17 Correction of Ptosis
Pearls
Margin-reflex distance 1 (MRD1, distance from the corneal light reflex to the upper lid margin) in a sitting position is the most important parameter for ptosis evaluation.
History, levator function test, and measurement of lid lag on down-gaze help differentiate between aponeurotic and congenital ptosis.
Levator function is the most important parameter in determining the surgical method (levator advancement, frontalis sling, etc.) and the most reliable predictor of surgical response.
Mild ptosis with good levator function can be treated with conjunctivo-Müllerectomy.
Bilateral surgery is more likely to be predictable and reliable than unilateral surgery, especially in elderly patients or patients with poor levator function.
The burden factors such as redundant skin, orbicularis muscle, and fat should be addressed because they can aggravate the ptosis or cause subclinical ptosis.
Structural weakness and the pretarsal fat pad are more easily seen in the medial part among elderly East Asians, and an effort to overcome those factors is required for better results.
Additional procedures to form a lid crease after ptosis correction are usually required for a durable lid crease formation in Asian patients.
Meticulous hemostasis and intraoperative cooling are helpful in improving the accuracy of intraoperative adjustment.
Asymmetry after ptosis repair can be fixed in the early postoperative period of a week or so.
Introduction
Upper eyelid ptosis is evaluated by margin-reflex distance 1 (MRD1), which is the distance from the corneal light reflex to the upper lid margin and normally ranges from 3.5 to 4.5 mm in Caucasians. However, MRD1 depends on age, sex, and race and tends to show lower values in the elderly, males, and Asians. Unilateral ptosis is diagnosed when one eyelid is positioned over 2 mm lower than the other eyelid.
The levator palpebral muscle is the primary upper eyelid retractor. The Müller and frontalis muscles are also involved in lifting the upper eyelid. Functional or anatomic abnormalities of the upper eyelid retractors (mostly the levator muscle and aponeurosis) are the main reasons for blepharoptosis. Patients with ptosis usually show brow elevation because the frontalis muscle is overused to compensate for the weak primary upper eyelid retractor.
In contrast to true blepharoptosis, pseudoptosis is not associated with abnormalities of the retractors. Common causes of pseudoptosis are contralateral lid retraction, hypotropia, enophthalmos or contralateral exophthalmos, puffy lid in Asians, and dermatochalasis (skin redundancy without aponeurotic ptosis).
History of Ptosis Surgery
Ptosis surgery has shown many revolutionary changes as our knowledge of anatomic and physiologic processes has expanded. In addition, expansion of the variety of materials has revolutionized the field of ptosis surgery since its ancient history. References show that the earliest treatments were performed by ancient Arabian ophthalmologists. More recent descriptions were provided by Scarpa, an Italian anatomist and surgeon, in 1806.1,2 However, the references from the early days regarding the treatment of ptosis, resecting the upper part of the eyelid, were insufficient and of only temporary relevance. Therefore, alternative ways to elevate the eyelid had to be researched and developed.
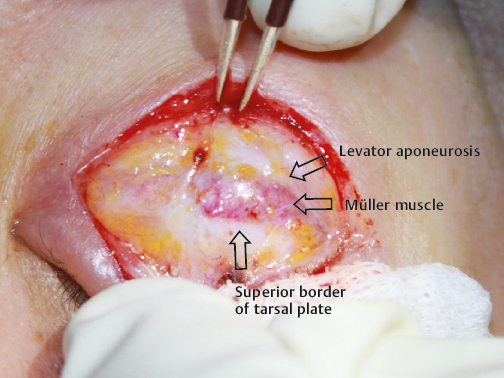
The levator muscle and aponeurosis, Müller’s muscle, and the frontalis muscle are the upper lid retractors that are the primary tissues targeted during ptosis surgery. Ptosis surgery restores or reinforces the natural power of the eyelid retractor muscles (levator muscle or Müller muscle resection). It can also produce new mechanical lifting power (frontalis suspension) with or without ancillary procedures to shorten the eyelid length or to reduce the burden factors (tarsus, skin, and fat resection). Surgical techniques along with anatomical discoveries and surgical materials have developed as follows.
