Warts
Ajay N. Amarnani
I. BACKGROUND
Warts are intraepidermal tumors of the skin and mucosa caused by infection with the human papillomavirus (HPV), a group of nonenveloped, double-stranded DNA viruses. These papillomaviruses are host specific; there are over 100 variants known to cause disease in humans. Implantation of HPV into basal keratinocytes is thought to occur primarily through mechanical disruption of the skin barrier. The virus replicates in the nucleus of the keratinocyte as it differentiates and migrates upward through the epidermis. Once the entire nuclear space is filled, virus spills into the cytoplasm; in the stratum corneum, the virus lies free within the keratin mass. HPV, a very stable virus, is shed from the superficial keratinocytes and then transmitted through hetero- or autoinoculation and even through indirect contact with contaminated articles such as swimming pool surfaces.
Although difficult to cultivate in vitro, in situ DNA hybridization, polymerase chain reaction, and molecular nucleic acid hybridization have allowed the separation and cloning of many HPV subtypes (Table 47-1). Infections by HPV subtypes show a marked preference for specific sites and are often characterized by type-specific macroscopic and microscopic features. Several HPV types are oncogenic, and there is a strong association between certain types, particularly HPV-16 and -18, and dysplasias and invasive cancers of the female lower genital tract, the penis, and the anorectal region.
HPV lesions are more common in patients receiving immunosuppressive drugs and those with immune deficiency states, including lymphoma, chronic lymphocytic leukemia, Hodgkin disease, and human immunodeficiency virus (HIV). This information, plus the increased frequency of cell-mediated responses and antibodies specific for viral antigens in patients with regression or cured warts, supports a role for immunity in the resolution of warts. Most HPV infections are latent or transient, suggesting intracellular control of viral expression; when this control is compromised, HPV-associated diseases will result. In persons with a healthy immune system, approximately 20% to 30% of all lesions will involute spontaneously within 6 months, 50% within 1 year, and 66% within 2 years. New lesions may continue to appear during this period and are seen three times more frequently in children with warts than in those without.
II. CLINICAL PRESENTATION
Clinically, warts are classified by location into three main subtypes: cutaneous, anogenital/mucosal, and epidermodysplasia verruciformis (EV). There are several morphologic variants of warts such as the following:
A. Common Warts start as small, pinhead-sized, flesh-colored, translucent papules and grow over several weeks or months to larger, raised, papillarysurfaced, flesh-colored or darker, hyperkeratotic papules. Black specks of hemosiderin pigment may be seen in thrombosed capillary loops (Fig. 47-1). Paring the lesion may result in punctate bleeding points. Common warts are found most often on the hands, especially in children, or on other sites often subjected to trauma. They may grow anywhere on the epidermis or mucous membranes and are spread by contact or autoinoculation. Common warts are most frequent between the ages of 12 and 16.
TABLE 47-1 Human Papillomavirus Subtypes | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||
B. Filiform Warts are slender, soft, thin, finger-like growths seen primarily on the face and neck.
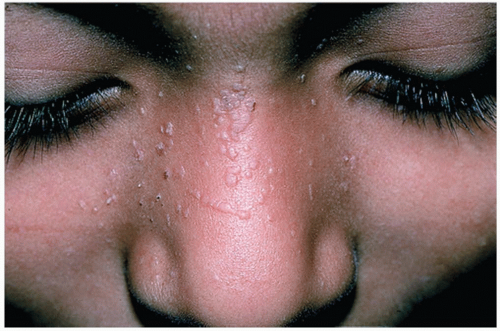
C. Flat, Plane, or Juvenile Warts are flesh-colored or tan, soft, 1- to 3-mmdiameter, discrete papules appearing primarily on the face, neck, extensor aspect of the forearms, and hands (Fig. 47-2).
D. Plantar or Palmar Warts are hyperkeratotic, firm, and elevated or flat lesions that interrupt the natural skin lines (as opposed to calluses). Red or black capillary dots may be seen. A mosaic wart (Fig. 47-3) consists of the confluence of multiple lesions into one large, usually flat lesion. As a point of contrast, corns or calluses are often more painful with direct pressure, whereas warts are more painful with lateral pressure.
E. Warts That Grow in Warm, Moist, Intertriginous Areas develop into soft, friable, vegetating clusters. These condylomata acuminata are found frequently on the foreskin and penis, particularly in uncircumcised men, on vaginal and labial mucosa, and in the urethral meatus and perianal area (Fig. 47-4).
F. EV is a chronic autosomal recessive disorder associated with chronic infection with HPV. The lesions can resemble tinea versicolor—like plaques or flat-topped papules. The lesions usually start in childhood and are often distributed on the face and extremities. During the third and fourth decades of life, one-third of patients will develop actinic keratoses and
nonmelanoma skin cancers in sun-exposed areas. Ultraviolet light is involved in the pathogenesis of EV through its immunosuppressive and mutagenic effects.
nonmelanoma skin cancers in sun-exposed areas. Ultraviolet light is involved in the pathogenesis of EV through its immunosuppressive and mutagenic effects.
III. WORKUP
The diagnosis of a wart is usually made with clinical observation. With atypical lesions, biopsy may aid in diagnosis. Smaller genital warts may be hyperpigmented (resembling seborrheic keratoses or nevi).
Application of a 5% acetic acid solution for 10 to 15 minutes will turn possible verrucae white. Two-thirds of women and one-third of men with genital warts may have accompanying genital infections that must be identified and treated.
Application of a 5% acetic acid solution for 10 to 15 minutes will turn possible verrucae white. Two-thirds of women and one-third of men with genital warts may have accompanying genital infections that must be identified and treated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree