20 Facelift: The extended SMAS technique
INDICATIONS
Facial aging, including slack facial skin
Relaxed nasolabial folds
Jowling
Obliquity of cervical contour
Facial fat descent with radial expansion of the fat away from the facial skeleton
INTRODUCTION
Rejuvenation of the aging face has taken many turns over the last few decades. Most recently, non-surgical rejuvenation with neuromodulators and facial fillers has exploded in popularity. These quick, short-term solutions are appropriate for some patients and some problems, but they do not address the global issues of facial aging. Facelifting procedures remain the best long-term answer to the problem of facial aging. The extended superficial musculoaponeurotic system (SMAS) technique for facelifting addresses and corrects many of the problems that occur with facial aging. 1 Issues and anatomic changes addressed during this type of facelift procedure include skin laxity (secondary to loss of elasticity), facial fat descent, facial deflation, and radial expansion (facial fat no longer adherent to the facial skeleton tends to fall radially away from the face).
The extended SMAS technique involves raising both a skin flap and an SMAS flap. These two flaps can then be repositioned in two different vectors. The SMAS flap, along with the superficial facial fat, can then be redirected vertically, repositioning into areas of deflation within the lateral cheek. This restores fullness to regions that have hollowed and removes bulging from areas that should be contoured, such as the jowl. The skin can then be pulled and redraped in a more horizontal plane, providing a more natural postoperative appearance. Lengthy discussions regarding facial fat descent, retaining ligaments of the face, deflation, radial expansion, and the role of skeletal support have been included in previous texts. The fat compartments of the face have similarly been well described previously in articles and texts. 2
Knowledge of the detailed anatomy of the face is imperative for performing both a safe and a successful facelift. The focus of this chapter is to provide a step-by-step guide to performing the extended SMAS technique for facelifting. The goal of this type of facelift is to provide the patient with a long-lasting result of a more youthful and natural appearance. Table 20.1 provides a list of special equipment needed.
Needle-tip bovie cautery | Portable free-standing light |
Lidocaine with epinephrine | Rubber bands, small size |
Methylene blue | Bipolar cautery |
Cotton-tip applicator | Thimble retractor |
MARKINGS
A line is drawn from a point just lateral to the lateral canthus and extending caudally toward the body of the mandible. This line should be parallel to the anterior border of the masseter. This will mark the medial extent of the subcutaneous dissection.
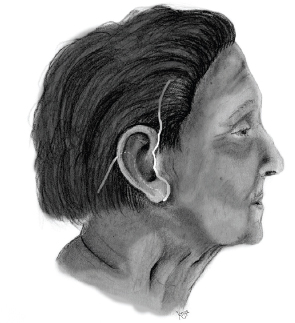
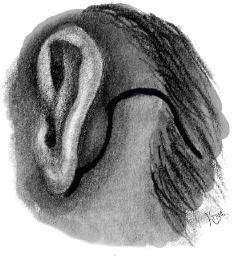
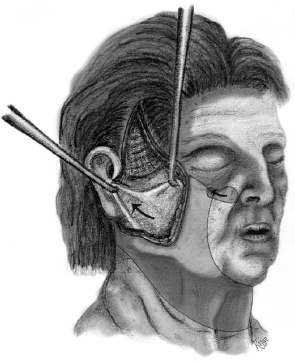
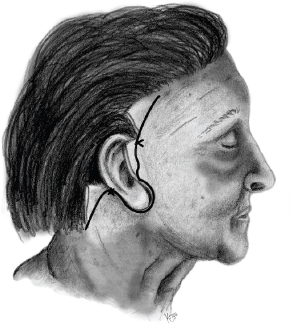
Another line is drawn starting within the hair-bearing scalp of the temporal region and extending inferiorly, anterior to the ear, within the tragus, to the inferior aspect of the ear (Figure 20.1). This intratragal incision will help avoid the telltale sign of a facelift, namely color difference between the tragus and the cheek. This line is then carried under the lobule, then up and behind the ear, in the vertical direction within the junction of the posterior concha and the postauricular skin (i.e., the conchal groove). The line takes a right-angle turn posteriorly at the point where the concha meets the hairline, and the line extends into the hair-bearing scalp of the occipital region. Finally, this line takes a gentle curve posteroinferiorly within the hair-bearing scalp (Figure 20.2).
INTRAOPERATIVE DETAILS
It is helpful to place the patient’s hair into bundles secured with individual rubber bands.
The face is prepped and draped in the usual fashion with Betadine® (Purdue Products, Stamford, CT) paint.
Lidocaine 0.5% with epinephrine is instilled along the incision lines and the planes of subcutaneous dissection.
The skin is incised through the predrawn intratragal incision extending into the temporal scalp. Of significant importance is the preservation of the incisura of the tragus, the junction of the inferior-most aspect of the tragus with the cephalad-most portion of the earlobe.
Using skin hooks, the skin is retracted, and the dissection is begun with a #15 blade scalpel and then sharp scissor dissection. Special care and meticulous attention are paid to this dissection to ensure even flaps that are not too thick or too thin. The use of a free-standing portable light source is helpful for transillumination of the other side of the skin flap to show the interface between subcutaneous fat and the SMAS. It is important not to dissect deep to the SMAS, or it will be difficult to raise an adequate SMAS flap later. It is equally important not to make the skin flaps too thin, lest they should be prone to venous congestion.
The superficial temporal artery splits into the parietal and frontal branches. The parietal branch is then identified and ligated at its takeoff. The temporal dissection is carried directly superficial to the deep temporal fascia.
The subcutaneous dissection is now carried caudally toward the neck. At this point, the skin flap can be left a little thicker than its more cranial counterpart. Note that the great auricular nerve lies beneath the SMAS along the mid-belly of the sternocleidomastoid muscle. This dissection is continued caudally over the angle of the mandible and further down into the neck overlying the platysma. The dissection is carried medially into the anterior neck forward through the submental incision, which will be incised later in the procedure.
Returning to the malar region, the subcutaneous dissection is continued until the skin is freed from the restraint of the zygomatic ligaments, toward the lateral canthus.
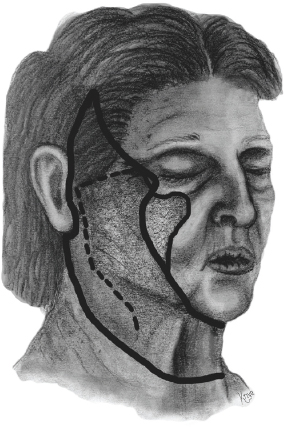
The SMAS dissection commences by first marking the path of the frontal branch of the facial nerve, keeping the SMAS dissection inferior to the line. Using the back end of a cotton-tip applicator dipped in methylene blue, a line from the tragus to the eyebrow overlying the SMAS is drawn. Cranial to this line is the area where the frontal nerve will begin to course more superficially, and staying caudal to this line will ensure its safety.
The next line that is drawn is a line 1 cm inferior and parallel to the zygomatic arch. At the point where the zygomatic arch meets the body of the zygoma, an extension of this line is carried at approximately 45° toward the lateral canthus and overlying the malar eminence for approximately 3–4 cm. This is the cranial-most extent of the SMAS dissection.
A vertical line is drawn along the SMAS paralleling the original skin incision from the zygomatic arch inferiorly along the lateral border of the platysma. This line begins at the lateral-most aspect of the previously drawn line (1 cm inferior to the zygomatic arch) and continues vertically and inferiorly along the posterior border of the platysma, approximately 5–6 cm below the mandibular border (Figure 20.3).
Now, the incision line in the SMAS and the plane beneath the SMAS are infiltrated with a solution of 0.5% lidocaine containing epinephrine.
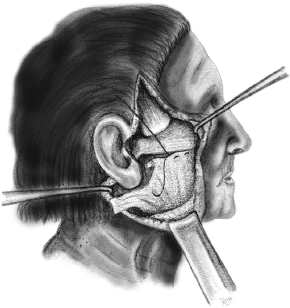
The SMAS may now be incised with a #10 scalpel. The SMAS is reflected medially with forceps with teeth, and the dissection is begun on the undersurface of the SMAS with a combination of sharp and electrocautery dissection. Keeping the dissection superficial to the parotid capsule and deep facial fascia is critical to prevent a facial nerve injury. Dissecting directly along the undersurface of the SMAS and leaving the sub-SMAS fat on top of the deep facial fascia protects underlying facial nerve branches.
This sub-SMAS dissection is carried medially until the zygomaticus major is encountered, and the SMAS is freed from the lateral zygomatic eminence superficial to the zygomaticus major.
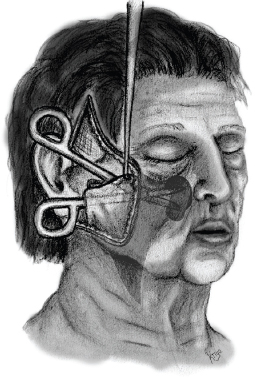
Often, the SMAS is not yet completely mobile at this point, and the sub-SMAS dissection needs to be carried further medially in the malar region. This is done by inserting scissors in the plane between the malar fat pad and the elevators of the lip. The scissors are used to bluntly dissect in a direction aiming toward the nasal ala. Of note, this is an area of SMAS dissection that does not have a skin flap dissection overlying it (Figure 20.4).
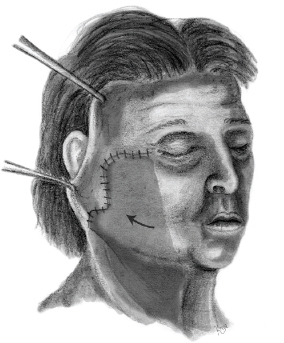
Now that the SMAS layer is free and mobile, it can be repositioned into a location that brings the facial fat pads superiorly into the regions of lateral cheek deflation. The direction of pull is vertical (Figure 20.5).
Now, if malar augmentation is deemed necessary, any SMAS that has been displaced superiorly and extends above the zygomatic arch is folded under itself to augment the malar eminence. If malar augmentation is not planned, then the remaining SMAS extending above the zygomatic arch is incised and discarded. In either case, the SMAS is split at the point that it overlaps the lobule of the ear, allowing some SMAS to be secured anterior and some SMAS to be secured posterior to the ear. The SMAS is then secured in this location with a soft absorbable suture, down to the underlying tissue and periosteum of the zygomatic arch (Figure 20.6).
The preceding steps are repeated for the opposite side of the face.
Next, a submental incision is made in a crease 5 mm caudal to the submandibular crease.
The dissection is carried out in a subcutaneous plane until the subcutaneous dissections from either side of the face meet. It is important to keep and preserve 5–6 cm of preplatysma fat on the skin flap. Following through-and-through neck dissection, excess cervical fat is sharply contoured with scissors. This dissection is aided by the use of a lighted retractor.
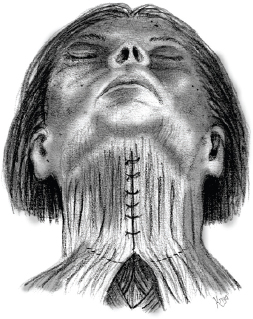
At this point, the platysma muscle can be visualized and may need to be repositioned and sutured together if it has splayed in the midline.
Next, the freed medial edges of platysma are grasped and brought toward the midline to assess redundancy. Any excess platysma should be resected.
The medial edges of the platysma muscles can be sutured together in the midline. Attempts to place these sutures through the muscular fascia should be made.
Now, an incision can be made that transects the medial portion of the platysma inferiorly. This allows the platysma to redrape itself in a more anatomic and youthful position and removes tension on the platysmaplasty. This partial platysma myotomy is performed in the lower neck, usually from a dissection of 5–6 cm on each side of the platysma, and is performed distal to the hyoid (Figure 20.7).
A small suction drain is placed into the neck, exiting the skin incision behind the ear.
After achieving meticulous hemostasis, the neck incision can be closed with 6-0 nylon suture in a simple, interrupted fashion. Hemostasis cannot be overstated. This will reduce both postoperative hematoma and edema.
The skin is now redraped, and the amount to be resected is determined (Figure 20.8). Using a #15 scalpel, the skin flap is incised in the temporal region, and key sutures are placed. A similar key suture is placed in the postauricular region (Figure 20.9).
The skin is now draped over the tragus, and the line of resection is determined. It is usually a rectangular resection and should be made with very sharp corners and some skin redundancy. This redundancy will help to prevent postoperative contraction around the tragus and subsequent external meatal “show.”
All incisions are closed with 4-0 and 6-0 nylon suture.
Fat grafting can be performed at this time if deemed necessary preoperatively.
The face is cleaned, and the hair is washed. A bulky head dressing is applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








