Loss of hair-bearing tissue in the head and neck area can result from surgery, trauma, burns, tumors, and infection, as well as a diversity of inflammatory conditions, and the resulting defect can present a challenging problem for the reconstructive surgeon. Hair transplantation can be used as a reconstructive method alone or in conjunction with other techniques. The current method of using follicular unit grafts has led to natural restorations for a variety of areas including not only the scalp but also eyebrows, eyelashes, and beard areas. Camouflage provided by hair grafts can provide restoration not obtainable with other methods.
Loss of hair-bearing tissue in the head and neck area can result from surgery, trauma, burns, tumors, and infection, as well as a diversity of inflammatory conditions such as lichen plano pilaris, which causes irreversible damage to the hair follicle. The resulting defect can be cosmetically disfiguring and can present a challenging problem for the reconstructive surgeon. Several well-established treatment modalities have been used for reconstruction of these areas including secondary intention, primary closure, local flaps, skin grafts, allografts, free flaps, and hair transplantation.
Hair transplantation can be used as a reconstructive method alone or in conjunction with the other techniques. The use of hair grafts for scar camouflage was used as early as the 1970s, during which punch grafting was the method of treatment. Standard punch grafting is what generally created a “doll’s hair” appearance. Hair transplantation has evolved over the decades, and the current method of using follicular unit grafts has led to very natural restorations for a variety of areas including not only the scalp but also the eyebrows, eyelashes, and the beard areas. The hair used for facial hair transplants can be harvested from the occipital and temporal areas, the same donor region as is used for restoration of the scalp.
Norman Orentreich described a key concept called “donor dominance,” which has helped to form the foundation of hair restoration. He stated that donor hair characteristics such as texture, color, growth rate, and anagen (growth) period are maintained after transplantation and that the transplanted hair behaves independently of the recipient site. Although the concept of donor dominance is not as straightforward as originally thought, transplanted facial hair will grow with similar properties to that of the donor site, thus requiring trimming and grooming. The camouflage provided by hair grafts can provide a restoration not obtainable with other methods. One’s surgical armamentarium will be greatly complemented by offering this technique, affording a more comprehensive approach to treating these patients.
Follicular unit transplantation
Understanding the basic concepts of follicular transplantation is critical when approaching patients requiring reconstruction of scarring in the hair-bearing regions of the head and neck. The concept of the follicular unit was described in 1984 and has revolutionized the preparation of the grafts, allowing surgeons to create a much more natural-appearing recipient bed. While studying the horizontal histology of the scalp, it was found that hairs grow in natural groupings of 1, 2, 3, or 4 terminal hairs with their own neurovascular bundles, a piloerectile muscle, sebaceous gland, sweat gland, and subcutaneous fat, all surrounded by a sheath of collagen. Today, as surgeons dissect these follicular units under magnification the aim is to keep them as intact as possible.
Hair transplantation involves aesthetically redistributing follicular units from the donor site to a much larger recipient site with the goal of maximizing the cosmetic impact of the surgery. It is important to recognize that recreating 50% of the native density on the scalp will create an excellent optical cosmetic density. If the demand outweighs the supply, grafts may be “weighted” to improve optical density in more cosmetically important areas such as the front or the side that the hair is combed from. Recipient site density may vary from 20 follicular units/cm 2 to 65 follicular units/cm 2 . One needs to balance the desire to create an ideal cosmetic density with the donor supply available as well as the survival of the grafts. It is critical that the patient also understands this concept.
Placing more than 30 follicular units/cm 2 into normal tissue is considered “dense packing” (although this term is variably defined by hair transplant surgeons). Dense packing may risk poor growth of the grafts and even skin necrosis depending on the vascularity of the recipient site. There is some debate regarding what the ideal cosmetic density is, but most would not argue with the safety and cosmetic outcome of creating a density of approximately 35 follicular units/cm 2 . In a normally vascularized area the graft survival rate ranges between 90% and 95%. In reconstructive cases, the vascular supply that will support the newly transplanted grafts must be considered. If significantly compromised, one should not dense pack, and the patient and his or her family must be informed that 2 to 3 or even 4 sessions may be necessary for a more optimal result.
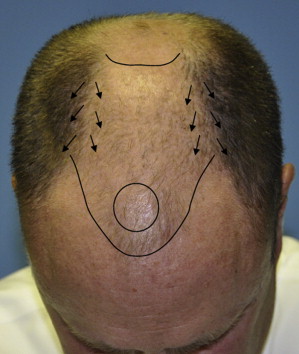
To optimally camouflage a scar in the hair-bearing scalp, it is important to understand and recreate patterns found in nature. For a male, the anterior hair line should originate where the vertical forehead changes to horizontal caudal scalp ( Fig. 1 ) approximately 8 cm above the glabella. Typically, a slightly flared line then joins the temporal hump laterally at the vertical level of the lateral canthus to create the frontal hairline contour ( Fig. 2 ). The design of the female hairline differs from that of the male in that the hairline should start at a height of approximately 5.5 cm above the glabella and frequently has a “widow’s peak” and lateral mounds. Hairline design is a topic of continual debate and discussion. Transition zones of 1-hair and 2-hair grafts are used at the hairline with 3-hair and 4-hair grafts preserved for the center of the parietal scalp. Macroirregularity and microirregularity of the grafts are also used in these transition zones to create a natural appearance. When reconstructing a scarred region in the crown, it is important to recognize the whorl patterns that occur naturally. The S-shaped pattern ( Fig. 3 ) is the most common pattern seen in Caucasian men. Designing the recipient site is the art of hair restoration. It is critical to pay close attention to the native hair as well as the patient’s preferences and styling patterns when creating the design for maximum camouflage.


When developing a treatment plan, one should always consider the patient’s personal and family history of androgenic alopecia. A history of advanced balding on either side of the family is a great risk factor for progressive hair loss in the patient as well. When appropriate, scalp recipient sites should always be designed with future hair loss in mind to avoid the cosmetic deformity that can occur as miniaturized hair recedes away from genetically stable transplanted hair. These patients should be encouraged to start on medical therapy to preserve the hair that they have and, if future hair loss is anticipated, they should be educated about the potential need for more hair grafting as their hair recedes.
Once the recipient site is designed, donor hair is harvested from the occipital scalp in the region just above the external occipital protuberance where the hair is genetically stable ( Fig. 4 ). It is in this region where the density is greatest on the scalp is most resistant to hormone-related alopecia. When evaluating the donor site, the length of the donor region can be measured from 3 cm behind the hairline at the temple to a corresponding spot on the contralateral side. The hair transplantation surgeon should always keep in mind the limited donor reservoir of good genetic hair available, which is approximately 30 × 4 cm. As a general rule of thumb, half of the donor area may be moved (in total) without a significant change in appearance. Strips measuring less than 1.5 cm in width are less likely to result in a widened scar. The amount of donor hair available is dependent on the density of hair present as well as the laxity of the scalp in the occipital area. These two factors can be compromised by injury and previous scalp surgery. If the scalp has been stretched from previous surgery, the follicular units will be spaced further apart. Scarring in the donor area will also have a significant impact on the ultimate donor yield. It is important to measure the patient’s scalp laxity and density to determine the width of the strip that can be harvested to meet the needs of the recipient site.

The harvesting of donor hairs can be performed using either the strip technique or follicular unit extraction. With the strip technique, an appropriately sized elongated ellipse of donor scalp is harvested just deep to the follicles and closed. With follicular unit extraction (FUE), follicular units are directly extracted from the donor area using a small punch that may leave an inconspicuous scar; this may be a better technique for patients who like to wear their hair very short. When donor hair reserves are scarce, FUE may also be used to harvest body hair for grafting, termed body hair transplant. One region where the use of FUE can be helpful is in the case of a wide occipital donor scar. While generally one can prevent a widened donor scar by harvesting long narrow strips, widened scars are still seen, especially in the patient who has undergone multiple hair transplant surgeries in the past. Because of the limited scalp laxity and often depleted donor reserve, FUE is an excellent method for restoration of this scar. Although FUE is an exciting alternative to the strip technique, hair transection on extraction as well as other technical problems exist and thus limit its use by many hair surgeons.
Once the donor hair is harvested, the excess tissue between each unit is dissected away while the germinative and vital support components of each unit are preserved. Hair grafts are free tissue grafts that survive only by anaerobic metabolism. Any desiccation, trauma, or increase in metabolic or ischemia time will influence the final survival rate of the transplanted follicles. Efforts to reduce ischemia-reperfusion injury and improve graft survival have led to experimentation with different storage solutions for the purpose of delayed transplantation. Grafts may be stored in a Petri dish containing 4% saline or lactated Ringer solution; however, there are now other commercially available solutions such as HypoThermosol (BioLife Solutions Inc, Bothell, WA) that contain antioxidants such as vitamin E and glutathione, which may alleviate ischemia-reperfusion injury. Following creation of the follicular units, recipient incisions are made according to the design developed preoperatively, and the hair is transplanted to the recipient area. After the grafts are placed, nutrients from the recipient bed enable survival until circulation is established days later.
As previously mentioned, the concept of donor dominance has formed the foundation of hair restoration; however, it is now understood that the recipient site has some influence on the growth characteristics of transplanted hairs. The cell cycle such as the anagen phase may be influenced by the recipient bed on the background of innate programming of the follicle when hairs are transplanted to sites away from the scalp. This concept becomes more relevant as one continues to graft hair-bearing regions outside of the scalp (ie, the face) with scalp hair.
The face is the second most common area for hair transplantation, and can include eyebrows, eyelashes, moustaches, and beards. It is important to pay attention to the hair patterns present in the recipient site so as to mimic these properties when transplanting hairs to scars in these regions. The hair on the face does not grow in follicular units, and single-hair grafts should be used when transplanting the beard. Two to 3 hair grafts may be used toward the center of the moustache to improve density.
The eyebrows and eyelashes are especially sensitive to the direction of the recipient incision and exit angle of the hair shaft and, hence, growth direction of the hair. The transplanted hair shaft should be left longer to facilitate better control of hair direction during implantation into the recipient site. Donor hair may be taken from the occipital scalp, temple, or other areas such as the postauricular region, brow, and nasal vibrissae, to closer mimic the hair qualities such as shaft diameter and anagen phase duration. In the eyebrow, incisions should be nearly parallel to the skin surface so that the hairs grow almost flat against the skin surface as in natural eyebrows. Mostly 1-hair grafts should be used, although some 2-hair grafts can be placed centrally. When restoring an eyebrow, 150 to 200 grafts may be used per brow with the superiormost hairs angled inferiorly and the inferior edge angled superiorly. For eyelid hair grafts, many techniques are being developed and used by hair restoration surgeons around the world. Depending on technique, approximately 60 hairs per lid may be grafted. The majority of the epithelium should be trimmed off to avoid hordoleum (stye). The incisions may be made in a variety of ways to produce an exit site at the ciliary margin overlapping the original eyelash at an angle of about 30° with the curl of the hair facing upward. Grooming, trimming, and curling of the hairs is typically necessary.
Hair grafting for scars
Preventing visible scars in hair-bearing regions is always preferable to requiring a second surgery for scar camouflage. Although good results can be obtained with trichophytic closures, growth of hair through the scar can result in ingrown hairs and irregularity of growth direction. When making incisions parallel to the hair follicles, despite tension-free closures, incisions often leave a visible hairless linear scar. A method that may be used adjunctively is to place hair grafts dissected from the corners of skin after excising a benign lesion that would have otherwise been discarded, and placing them into the newly closed wound to conceal an anticipated scar after a tension-free closure. Once the wound has been closed, hair grafts are dissected using a standard technique from the excised hair-bearing skin; these can then be inserted into the wound in between adjacent sutures using jeweler’s forceps. It is not well understood how this may affect the tensile strength of the wound, and it is recommended that sutures be left in place several days longer than usual. This delay saves the patient from a second operation.
Hair grafting for scar camouflage is a critical component of a multimodality approach to scar improvement, and is an accepted part of the standard of care in the reconstruction of scars in hair-bearing areas. Hair grafting can be used alone or in conjunction with other methods such as serial excision or scalp expansion/reduction. Follicular unit transplants have the advantage of creating a hair density and growth direction that is natural in appearance, providing for a more aesthetic and manageable restoration. Overall, the same principles apply as when approaching a patient with androgenic alopecia.
More continues to be learned about optimal techniques as well as their potential application and limitations. Grafting into scar tissue and grafted skin does have some unique obstacles: the blood supply is reduced relative to native tissue, the tissue is stiff, and the skin may not be as thick. Before considering transplantation, the scar tissue should be mature, ideally with some substance and pliability. In addition, hypertrophic or keloid scars should be treated to provide a tissue bed that is at the same level as the surrounding skin prior to transplantation.
When approaching vascularly impaired skin, it is best to err on the cautious side when creating a surgical plan, due to the concern that grafting into a scarred recipient bed may produce a lower survival rate of donor hair. Several investigators have found that because of their small size and low metabolic requirements, hair grafts grow well in scars even in very large areas of burns and thin skin ; however, care should be taken to minimize further compromising blood supply. Special techniques include limiting the use of epinephrine in the recipient bed as well as leaving the grafts “chubby,” with ample subcutaneous tissue surrounding the germinative center of the hair follicle. When grafting into very thin skin and skin grafts, placement of the grafts will need to be at an acute angle in the general direction of natural hair growth, as the tissue bed is very shallow. The use of tumescence and/or fat grafting before the placement of grafts has been used by some surgeons who have anecdotally noted that these techniques may assist in proper placement and optimal growth of grafts in this attenuated tissue. In has been shown that fat grafting improves the clinical appearance of burn scars, with new collagen deposition as well as an increase in vascularity seen on histologic examination. This finding may support the clinical observation of improved hair growth in scar tissue that has previously been fat grafted. Barrera (personal observation) has also noted an improved clinical appearance of the scar, including texture, thickness, and pliability, after transplanting hair grafts directly into scar tissue, an improvement that may be a result of stem cells present in the follicular units. The contribution of stem cells to the field of hair restoration is an active area of research.
Other well-described methods may improve the vascularity of the recipient bed. If the defect location allows, the transposition of a temporalis fascia flap to the site of a thin skin graft will increase the vascularity of the recipient bed, likely improving graft survival of the subsequent hair transplant surgery. Follicular unit grafting has also been used to help camouflage free-flap reconstructions in the lower face of a male. Survival of follicular unit grafts transplanted into free flaps approximates the rate achievable in native scalp.
It was previously discussed that in normal scalp, dense packing can compromise blood supply to the grafts. This aspect should be strongly considered when approaching a scarred tissue bed. Grafts placed using a density of 20 to 30 grafts per cm 2 is reasonable. The use of a higher density for small scars and a lower density for larger scars is recommended. When grafting at lower densities, a second or third stage will likely be required to obtain ideal cosmetic density. Some surgeons (presentation by Dr Robert Jones at ISHRS meeting, October 2010) will use higher densities when approaching even larger cases, but recommend testing a small area to assess graft survival before proceeding with the entire restoration. When approaching extensive areas of alopecia, it may be wise to consider staging the reconstruction by grafting the most peripheral areas with the best blood supply first and grafting the centermost regions at a second stage. One to 3 sessions over the course of 6 to 18 months will be required to achieve optimal aesthetic results. Alternative techniques including scalp expansion should also be considered in these cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