Frontalis Sling
Dransart adapted exogenous material as a suspender and applied it to buried catgut sutures in 1880. Hess introduced a temporary placement of silk suture in 1893.3,4 De Wecker employed the first autogenous sling with a combination of skin, orbicularis muscle, and silk suture as a suspender.5
In 1909 Payr introduced a thigh fascia that marked a significant advance in frontalis slings and still remains one of the gold standard materials.5 Yasuna described a frontalis sling using cadaveric fascia lata, which received extensive attention during the 1970s.6,7,8,9,10,11 In 1966 Tillet recommended the use of silicone strips, which received further attention and are still in use. In 1986 Anderson suggested that sling material be placed behind the septum. This resulted in a more cosmetically acceptable appearance and a more naturallooking lid crease.12
Levator Muscle and Aponeurosis Repair
Levator surgery did not gain popularity until the end of the 19th century. More reliable alternatives such as the frontalis sling were preferred. It was Bowman who targeted the retractor muscle instead of weakening the protractor muscle for the first time.13 In 1857 he resected both the levator muscle and the tarsus using an internal/external approach.
Interest in levator surgery was revived with the introduction of an external approach, levator tucking, by Everbusch and levator aponeurosis resection by Snellen in 1883.14,15 In 1896 Wolff devised a procedure for isolating, mobilizing, and advancing the levator muscle.16 On the other hand, Blaskovics suggested an internal approach with excision of the tarsus and levator in 1909.17
Interest in the external approach was continued by Jones, who devised a surgery that advances the levator aponeurosis while preserving Müller’s muscle in 1960.18 Anderson, a great investigator of levator surgery, published his work extensively on eyelid anatomy and levator aponeurosis surgery in neuromyopathic, involutional, and mild cases of congenital ptosis, making the 1980s “the Age of Aponeurotic Awareness.”19,20,21,22 During this period, various techniques were introduced, including the manner of aponeurotic repair, the number of fixation sutures, adjustable suture techniques, and alternatives in the size or location of the incision made by a variety of instruments.21,22,23,24
Müller Muscle Surgery
Conjunctival tarsal Müllerectomy, otherwise known as the Fasanella-Servat procedure, was introduced in 1961.25 It was regarded as a type of levator resection initially but was later understood to work due to its action on Müller’s muscle. In 1972 Putterman devised a clamp and reported a modification that resects Müller’s muscle and conjunctiva while sparing the tarsus (Müller’s muscle conjunctiva resection, or MMCR).26,27
To avoid corneal irritation by sutures, Lauring reported a sutureless Fasanella-Servat operation and Bodian used external securing with 5–0 nylon suture.28,29,30 While Weinstein described a marking suture to more easily isolate Müller’s muscle and place the Putterman clamp, Iliff incorporated levator aponeurosis into the operative site with a Fasanella-Servat-like approach.31,32
Patient Evaluation
In blepharoptosis evaluation, not only the lid but also the wrinkles on the forehead, height of both eyebrows, and the presence of lid crease should be evaluated. If there is a lid crease, checking whether the crease is distinct or multiple is necessary. Occasionally, ptosis is masked by redundant eyelid skin or fat bulge, leading to an apparent ptosis after simple upper blepharoplasty. Moreover, in patients who have ptosis in the dominant eye, the other eye might have retracted due to Hering’s law. Therefore, it is important to evaluate the patient carefully prior to the surgery to detect any masked problems and thus reduce the rate of revision.
Anatomic structures of Asian lids without creases (lower orbital septum–levator fusion level with preaponeurotic fat hanging over the tarsal plate; more prominent subcutaneous, subdermal, suborbicularis, and pretarsal fat; and lower primary insertion of the levator aponeurosis onto the upper lid dermis) interfere with eye opening and can be regarded as a category of ptosis.33 By removing those burden factors instead of doing levator surgery, the surgeon can obtain excellent cosmetic improvement on a puffy, small, and droopy Asian lid.
