This article describes the physiology of wound healing, discusses considerations and techniques for dermabrasion, and presents case studies and figures for a series of patients who underwent dermabrasion after surgeries for facial trauma.
Dermabrasion is a well-established method of skin resurfacing, used for both facial rejuvenation and scar revision. The earliest known use of dermabrasion dates back to Egypt, 1500 BC, when sandpaper was used to revise scars. Many forms of skin resurfacing are available, including chemical peels, laser resurfacing, and mechanical resurfacing, known as dermabrasion . Dermabrasion results in the removal of the epidermis along with partial removal of the dermis. Dermabrasion devices consist of a powered hand piece and either a wire brush or diamond fraise. Although not viewed as “high tech” or glamorous, dermabrasion continues to be a popular adjunct to scar revision, with many benefits over other resurfacing options. As with any procedure, technical proficiency, experience, and understanding of its applications and limitations are paramount.
Physiology of wound healing
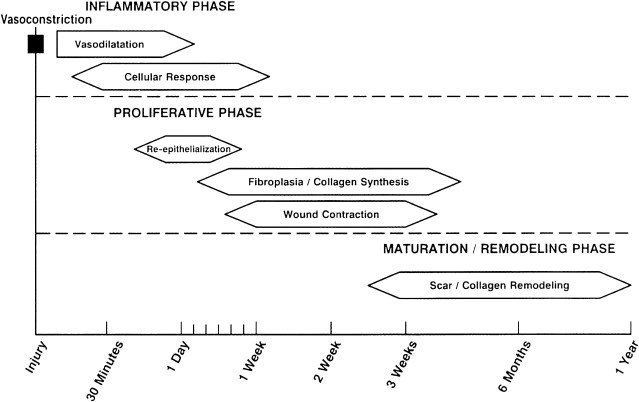
Understanding the physiology of wound healing is important when considering any skin resurfacing procedure. Wound healing occurs in progressive phases: the inflammatory phase, the proliferative phase, and the maturation phase; with significant overlap between the inflammatory and proliferative phases ( Fig. 1 ).
Inflammatory Phase
During the inflammatory phase, injury to endothelial cells results in exposure of subendothelial collagen, which acts as a binding surface for aggregation of platelets and results in their activation. The extrinsic and intrinsic coagulation cascades then occur, ultimately resulting in the activation of thrombin, which converts fibrinogen to fibrin. Fibrin then acts as the substrate for further platelet aggregation, migration of inflammatory cells, and plasma proteins. The inflammatory phase initially involves a period of vasoconstriction, mediated by epinephrine, norepinephrine, prostaglandins, serotonin, and thromboxane. This stage is followed by vasodilation, which is activated by histamines, prostaglandins, kinins, and leukotrienes. Macrophages function in phagocytosis and also release chemotactic and growth factors, including transforming growth factor (TGF)-β, basic fibroblast growth factor, epidermal growth factor, TGF-α, and platelet-derived growth factor, which is critical in endothelial cell and fibroblast proliferation.
Proliferative Phase
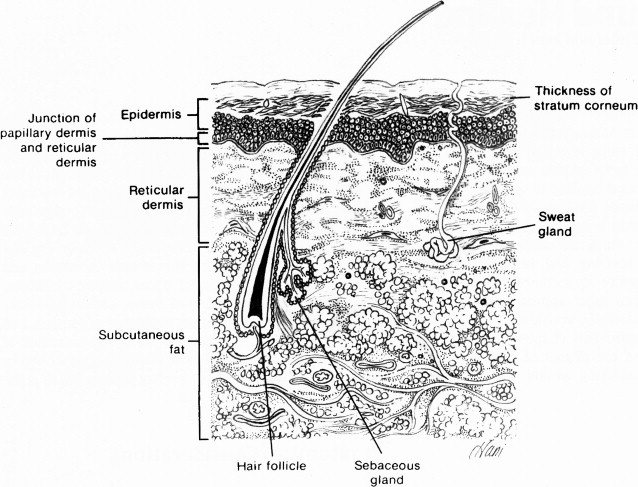
The proliferative phase begins within 24 hours of injury and has significant overlap with the inflammatory phase. Epithelial regeneration, fibroplasia, collagen formation, wound contraction, and neovascularization all occur during the proliferative phase. Epithelial regeneration begins within 24 hours of injury and is at its peak between 48 and 72 hours. Reepithelialization occurs as a result of the migration of epithelial cells from the wound margins and from within adnexal structures of the skin, which include sweat glands, hair follicles, and sebaceous glands. Basal stem cells within the adnexae undergo differentiation and subsequent migration, which is why it is paramount to dermabrade only down as far as the superficial reticular dermis, otherwise epithelialization will be impaired and scarring may result ( Fig. 2 ). Apposition of advancing epithelial cells results in inhibition of further migration, and in stratification and differentiation.
Fibroplasia, which is the growth of fibroblasts within the wound, occurs 48 to 72 hours after injury and is associated with a significant increase in collagen synthesis, which is most prominent 4 days after injury. In addition to collagen, fibroblasts also secrete elastin, fibronectin, glycosaminoglycans, and collagenase. Granulation tissue and neovascularization are also noted during the proliferative phase. Granulation tissue forms during the reepithelialization process, usually beginning at day 3 or 4, and continues until reepithelialization is complete. Wound contraction occurs as fibroblasts differentiate into myofibroblasts, reaching its maximum around 10 to 15 days after injury.
Maturation Phase
The maturation or remodeling phase begins approximately 3 weeks after injury. During this phase, type III collagen is replaced by type I collagen, with reorientation of collagen fibers parallel to the scar, and regression of neovascularization. Scar tensile strength is ultimately 70% to 80% of that encountered in nonwounded skin. The maturation phase can take up to 18 months after injury.
Yarborough proposed that dermabrasion created a reorientation of collagen fibers parallel to the lines of wound tension, which may account for some of the scar contour smoothing effects noted after the procedure. Harmon and colleagues performed ultrastructural evaluation of scars resulting from excision and primary closure of cutaneous malignancies in patients who underwent primary closure and those who underwent primary closure with dermabrasion. Serial punch biopsies over the course of 6 weeks showed organized unidirectional collagen fiber orientation parallel to the epidermal surface in the dermabrasion specimens, whereas the control specimens were found to have more-sparse and less-well-organized collagen fiber orientation.
Preoperative considerations
Surgeons should obtain a complete past medical history, including a current list of all medications, especially anticoagulants. Patients taking anticoagulants should discontinue these 2 weeks before dermabrasion if medically feasible. Acne scarring is a common indication for dermabrasion, and therefore it is important to ask about recent or current use of isotretinoin (13-cis-retinoic acid; Accutane). Because of concerns regarding hypertrophic scarring and keloid formation, patients taking isotretinoin should discontinue this 6 to 12 months before dermabrasion. Hydroquinone and retinoic acid may be prescribed to help prevent hyperpigmentation after dermabrasion. Hydroquinone inhibits melanocyte conversion of tyrosine to 3,4-dihydroxyphenylalanine and is typically prescribed as a 4% topical cream or gel applied twice daily. Retinoic acid (0.05% cream applied once daily) started 2 weeks before dermabrasion was shown by Mandy to result in expedited reepithelialization. Additionally, he found that no patients who resumed once-daily topical 0.05% retinoic acid within 1 week of dermabrasion experienced postoperative postinflammatory hyperpigmentation or milia compared with 28% in the control group. Prophylaxis against herpes simplex virus (HSV) outbreak should be considered in patients with a history to prevent reactivation. The authors do not typically use any preoperative medications when performing dermabrasion for a limited facial scar.
Preoperative considerations
Surgeons should obtain a complete past medical history, including a current list of all medications, especially anticoagulants. Patients taking anticoagulants should discontinue these 2 weeks before dermabrasion if medically feasible. Acne scarring is a common indication for dermabrasion, and therefore it is important to ask about recent or current use of isotretinoin (13-cis-retinoic acid; Accutane). Because of concerns regarding hypertrophic scarring and keloid formation, patients taking isotretinoin should discontinue this 6 to 12 months before dermabrasion. Hydroquinone and retinoic acid may be prescribed to help prevent hyperpigmentation after dermabrasion. Hydroquinone inhibits melanocyte conversion of tyrosine to 3,4-dihydroxyphenylalanine and is typically prescribed as a 4% topical cream or gel applied twice daily. Retinoic acid (0.05% cream applied once daily) started 2 weeks before dermabrasion was shown by Mandy to result in expedited reepithelialization. Additionally, he found that no patients who resumed once-daily topical 0.05% retinoic acid within 1 week of dermabrasion experienced postoperative postinflammatory hyperpigmentation or milia compared with 28% in the control group. Prophylaxis against herpes simplex virus (HSV) outbreak should be considered in patients with a history to prevent reactivation. The authors do not typically use any preoperative medications when performing dermabrasion for a limited facial scar.
Dermabrasion
Anesthesia
For traumatic and surgical scars, local anesthesia is preferred. The local anesthetic is injected into the dermis surrounding the scar and into the scar itself. The authors typically use a lidocaine with epinephrine solution. The injection provides tissue turgor, and the epinephrine minimizes oozing. Regional blocks may also be used, especially if a larger surface area is to be addressed.
Skin Preparation
Proper skin tumescence helps maintain a uniform depth of dermabrasion and maximizes the surgeon’s control of the dermabrader. Several methods can be used to accomplish this, including skin refrigerants, infiltration with local anesthetic, and mechanically stretching the skin surface to create skin tension. Special care must be undertaken when infiltrating with local anesthetic, because this can distort important landmarks. The skin surface may be prepared with gentian violet or the ink from a marking pen; this is especially useful when dermabrading larger surface areas. Gentian violet or ink stains the epidermis, and therefore once the epidermis has been removed the surgeon no longer sees violet stain. In treating the multiple depressed and pitted scars resulting from acne, the violet color accentuates these areas after the first pass of the dermabrader. The surgeon should avoid using gauze, because it may become tangled within the dermabrader.
Equipment
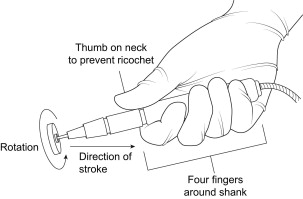
The dermabrader unit consists of the power source, hand piece, and cord ( Fig. 3 ). Dermabrader hand pieces rotate between 10,000 to 50,000 revolutions per minute and are powered pneumatically or by electric motor. Diamond fraises or wire brushes of varying sizes are used to perform dermabrasion. Alternatively, manual dermabrasion may be undertaken using a wire brush, diamond fraise, or sterilized common sandpaper. Personal protective equipment, including eye protection and facemask, are a necessity, because blood and tissue are aerosolized during the dermabrasion process.

Technique
The dermabrader may be held like a pencil or with all four fingers around the handpiece, with the thumb toward the neck. The latter method was advocated by Yarborough when using the wire brush, because it affords better control and minimizes the risk of ricochet of the device. This method is also used by the authors, although they typically use a diamond fraise. Yarborough recommends pulling the wire brush in a unidirectional fashion and perpendicular to the plane of rotation. Bradley and Park advocate that stroke direction should be 45° to the axis of the scar on the first pass, and perpendicular to the axis of initial dermabrasion on subsequent passes. Again, the direction of motion should be perpendicular to the rotation of the fraise ( Fig. 4 ). This technique maximizes control of the dermabrader and minimizes the risk of gouging. Special consideration must be given to the type of fraise used. Diamond fraises may be rotated clockwise or counterclockwise, whereas the wire brush may only be rotated clockwise. Wire brush dermabrasion creates microscopic lacerations, which are oriented at right angles to one another, creating a micro-Z-plasty effect. The diamond fraise is more forgiving and less dependent on skin turgor than the wire brush. For those with less experience, the diamond fraise is the safer option.