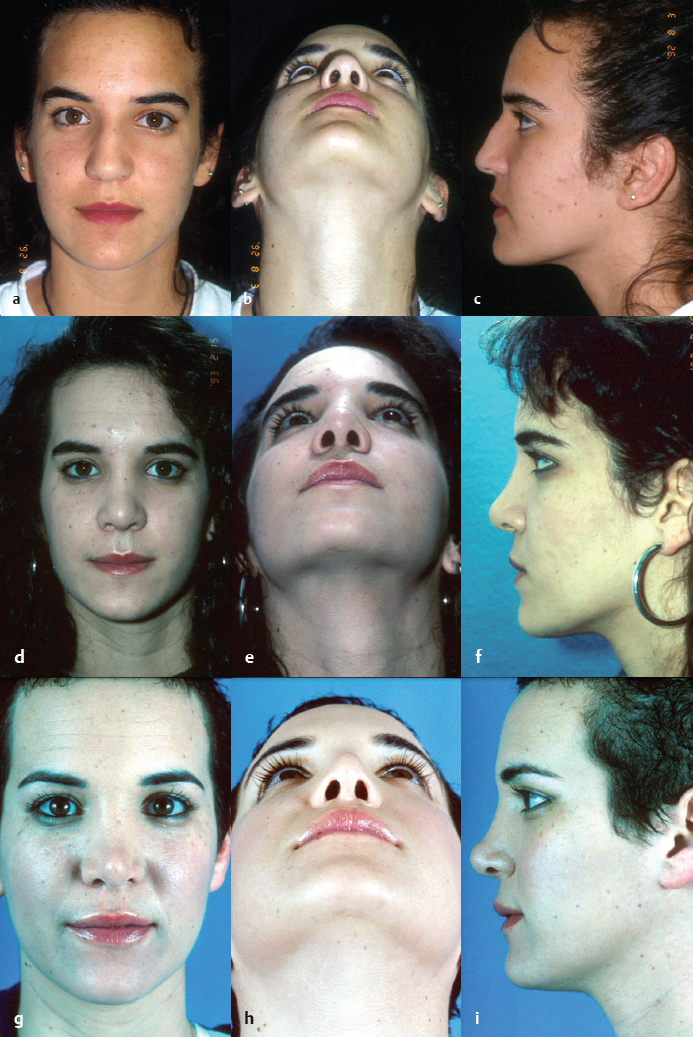
Fig. 39.1 demonstrates the power of tissue contraction over a 10-year period. Notice the changes in both tip and dorsal lines as healing occurs.
Approach
In recent years the open approach has become more popular for primary rhinoplasty. However, in revision rhinoplasty the choice of approach should be dictated by the deformity or problems being addressed and not the prior approach that was used. The surgeon should choose the approach that provides the best exposure to repair the problem, balanced with the least invasion/alteration required to get that result.
For example, an uncomplicated dorsal contour deformity is best addressed through an intranasal, intercartilaginous incision. This will preserve the tip structures, which require no further alteration. Simple alar grafting may actually be easier to perform via a marginal incision than an open method. Conversely, a patient with significant middle vault collapse that needs structural grafts may require an open approach for proper placement and fixation of the grafts. Significant tip asymmetry also lends itself to open procedures.
The choice of approach should be dictated by the individual needs of the patient. All rhinoplastic surgeons should have an array of techniques available to treat the wide range of deformities encountered.
Grafting Materials
Revision rhinoplasty often requires replacement of structural anatomy. As a general principle of reconstruction the surgeon should replace anatomical structures with like materials. In the nose, this implies autologous cartilage grafts to repair the lower twothirds. Cartilage is often used to repair the upper one-third and other bony structures as well.
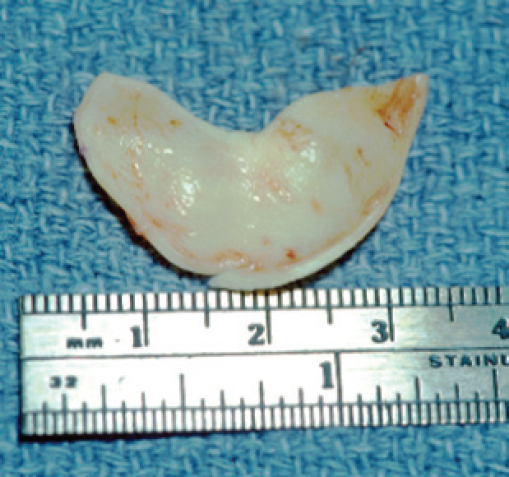
If septal cartilage is available, this can usually be obtained most easily, with minimal morbidity. Unfortunately, many revision rhinoplasty patients have already had resection of septal cartilage in previous procedures. Auricular cartilage is the next best choice and is present in most patients with good quantity. It is especially helpful in alar reconstruction due to its inherent curvature and thickness. Auricular cartilage can be obtained from the conchal bowl via either a lateral or medial incision and can also be used to obtain composite grafts.
Costal cartilage is a rich bank of cartilage for patients in need of more extensive reconstruction. This may be needed if septal and/or auricular grafts are not available. Harvesting of rib cartilage does require more time and is associated with more donor site discomfort than septal or ear cartilage. Care should be taken to avoid pleural puncture, and the incision should be meticulously closed to minimize the scar.
In some patients, irradiated homologous costal cartilage may be an alternative to autologous cartilage. In the specific patient with multiple comorbidities, weak auricular cartilage, or ossified costal cartilage, irradiated homologous costal cartilage may be the best choice. Additionally, in someone who is in need of significant dorsal augmentation this can mitigate the need for harvesting a large piece of rib. Proponents of irradiated homologous costal cartilage emphasize the large quantity of grafting material available and the lack of donor site morbidity as reasons for its use. 7 In addition to dorsal onlay, it can be used for a wide variety of grafts including tip grafts, columellar strut, or alar batten grafts. However, unpredictable resorption and warping of the graft have been noted in longterm followup studies. 8 Donor site morbidity, risk of reabsorption, infection, and warping are all factors that must be weighed and considered with the patient.
Cranial bone has been utilized for dorsal nasal reconstruction with some success. 9 The bone is harvested from the outer table of the parietal skull, and is available in large amounts. Donor site morbidity is minimal with careful technique. 10 Fixation of the bone grafts is essential, and using a sunken lag screw into the preexisting nasal bones is a reliable method. Cranial bone grafts in the nose do tend to create an unnatural stiffness, often noted by patients.
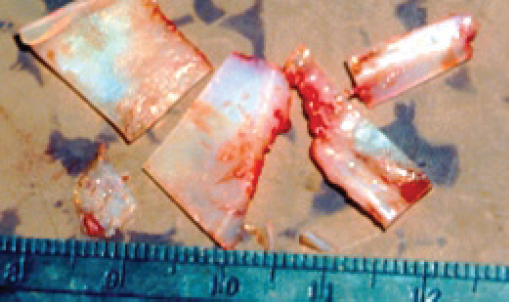
Synthetic materials have been utilized in primary and revision rhinoplastic surgery for many years. The rate of extrusion or infection of materials such as Gore-Tex (W. L. Gore & Associates, Inc.) or Medpor (Stryker) in primary cases has been about 3%. 11 This complication rate in revision rhinoplasty patients is much higher. With increased follow up, the rate of extrusion seems to increase. 12 Therefore, many surgeons will only utilize synthetic materials in revision rhinoplasty if no other options are available or if the patient refuses the use of autologous grafts ( Figs. 39.2–39.4 ).

Bony Dorsal Deformities
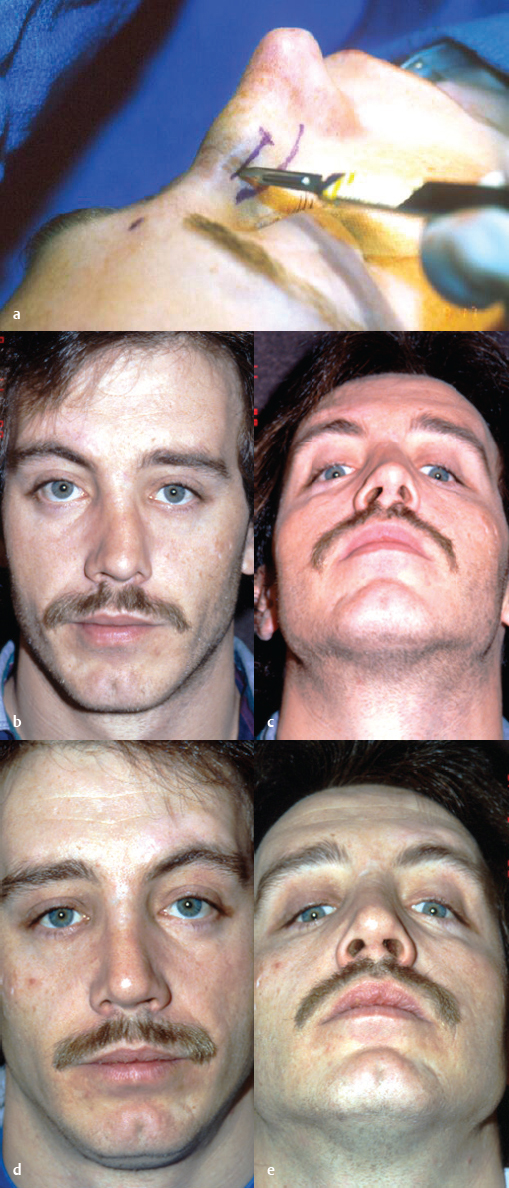
The most common deformity of the bony dorsum after rhinoplasty is a visual contour deformity. This may be midline or lateral. These contour defects are due to uneven resection or augmentation of the upper one-third of the nose. Due to thin skin coverage in this area the defect is usually apparent early and does not improve with time. Treatment will usually require an intranasal approach, undermining of the skin–soft tissue envelope, and correcting the contour by rasping the bone edges or augmenting depressions with small cartilage grafts ( Fig. 39.5 ).

Deviation of the nasal bones after rhinoplasty is also very common, especially if there was asymmetry beforehand. Correction may require a combination of revision osteotomies and/or onlay grafts to camouflage bony concavities. An intermediate osteotomy on bony convexities combined with lateral osteotomies may help even out the bony dorsum ( Fig. 39.6 ).
Stair step deformities of the upper lateral dorsum are the result of a lateral osteotomy being placed too high on the nasal process. This results in a visible and palpable deformity, often asymmetric. Treatment will require medial and lateral osteotomies to mobilize and properly place the lateral bony fragments.
Rocker deformities can result when the osteotomy produces a fracture that extends beyond the nasal bone and into the medial orbital wall. Pressing medially on the nasal bone inferiorly causes the superior bones to lateralize, thus named a rocker deformity. Treatment will require splinting the bones in the original position and allowing healing for 8–12 weeks. After the bones are fully healed the proper osteotomy can be accomplished.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








