33 Complications and Outcomes After Immediate Partial Breast Reconstruction
Partial breast reconstruction at the time of lumpectomy often adds additional procedures with their own inherent increased risk of complications. Moreover, postoperative irradiation for breast cancer is an integral part of breast-conserving therapy (BCT), additional complications or accentuation of surgical complications may also arise. When oncoplastic techniques are employed, it is important that complications do not interfere with the initiation of adjuvant therapy, whether chemotherapy or radiotherapy.
In this chapter, we discuss immediate and delayed complications. Cosmetic outcome is also considered, and we present guidelines to reduce complication rates and improve aesthetic results.
Immediate Complications
Displacement Techniques
Different methods of parenchymal redistribution have been described to fill small and moderate defects in the breast.
Looking at aesthetic surgery as a whole, breast reduction surgery in the United States is second only to rhinoplasty in the number of malpractice claims filed over the past 10 years. 1 Most of these malpractice cases are related to complications.
The incidence of complications is generally related to the surgeon’s learning curve and/or the patient’s body mass index (BMI), breast size, smoking history, and skin management. Oncoplastic surgeons should never forget the complexity of the procedure when two different procedures are done in one stage, which may accumulate the complications of both. Therefore complications may occur more frequently in oncoplastic breast reduction than in classic breast reduction procedures. The defect often has undermined areas that would not ordinarily have been undermined and skin flaps are often thinner than expected as a result of tumor resection. This all needs to be taken into consideration when planning the oncoplastic procedure and techniques changed to avoid adverse outcomes.
Patient Examples
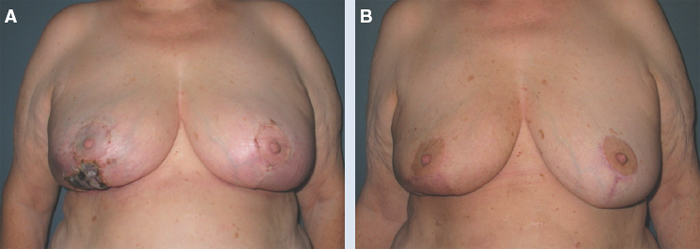
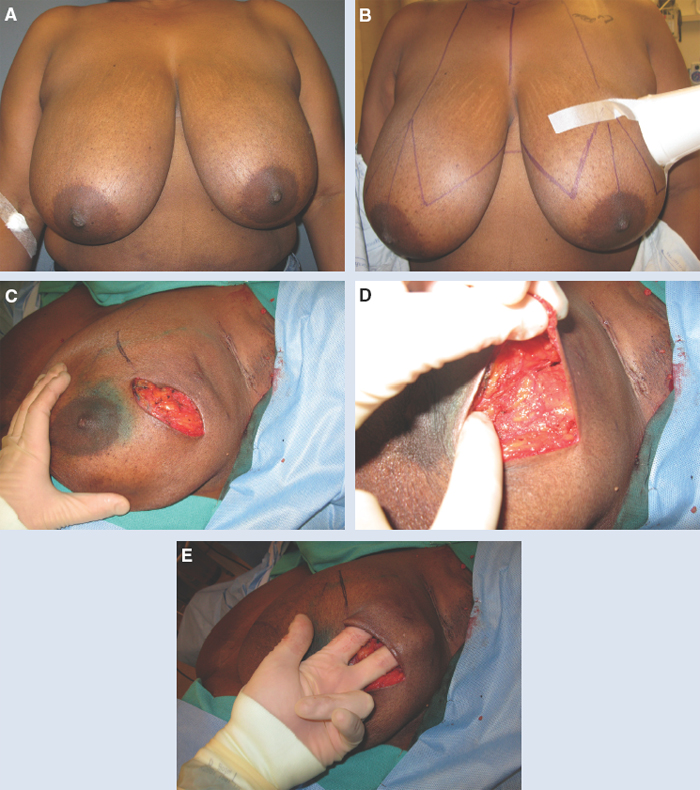
This 45-year-old woman had a superficial tumor resected from the right lower quadrant with an oncoplastic reduction to reconstruct the deformity. She unfortunately had full-thickness skin necrosis, necessitating debridement and split-thickness skin grafting before radiotherapy.
One year after completion of radiotherapy she had a significant deformity. This was reconstructed by excision of the contracted skin graft and placement of a latissimus dorsi flap.
Although her result was good after reconstruction with the latissimus dorsi flap, she required an unplanned reoperation as a result of a complication from skin flap necrosis.
This 52-year-old woman had a superficial left lateral invasive ductal carcinoma. She underwent tumor resection, and on examination of the defect, her skin flaps were found to be very thin. This was concerning for the development of skin necrosis (as described for Fig. 33-1).
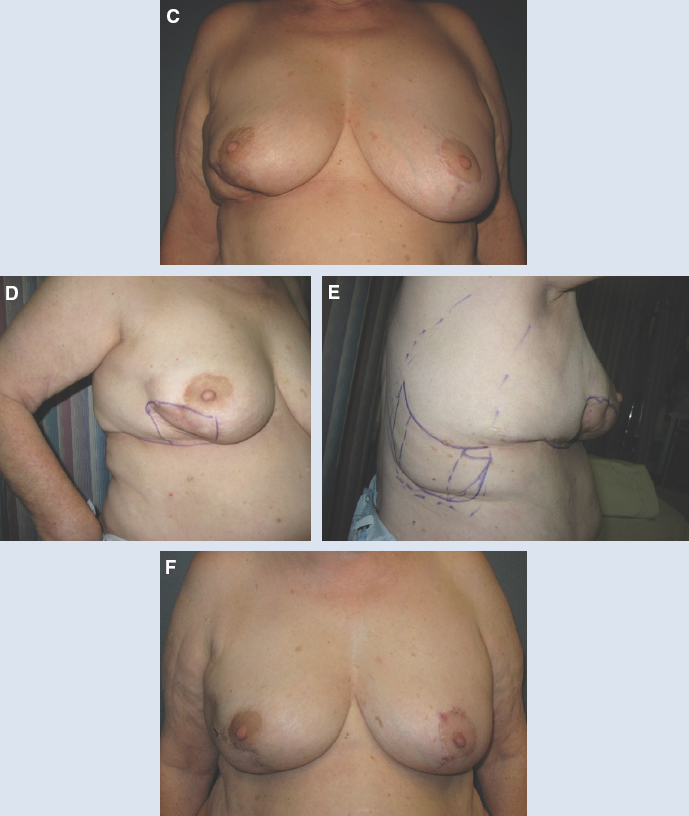
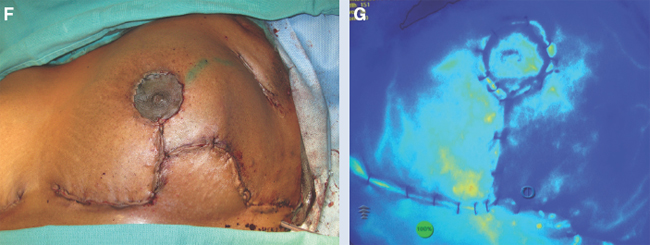
An immediate oncoplastic reduction was performed using a superomedial pedicle, and the skin was closed temporarily. Intraoperative angiography confirmed poor perfusion in the area of concern, subsequently predicting skin necrosis.
An inferiorly based flap was preserved because of a suspicion that skin ischemia might occur, and this was used to reconstruct the defect once the thin skin was removed.
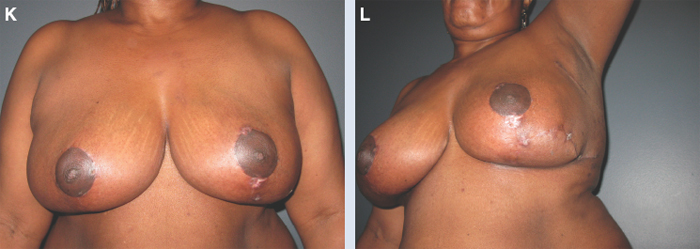
Her result is shown 1 month after oncoplastic reduction with a well-healed skin envelope that will tolerate radiotherapy better than thin skin flaps or a skin graft.
Ischemia of glandular or dermoglandular flaps may lead to fat necrosis when a large glandular flap with large skin undermining or separation from the muscles is done to close remote or large breast defects (see Fig. 33-1). Partial or total nipple-areola complex (NAC) necrosis can also occur. Most likely, unanticipated extension of the tumor resection into the subareolar region in an attempt to obtain a negative intraoperative tumor margin may result in a compromising of blood supply to the NAC (see Fig. 33-2). Wound dehiscence can occur either in the NAC or at the junction of an inverted-T scar. Incidence of other complications such as hematoma, seroma and infection is usually not different from the classical breast reduction. Nevertheless, overall complication rates after oncoplastic breast reduction was reported by Nogushi et al 8 to be as high as 24%. However, the authors found that some techniques (delayed corrections) performed in irradiated breasts have 50% complication rates. They also found that tumor location is a factor in the incidence of complications.

Tumors located within the upper outer quadrants tend to have the highest rate of complications followed by the inner quadrants of the breast.
One of the explanations is that resection performed in the upper outer quadrant is adjacent to the axillary lymphatic system, which can be traumatized intraoperatively and increase the potential for fluid-related complications. Another reason may be that the excessive length of a glandular flap that should be harvested and rotated upward to reach the most upper outer area in the defect which may end up with fat necrosis. The inner quadrants of the breast are also prone to complications because of the deficiency of surrounding breast tissue to fill the resultant defect.
Most of the repairs were done for tumors within the inferior quadrants, which reflects a particular experience of the surgeon with this technique. However, this may result in a less optimal outcome when the surgeon uses one technique for tumors with different locations. Munhoz et al 2 reported a larger series with 209 immediate breast-conserving reconstructions. However, only 141 of their patients underwent displacement procedures: 32 breast advancement flaps and 109 mastopexy or breast-reduction procedures. In the first group, fat necrosis occurred in 2 cases (6.25%). The authors reported a lower fat necrosis rate after mastopexy and breast-reduction techniques. They used lateral thoracic flaps or LD flaps for upper outer defects.
Adopting an algorithm for selecting the appropriate technique should reduce the complication rate and improve cosmetic outcomes. A recent comparison of timing of the oncoplastic reduction procedure demonstrated an overall complication rate of 21% when the reduction was done at the time of mastectomy, compared with 57% in delayed reconstruction. 3 Complications were higher in the delayed group as a result of the scarring and radiotherapy and more likely higher in the immediate delayed group because of the inflamed environment in which the reduction was being performed. The incidence of fat necrosis was 1% in the immediate reduction group and 14% in the delayed reduction group (p <0.001). Nipple necrosis was also significantly higher in the delayed reduction group (5% versus 0%, p = 0.01).
A recent meta-analysis compared 1773 oncoplastic reductions, 1392 oncoplastic flap reconstructions, and 5494 BCT-alone patients. 6 The average complication rate in the oncoplastic reduction group was 16%, and in the oncoplastic flap reconstruction group was 14%; however, there was no delay in the initiation of adjuvant therapy. Early complication rates were not routinely reported in the BCT-alone group; however, were on average 25.9% (n = 201: 775), compared to 15.5% (386: 2482) in the oncoplastic group. Satisfaction with the aesthetic outcome was significantly higher in the oncoplastic group 89.5% (1148: 1283) versus 82.9% (1590: 1916), (p <0.0001) in the BCT-alone group.
In a large oncoplastic series with 540 patients, Fitoussi et al 4 reported a complication rate of 16%. Complications are rarely recorded in BCT-only reports; however, in a series of 714 patients with BCT alone, Waljee et al 5 reported a complication rate of 24%. Such complications, especially in BCT-only patients, are often managed conservatively. The severity of the complications in the oncoplastic groups is different, with the need for surgical intervention being roughly 3%. It does not appear that complications in the oncoplastic groups, although potentially higher, have any negative impact on patient care from an oncologic standpoint. The reoperation rate is relatively low and does not appear to interfere with appropriate management. Safety is further confirmed by the lack of any adverse effects on cancer surveillance in both the oncoplastic reduction and flap reconstruction groups. Late complications requiring additional surgery are usually related to aesthetic outcome, radiation changes, or recurrence.
Box 33-1 Surgical Guidelines for Displacement Techniques
Careful preoperative assessment of the tumor resection and anticipation of the resultant defect are essential.
Surgical protocols and algorithm should be employed in selecting the appropriate reconstructive technique.
Any unnecessary glandular flap and or skin undermining must be avoided.
Skin-glandular flaps or perforator-based glandular flaps should be selected.
Excise ischemic or less vascularized parts of the flap, mainly the distal portions.
Meticulous hemostasis must be ensured.
A drain should be placed.
Dead space must be avoided.
A separate incision should be considered for axillary lymphatic dissection.
Tight skin closure must be prevented.
Replacement Techniques
Authors | Number | Overall Complications (%) |
Hernanz et al 9 | 28 | 39 |
Rainsbury et al 10 | 49 | 8 |
Nano et al 11 | 18 | 77 |
Kat et al 12 | 32 | 19 |
Gendy et al 13 | 49 | 8 |
Losken et al 14 | 39 | 31 |
Munhoz et al 15 | 48 | 33 |
A significant number of authors have reported their experience using volume replacement techniques for the immediate correction of the partial mastectomy defect. This approach restores the breast volume using autologous extramammary tissue as the frequently used latissimus dorsi flap. Noguchi et al 8 first described using the LD myocutaneous flap for partial breast reconstruction.
One major difference in flap techniques when compared with volume displacement techniques is the addition of donor-site complications. This increases the overall complication rate for flap techniques and ranges from 2% to 77%. 9 – 15 In most situations, the donor-site complication rate is higher than the flap complication rate, likely because of high seroma rates. Flap-related complications consist of total or partial flap loss, fat necrosis, hematoma, wound dehiscence, and infections, whereas donor-site-related complications include seroma formation, hematoma, wound dehiscence, and infection.
Munhoz et al 15 recently reported a 33% complication rate using the latissimus dorsi technique for partial mastectomy defects; 65% of these were related to the donor site. The most common complication was dorsal seroma, which occurred in 20% of their patients (that is, 50% of their complications). However, when they compared obese to nonobese patients, seroma formation was significantly higher in the first group.
Wound dehiscence should be less frequent when a smaller skin island is harvested.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree