I. BACKGROUND
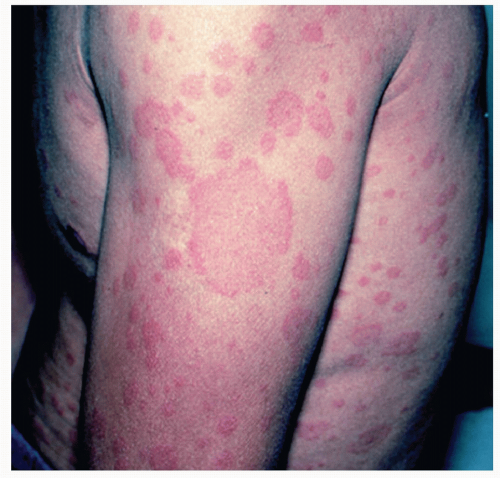
Urticaria is a heterogeneous group of conditions that are characterized by a similar skin eruption presenting as the sudden appearance of wheals, pruritus, and/or angioedema (
Fig. 44-1). It is estimated that 12% to 22% of people will experience acute urticaria at least once in their lifetime. Classification of the many types of urticaria is based on duration, frequency, and cause. In acute urticaria, wheals and/or angioedema resolve in less than 6 weeks, and most episodes are due to adverse reaction to one of the following:
Chronic urticaria, occurring in 0.5% of the general population, is characterized by episodes persisting longer than 6 weeks and is divided into two subgroups: chronic autoimmune urticaria and chronic idiopathic urticaria. A majority of cases of chronic urticaria are idiopathic. It has been associated with chronic parasitic infections (helminthes) and chronic infections in protected sites such as sinus, dental, and gallbladder infections. An association between thyroid autoimmunity and chronic urticaria has also been reported. The physical urticarias comprise a separate group of conditions in which urticaria is induced by an exogenous source.
Table 44-1 provides a summary of the types of urticaria.
Histamine derived from mast cells is the primary mediator of urticaria. Histamine release causes vasodilation and increased vessel permeability, thereby leading to erythema and edema, respectively. Histamine release from basophils may play a small role in urticaria. Mast cells may also release non-histamine mediators that promote increased vascular permeability (prostaglandin D2 and leukotriene C4) or upregulate adhesion molecules on endothelial cells leading to increased leukocyte adhesion (tumor necrosis factor-α and interleukin-4).
Cutaneous mast cells release histamine in response to many triggers. An IgE-mediated process is presumed to occur in patients with a history of atopy and in urticaria provoked by food, drugs, and aeroallergens. Mast cells can also be triggered to release histamine directly by substances such as complement 5a, morphine, and codeine. The mechanism of autoimmune urticaria is thought to be due to an IgG antibody to IgE or the IgE receptor on mast cells.
II. CLINICAL PRESENTATION
The typical lesions of urticaria are raised, erythematous, edematous, plaques of varying sizes with sharply defined serpiginous or polycyclic borders that involve the superficial portion of the dermis and may occur anywhere on the body. More edematous lesions may present with blanched centers. Individual lesions arise suddenly, typically resolve within 24 to 36 hours, and may continue to recur for an indefinite period of time. The lesions are usually extremely pruritic, but patients have also described a tingling or prickling sensation. The physical urticarias may present with a characteristic morphology and/or systemic symptoms in addition to the typical wheal and flare cutaneous reaction.