History Taking and Physical Examination
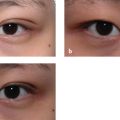
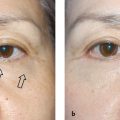
In severe unilateral ptosis, the eyebrow on one side can be elevated relative to the other with predominant forehead wrinkles. In addition to the patient’s history and age, upper lid lag is a helpful clue in distinguishing congenital ptosis from aponeurotic ptosis. If a down-gaze makes one eyelid bigger than the other, or if an up-gaze makes the eyeball hide behind the upper eyelid, congenital ptosis with poor levator function can be suspected (Fig. 17.1). Such a phenomenon occurs because of the levator muscle’s inherent inability to relax due to dysgenesis and fibrofatty degeneration. Patients with aponeurotic ptosis can have a deep superior sulcus due to the retraction of the preaponeurotic fat pad. The lid crease of an eye with ptosis gets higher due to the levator’s stretch or dehiscence (Fig. 17.2).


Since Asians often have medial epicanthal folds, medial epicanthoplasty can be performed at the same time as the ptosis surgery. It is essential to take photos before the surgery for documentation, review, education, and medicolegal purposes. Patients normally do not remember their preoperative features. By comparing the preoperative and postoperative photos, the results of the surgery can be objectively analyzed and evaluated. This helps to establish trust between the patient and the surgeon. When the patient complains, review the photos; if something is found lacking, discuss it with the patient and consider performing a revision surgery for better results. If a patient does not want photos to be taken before the surgery, the operation should be reconsidered. Photos are taken while the patient is looking ahead, up, and down. To check the conditions of the eyelashes, additional lateral view photos should be taken. If there are any important or unique occurrences during the surgery, intraoperative photos should be taken as well. To evaluate the progress of the surgery, photos are taken 1 week, 1 month, and 3 months after the surgery.
Diagnosis of Ptosis
It is important to measure the MRD and levator function to obtain proper evaluations. MRD1 is known to be the most predictable measurement for ptosis evaluation.34 MRD1 must be examined with the patient in a primary position with no excessive use of the frontalis muscle or orbicularis muscle. For an accurate exam, a light source (a pen light or flash) must be positioned at the same height as the patient’s eyes. MRD1 is the distance from the corneal light reflex to the upper eyelid margin, not the hanging skin margin. If the hanging upper lid skin is covering the upper lid margin of a patient with dermatochalasis, the skin should be gently pulled up and the lid margin should be observed during the exam. MRD2 (distance from the corneal light reflex to the lower lid margin) depends on the position of the lower lid. The sum of these two is the interpalpebral fissure (IPF).
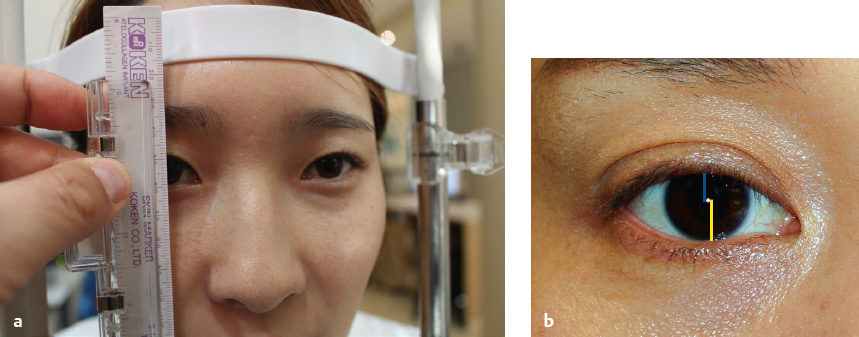
The levator function is determined by measuring the excursion of the eyelid margin, or the total distance traveled by the lid margin from down-gaze to up-gaze. A normal levator function is ~ 15 mm. Levator excursion is considered to be poor when the distance is less than 4 mm, moderate when the distance is between 5 and 10 mm, and good when the distance is above 10 mm. To prevent frontalis recruitment during these measurements, it is advisable to either have the forehead leaning on a support bar or using one’s hands to hold the forehead. By using a ruler attached to the side bar of the slit lamp, the values of MRD1, IPF, levator function, and lid lag are recorded in detail (Fig. 17.3). Using these kind of reliable records to objectively express patients’ status often builds patients’ trust.
The most common clinical ptosis occurs from stretching and dehiscence of the levator aponeurosis. Typical aponeurotic ptosis is found in cases of frequent eye rubbing due to atopy or wearing contact lenses for a long time, and senile changes due to aging. Similar cases can be found in patients after ophthalmic surgery, trauma, or frequent lid swelling.35,36 General clinical characteristics of aponeurotic ptosis include
Eyebrow elevation of the affected eye
Deep superior sulcus
Higher or multiple lid creases
Lid drooping
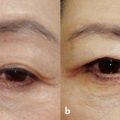
Good levator function
The lid crease height is the distance between the lid margin and the crease formed by the attachment of levator aponeurosis fibers to the subcutaneous tissue. This can vary among races and by sex. Lid crease height may increase in situations of ptosis owing to aponeurotic dehiscence.37 Levator function in patients with aponeurotic ptosis is good in general. However, if the levator aponeurosis totally detaches from the tarsal plate, the levator function will be very poor.38 This is especially true for elderly patients who have had ophthalmic surgery several times and whose levator aponeurosis is often totally detached from the tarsal plate (Fig. 17.4).

Most aponeurotic ptosis results from aging and is commonly detected in elderly patients. On the other hand, congenital ptosis is the most common type in children. Unlike aponeurotic ptosis, congenital ptosis shows poor to fair levator function and lid lag on down-gaze due to the loss of levator muscle elasticity. In some cases, incomplete lid closure (lagophthalmos) is also present. The histologic finding of congenital ptosis is dystrophy of the striate muscle fibers.39 Some patients with mild congenital ptosis are not diagnosed till adulthood.
Contact Lens–Induced Ptosis
Prolonged contact lens usage is well known to potentially cause acquired ptosis.40,41 The clinical features of aponeurotic blepharoptosis induced by the use of contact lenses do not differ from those related to other causes. Contact lensinduced ptosis can be caused by an allergic reaction to the preservatives in the contact lens solution, tarsal conjunctival irritation by the contact lens edge, and levator aponeurosis damage by physical opening of the eyelid for contact lens placement. Ptosis induced by hard contact lenses is caused by fibrosis of the Müller muscles.42
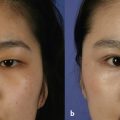
In most cases of contact lens–induced ptosis, the levator aponeurosis is connected to the tarsal plate since surgeries are performed in young and middle-aged patients. Temporary ptosis caused by contact lens usage is treated by prohibiting the use of contact lenses and prescribing antiinflammatory eye drops to reduce conjunctival swelling. Although dehiscence or rarefaction of the levator aponeurosis is more often found in patients with contact lens–induced ptosis, gross findings of aponeurotic disinsertion or defects can be observed (Fig. 17.5).
Phenylephrine Test
It was Dortzbach who found that a phenylephrine test is useful to predict the postoperative lid position after Müller’s muscle resection.43 A drop of 10% or 2.5% phenylephrine is instilled in cases of mild ptosis with good levator function. Once the eyelid goes up to a normal position, it is regarded to be a good candidate for a conjunctivo-Müllerectomy. This method is advantageous for patients who need unilateral surgery and do not want skin excision or any chance of getting a skin scar.
Preoperative Considerations
Eye Protective Function
Since ptosis surgery basically pulls the upper lids upward, lagophthalmos may occur temporarily in the early postoperative stage or become permanent. To avoid this complication, one should check the patient’s eye protective mechanisms and inform the patient of inevitable problems such as lid lag and lagophthalmos. Conditions such as significant dry eye syndrome, facial palsy, dysfunction of the superior rectus muscle, and absence of Bell’s phenomenon must be checked prior to the surgery. If the protective function is weak or absent, overcorrection should be avoided.
Visual Field Test
A visual field test is often needed for insurance coverage purposes in the Republic of Korea. Surgery on a droopy upper lid blocking the pupil is covered by insurance there.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree