14 Bilateral Cleft Lip
Summary
Repair of bilateral cleft lip has been regarded by many to be among the most challenging and rewarding of plastic surgical procedures. Methods of repair have evolved considerably over the past several decades. Presently, all repairs should be soundly founded in the modern principles that have been distilled and clarified from this evolutionary process. This chapter presents a practical synthesis and application of those principles to contemporary bilateral cleft lip repair, in the style of Mulliken.
14.1 Introduction
A number of infants born with bilateral cleft lip undergo old-fashioned, often multistaged, procedures, and later, they have to endure sundry revisions throughout childhood and adolescence. Despite the surgeon’s best efforts, the stigmata of the repaired cleft lip and nose remain painfully obvious—even at a distance. To the contrary, … the appearance of a child with repaired bilateral cleft lip should be comparable to, and in many instances surpass, that of a repaired unilateral cleft lip. — John B. Mulliken
This chapter provides an introduction to the operative treatment of bilateral cleft lip, with or without cleft alveolus and with or without cleft palate. The history of bilateral cleft lip repair is rich, interesting, and lengthy. For those interested, a thorough recounting of this history is available. This chapter focuses on a practical synthesis and application of the principles that have been distilled from this evolutionary process.
14.2 Anatomy, Terminology, and Classification
A history of classification systems for cleft lip or palate summarizes the major types of the bilateral paramedian orofacial cleft deformity, as follows (Table 14‑1):
“Lesser-form” cleft lip is an “umbrella term” that may be further described as minor-form, microform, or mini-microform cleft lip.
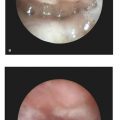
If the two sides of the bilateral cleft lip are clefted to the same degree (e.g., bilateral complete and bilateral incomplete), the cleft is termed symmetric. Contrarily, if the two sides of the bilateral cleft lip are clefted to different degrees (e.g., complete + incomplete and complete + lesser form), then the cleft is termed asymmetric. The ontological qualifier “symmetric” considers the severity of only the preforaminal (labial and alveolar) clefts on each side; the term does not encompass other aspects of symmetry that are important to the surgeon, such as the possibility of a deviated premaxilla that is situated closer to one side than the other (Fig. 14‑1).

Premaxillary malpositioning will occur only if the alveolar arch is clefted. In the typical bilateral symmetric cleft lip (e.g., bilateral complete and bilateral incomplete), the premaxilla and vomer usually remain in the midline (nondeviated). In the bilateral complete case, the prolabium is separated from the lateral labial elements and the premaxilla is separated from the lateral alveolar processes; this allows unrestrained growth of the vomer and results in anterior projection and/or proclination of the premaxillary segment. In the bilateral incomplete case, the retention by the partial labial and/or partial alveolar attachment may prevent projection and proclination. In bilateral asymmetric cleft lip (e.g., complete + incomplete), an imbalance of retention forces on one side versus the other results in deviation of the premaxilla toward the lesser side.
The morphology of any palatal cleft that may be present will also have an effect on the position of the premaxilla and vomer. In the typical case of bilateral cleft lip with cleft palate, the palatal cleft is morphologically Veau-IV (i.e., a midline cleft of the secondary palate, with exposure of the vomer and bilateral extension through each alveolar process). Of course, it is possible for the palatal cleft to be morphologically different (i.e., Veau-III, Veau-II, and Veau-I), and it is therefore important to describe the morphology of the cleft palate in the complete description of the cleft phenotype. Veau-III cleft palate (unilateral complete cleft through one side of the alveolar arch, with vomerine attachment to the contralateral palatal shelf) results in appreciable deviation of the vomer and premaxilla.
The anatomic details of the bilateral cleft are important for preoperative planning and intraoperative treatment. In the text that follows, we will use a shorthand notation to describe specific phenotypic cases: bCL, bCLA, and bCLAP for bilateral cleft lip; bilateral cleft lip and alveolus; and bilateral cleft lip, alveolus, and palate, respectively. If more phenotypic detail is of significance to the discussion, it will be described in longhand.
14.3 Planning
14.3.1 Principles
The modern approach to primary repair of the bilateral cleft lip and related nasal deformity is founded on several guiding principles:
Maintain (or establish) symmetry.
Prepare the projecting premaxilla.
Anticipate fourth-dimensional changes that occur with growth.
Construct a full central lip by using lateral labial elements and discard prolabial vermilion.
Deepen the gingivolabial sulcus by using premaxillary mucosa.
Establish muscular continuity primarily.
Address the nasal deformity synchronously.
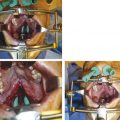
The first three principles relate to operative planning or preparation, whereas the remaining principles relate to technical details that should be executed skillfully during the operative repair. For thorough exploration of these principles and the history behind them, the reader may refer to Mulliken and Allori and Marcus. Disregard for some of these principles may lead to inferior outcomes and the stigmata of bilateral cleft lip repair (Fig. 14‑2).

14.3.2 Treatment Algorithm
Presentation in Infancy
Ideally, a cleft team will first encounter an infant with cleft lip and/or palate (CL/P) in the neonatal period, perhaps after previously having met the then-expectant parents in prenatal consultation. The purpose of the first encounter is to examine the child, document an accurate phenotype, and begin to formulate and coordinate the treatment plan; to evaluate feeding and nutrition and provide feeding education and support; and to begin the process of preoperative education for the parents.
As described elsewhere in this textbook, protocols for treatment of a child with CL/P may differ from center to center. Generally, the early surgical timeline for a child who presents with the condition in infancy proceeds as follows (Table 14‑2):
For a child with bCL (with intact alveolus and palate), the surgeon may proceed with primary labial repair directly.
For bCLA or bCLAP, the cleft surgeon should first determine whether presurgical orthopedics is indicated and available. If so, this process should be initiated as early as possible in order to achieve maximal effectiveness in a timely fashion, so that operative treatment is not unduly delayed. Presurgical orthopedics is described in detail in a subsequent section of this chapter. In centers where presurgical orthopedics is not available, bilateral labial or nasolabial adhesion may be performed instead. Nasolabial adhesion achieves some of the same effects as presurgical orthopedics on premaxillary repositioning from the natural retrograde pull of the labial elements. Nasolabial adhesion is described in section “Adhesion Cheiloplasty: Labial Adhesion and Nasolabial Adhesion.”
Nasolabial adhesion may be performed for another reason: it may be utilized to great effect in case of bilateral asymmetric case, in order to preliminarily establish better symmetry before proceeding with lip repair. For example, in case of complete + incomplete bCLA, nasolabial adhesion may be performed unilaterally on the complete side, effectively converting the asymmetric phenotype into symmetric bilateral incomplete cleft lip and alveolus. The primary labial repair that follows is thereby facilitated in both the design and the execution of the repair. In deciding whether to include nasolabial adhesion for this purpose in his or her treatment protocol, the cleft surgeon must weigh the relative benefit of improved symmetry with the risk and burden of the extra anesthetic and operative procedure.
Late Presentation
For many reasons, including significant comorbidities and international adoption, some children may first present to the cleft team at an older age. At this time, malposition of the premaxilla poses a greater challenge due to the strength and rigidity of the vomer in an older child; that is, although the vomer of the neonate may be “buckled” by presurgical orthopedic techniques or by nasolabial adhesion, this is no longer possible in the older child.
If the premaxillary projection or proclination in the older child is minor, it may be possible to perform preliminary adhesion or to proceed directly to labial repair, with minimal tension on the labial repair. On the other hand, if the premaxilla is severely projecting or proclined, this precludes a safe and effective labial repair, because the gap that must be spanned by the cutaneous and muscular closure is too great and will be under excessive tension. In order to repair the lip over this gap, the surgeon is forced to design an unaesthetically wide philtral flap; moreover, the size of the gap makes continuous muscular approximation difficult and gingivoperiosteoplasty (GPP) impossible.
In addition to the challenges of premaxillary projection or proclination, premaxillary deviation is also difficult to correct in the older child. This deviation results in an asymmetry that cannot be compensated for merely by alteration of the design of the repair.
In such cases, the skeletal malposition requires a skeletal correction: premaxillary ostectomy and setback. This procedure is described in section 14.3, “Premaxillary Ostectomy and Setback”. Importantly, premaxillary setback must be done as a preliminary procedure and should never be combined with primary cheiloplasty. In premaxillary ostectomy, the division of the vomer disrupts the posterior blood supply to the premaxilla, leaving the premaxilla totally dependent on anterior blood supply from the prolabium. If the philtral flap is dissected and raised, this will also eliminate the anterior blood supply, risking avascular necrosis of the premaxilla. Consequently, if premaxillary ostectomy and setback are necessary, they must be done 3 to 4 months before the lip repair. It is safe to combine premaxillary ostectomy and setback with either nasolabial adhesion (in case of bCLA) or palatoplasty with GPP (in case of bCLAP). These procedures improve the fixation and support of the retropositioned premaxilla, while respecting its prolabial blood supply. In additionally, in case of an older child with bCLAP, performing palatoplasty at this time efficiently combines two procedures that this child needs under one anesthetic. The definitive labial repair (with inherent elevation of the philtral flap) may be safely performed approximately 3 to 4 months following the premaxillary setback.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree