16 Lower Blepharoplasty
Pearls
The surgical procedure of lower blepharoplasty evolved from fat and skin excision into volume enhancement. A customized approach considering each patient’s lower eyelid configuration is essential to the success of surgery.
Surgeons must discuss what they can or cannot do with patients. Fine or dynamic wrinkles, local skin pigmentation, or skin scars cannot be addressed with lower blepharoplasty, and this should be acknowledged to the patients who want lower blepharoplasty.
The surgeon should choose an approach: transconjunctival versus transcutaneous. A transconjunctival approach is ideal for patients who show fat prolapse without skin or eyelid laxity. A transconjunctival approach is also applicable for those who don’t want a skin scar, who are undergoing reoperation for fat prolapse, or who have a tendency to develop hyperpigmentation on a skin incision site.
The surgeon must decide how much orbital fat is to be removed or redistributed. If tear trough depression is evident relative to fat prolapse, fat redistribution is recommended to avoid a postoperative hollow appearance. Gentle pressure to the globe is helpful in deciding whether or how much fat excision is needed because lying down on a surgical table does not simulate the conditions of sitting up.
The surgeon must assess the degree of lower eyelid laxity with a snap-back test or a lid distraction test and must perform a horizontal lid tightening procedure if the laxity is significant enough to affect postoperative lower lid retraction.
During the fat redistribution procedure, ocular movement should not be restricted on a fat anchoring suture. If there is movement restriction, release the suture, perform further dissection, and confirm that movement is not hindered by a refixation suture.
Proper hemostasis is needed during orbital fat resection to avoid the disastrous complication of orbital hemorrhage. Traction on the fat tissue should be minimized to avoid hemorrhage from the deeper orbit, and a clamp-cut-cautery technique is recommended for resection of the medial fat pocket harboring relatively large-bored blood vessels.
The skin excision should be conservative to avoid lower eyelid retraction during transcutaneous blepharoplasty. It is helpful to have the patient open his or her mouth and look up when the skin excision amount is measured with a draping method, to minimize skin over-resection.
Postoperative caution should be stressed to the patient to prevent orbital hemorrhage. Cold compression is recommended for 48 hours, and avoidance of head down positioning and of physical exertion should be emphasized.
Introduction
The demand for blepharoplasty among persons of East Asian descent is increasing in the United States. In a 2013 plastic surgery statistics report, Asians/Pacific Islanders accounted for 6.2% of all cosmetic blepharoplasty procedures in the United States; the proportion for this procedure was the highest among all cosmetic surgical procedures.1
For successful blepharoplasty for Asians, understanding of the characteristic features of the eyelid is most important. Asian faces have more melanin pigment and thicker skin, so the incision scar from surgery can be hypertrophied or hyperpigmented.2 Lower eyelids of Asians are characterized by a fuller appearance than those of Caucasians, which is caused by protruded orbital fat.3 Asians have heavier soft tissue and larger amounts of malar fat, which are subjected to greater gravitational force.2 The eyelid and adjacent structures are tight; sometimes wider incisions and exposures have been advocated in periocular surgeries for Asian patients.4,5 Therefore, preoperative evaluation, judicious skin manipulation, and proper postoperative care are important to ensure a good surgical outcome for Asian lower eyelid blepharoplasty.
The concept of aging in lower blepharoplasty has been changed. In conventional thought, the periocular aging change was regarded as the result of the descent of midface, unopposing, weakened supporting structures and orbital fat prolapse. After the volume deflation concept was introduced in the interpretation of the aging process, aesthetic approaches to patients have been modified tremendously.
In the historical view of surgical management of the lower eyelid aging process, the prototype procedure was orbital fat excision with a transcutaneous approach. Lower lid tightening procedures were developed to prevent or treat eyelid malposition, which was the most common complication of the conventional technique.6,7,8 The transconjunctival approach subsequently became popular in blepharoplasty, as it could prevent postoperative eyelid retraction and leave no visible scar while providing wide exposure.9 Since the transconjunctival approach was applicable only to patients who did not need skin excision, the concomitant skin pinch technique was used to address the excess skin in transconjunctival blepharoplasty.
However, for patients who had pseudoherniation of the fat and tear trough depression, removing lower eyelid fat can create a concave contour deformity of the lower eyelids and cause a hollow appearance.10 In addition, deepening of the superior sulcus has been noted after the orbital fat removal procedure.11 Therefore, volume enhancement has become an important issue in rejuvenation of the lower eyelid. Consequently, a customized approach to each patient is essential; the specific configuration of each patient needs to be assessed and addressed.12
Patient Evaluation
Goldberg et al analyzed the configuration of aging lower eyelids in patients seeking aesthetic surgery and revealed anatomic factors contributing to eyelid bags.12 They assessed patients in six anatomic categories; tear trough depression was the most significant contributing factor, followed by orbital fat prolapse, loss of skin elasticity, eyelid fluid, orbicularis prominence, and triangular malar mound. In an analysis of lower eyelid aging in an Asian population, Asians showed a tendency toward less contribution of tear trough defect and more contribution of fat prolapse to eyelid bags compared with Caucasian patients.13 The periocular aging changes can be assessed by analyzing these categories.
Tear Trough Depression and Palpebromalar Groove
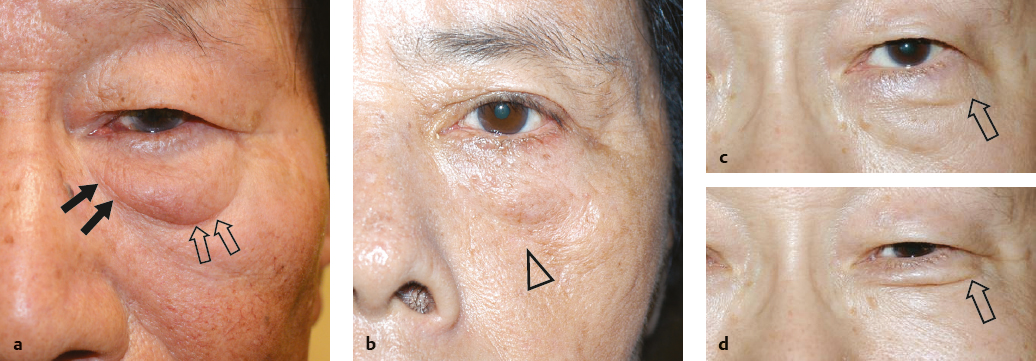
Tear trough depression occurs at the inferomedial aspect of the lower eyelid. With aging, this deformity is seen more prominently (Fig. 16.1). Tear trough depression is known to be characterized by loss of subcutaneous fat and skin thickness along with the inferomedial orbital rim, which is accentuated by fat prolapse and cheek descent.14 In a microscopic study comparing the young and the aged, the elderly individuals showed significant tissue atrophy in various layers, malar fat atrophy and descent, and orbital fat bulging.15
To correct tear trough depression, various techniques have been tried, including fat redraping blepharoplasty, various injections, and tear trough implants of various designs. Fat injection is not a recommended procedure for this region because injected fat tends to leave small, firm nodules of fat and scarring, and provides irregularity and shadows. Filler injection such as hyaluronic acid gel is increasing in this region and gets favorable results; however, repeated injections are needed.16
The volume change in the tear trough area was addressed by Hamra with fat preservation blepharoplasty, which corresponded to an epoch in lower blepharoplasty.10 Since then, several modifications have been introduced. The procedure can be performed transconjunctivally or transcutaneously, and the fat can be transposed subperiosteally or supraperiosteally.4,17,18,19,20
To address the palpebromalar groove, an orbital rim depression of the central to lateral region, orbital retaining ligament release is an important step that can be combined with suborbicularis oculi fat (SOOF) elevation or the orbicularis tightening procedure.15,19
Since Asian patients have relatively thicker skin and subcutaneous tissue at the tear trough or palpebromalar region, the fat resection procedure alone can achieve a good cosmetic outcome in selected cases.21
Orbital Fat Prolapse
Three orbital fat compartments are separated by inferior oblique and arcuate expansion. The pockets are called medial, central, and lateral fat pockets. It is important to have the patient look up during examination because the fat pockets are more noticeable when the patient is looking up. It is also useful to have the patient lie down, mimicking intraoperative state, and to see the degree of retroposition of fat preoperatively.
The total volumes of intraorbital fat and fat anterior to the inferior orbital rim have been shown to increase until 60 years of age and then decrease, in a study of computed tomography (CT) analysis for Koreans.22 Therefore, an increase in orbital fat volume is considered to contribute to lower eyelid prominence in Asian patients. As Asian patients have substantially more protruded orbital fat, many articles have asserted the importance of fat resection during lower blepharoplasty for Asians.15 Fat removal was also stressed in another group, saying that an Asian patient with a brachiocephalic face may not be a good candidate for the fat transposition procedure unless it is modified by more fat removal.5 Of note, fat resection should be performed judiciously, especially for the aged, to avoid a hollow look postoperatively.
Loss of Skin Elasticity
The lower eyelid skin shows wrinkles and grooves resulting from sun damage and subcutaneous volume loss. A skin tightening procedure is considered if a significant amount of skin laxity is encountered, including surgical resection, chemical peeling, or laser skin resurfacing. In Asian patients, skin erythema and hyperpigmentation can result from skin surface ablation treatment; therefore, care should be taken in deciding the treatment modality for each patient.23
Eyelid Fluid
If fluid is accumulated in the lower eyelid from systemic or local edema, it can mimic fat prolapse. It can be distinguished by its diffuse nature, fluctuation in degree, lack of compartmentalization, or purplish color when it is severe.12
Even though the presentation of eyelid fluid was found to be very rare in a Korean study, it should be one of the differential diagnoses of fat prolapse in Asian people.13
Orbicularis Prominence
Orbicularis oculi prominence also contributes to lower eyelid aging features, with static and dynamic wrinkles. Horizontal or oblique lines accentuated with facial expressions can be noticed in many patients, and may be more common in Asian patients (Fig. 16.1c,d ).13,24
Orbicularis prominence can be dealt with by the orbicularis oculi suspension procedure in blepharoplasty.
Triangular Malar Mound
The triangular malar mound is a fluid sponge bound above by the orbital rim ligament and below by the orbitozygomatic ligament.13 This is relatively rare in Asian patients.13
Position of the Globe and the Inferior Orbital Rim
The relative position of the globe and inferior orbital rim should be examined preoperatively because this is helpful in deciding which procedure is appropriate for each patient. In the sagittal plane, when the anterior margin of the inferior orbital rim is posterior to the anterior-most point of the cornea, the patient has a negative vector anatomy (Fig. 16.1b ). Patients with a negative vector tend to have preoperative scleral show due to midfacial hypoplasia. Simple excision of the orbital fat often leads to exacerbation of the tear trough depression and increased scleral show. Patients in this category should be considered for fatpreserving blepharoplasty.
If the anterior margin of the inferior orbital rim is anterior to the anterior-most point of the cornea, the patient has a positive vector anatomy. For a patient with positive vector, conservative excision of fat is recommended.
Lower Eyelid Laxity
The most significant complication related to lower blepharoplasty is eyelid malposition such as retraction or ectropion.6 To prevent these complications, preoperative evaluation of the lower eyelid laxity is important.8
First of all, the eyelid position needs to be recorded as margin-to-reflex distance 2 (MRD2), which is defined as the distance from the lower eyelid to the corneal light reflex, to document the amount of preoperative eyelid retraction, if present.
Eyelid laxity can be determined by the snap-back test or the distraction test. With a snap-back test, the restoring force of the lower eyelid can be assessed after downward eversion of the eyelid. If the eyelid goes back to its normal position instantly, the horizontal tightening procedure won’t be necessary. If the eyelid goes back after blinking, horizontal tightening procedures such as orbicularis oculi suspension might be needed. If the eyelid does not go back even after blinking, a lateral tarsal strip procedure is recommended to avoid eyelid retraction after blepharoplasty.
With a distraction test (forward traction test), medial and lateral canthal ligament and eyelid laxity can be assessed. If the eyelid can be pulled over 8 mm from the cornea with forward traction of the eyelid, a horizontal tightening procedure is recommended.
Surgical Considerations in Asian Patients
For patients requiring lower eyelid blepharoplasty, significant factors in the aging process in each patient should be assessed and suggestive surgical methods discussed with the patient.25
If a patient shows fairly good skin tone, simple fat excision with the transconjunctival approach is the first choice for primary eyelid bags.21,25 If a patient has redundant skin and wrinkles without significant laxity of the eyelid, transconjunctival fat removal with pinch skin excision or transcutaneous fat excision blepharoplasty can be performed.24 The orbicularis muscle tightening procedure can be added to transcutaneous blepharoplasty for those who show moderate eyelid laxity.
If a patient has a tear trough depression and midface sagging resulting in significant volume depletion at the inferomedial orbital rim, fat transposition blepharoplasty is needed transconjunctivally or transcutaneously.26 If the patient shows significant palpebromalar groove, orbicularis retaining ligament release and orbicularis suspension and/or SOOF lift are recommended.
Photographs should be taken preoperatively with eyelid closed and open and with the patient looking up and down. These photos are for legal protection or in case of postoperative patient dissatisfaction.
Surgical Techniques
Transconjunctival Fat Excision Blepharoplasty
With the transconjunctival approach, the integrity of the orbicularis muscle and the orbital septum can be maintained. Equal exposure to the fat pads is provided with the transcutaneous approach, and the skin pinch technique is allowed for redundant skin.
Conjunctival Incision
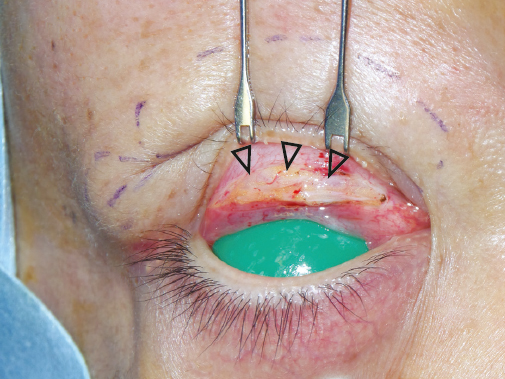
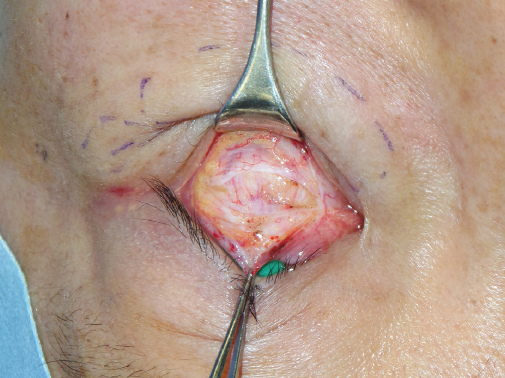
Before surgery, assess the amount of prolapsed orbital fat from each compartment while the patient sits up. Wait 15 minutes for hemostasis after local anesthetic injection into the subconjunctival space and fat pockets. Make a conjunctival incision 3 to 4 mm below the inferior margin of the tarsus (Fig. 16.2), and proceed to dissect toward the inferior orbital rim until the orbital fat pockets are exposed (Fig. 16.3). With this approach, there is no scar formation on the orbital septum because the septum is not violated. This retroseptal transconjunctival approach can avoid the common complications of lower lid blepharoplasty such as eyelid retraction and scleral show.
A preseptal transconjunctival lower blepharoplasty is also performed by some surgeons: a conjunctival incision is made below the tarsus, dissection then proceeds inferiorly, and a preseptal space is assessed. The orbital septum is opened to expose the orbital fat. Proponents of the preseptal approach suggest that the scar formation on the septum may bolster against the pseudo-herniation postoperatively. No significant difference in eyelid position between preand retro-septal approaches has been reported.27,28
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree