Chapter 29 Two-Stage Reconstruction with the Modified Paneva-Holevich Technique
Outline
In 1965, Paneva-Holevich1 published a small series of flexor tendon injuries in which the proximal part of the flexor digitorum superficialis (FDS) was used as a pedicle graft for flexor digitorum profundus (FDP) tendon reconstruction. In 1969, Paneva-Holevich reported two-stage tendon reconstruction using this method in 34 digits.2 She called her new method “two-stage tenoplasty.” This surgery was later known as the “Paneva-Holevich procedure.” James Hunter,3 the pioneer of staged tendon reconstruction, first described the use of a silicone rod as a “space saver” followed by free tendon grafting for the management of patients with poor prognosis (Boyes grades 2 to 5) in 1971. The philosophy was simple: a flexible silicone-Dacron–reinforced gliding implant for the formation of a pseudo-sheath as the first stage of profundus tendon reconstruction, followed by grafting an autogenous tendon into the pseudo-sheath in the second stage. This method was used rather popularly in later years.5–9
In 1972, Kessler4 reported a combination of these techniques using the pedicle tendon transfer to replace the rod. This method was later known as “modified Paneva-Holevich method.” This combination presents several technical advantages and resolves some problems emerging from the Hunter technique.11 The graft used (FDS) is an intrasynovial donor tendon and has better morphological, functional, and healing characteristics than extrasynovial tendons.12–14 In the past two decades, we used modified Paneva-Holevich method in the patients who were indicated for staged tendon reconstruction in the digits. We found that this technique has some unique advantages. The size of the FDS is similar to the silicone rod that is used in the first stage for stimulation of pseudo-sheath formation. In addition, during the second stage we found it very easy to locate the loop between FDP and FDS that is usually situated at the level of the lumbrical muscles. There have been no donor site morbidity. This operation is associated with a lower rate of post-reconstruction tendon ruptures, because there is only one suture site at the second stage instead of two for a free tendon graft as with the Hunter technique.
Indications
The indications for the modified Paneva-Holevich are the same as for the Hunter technique. Candidates for a modified Paneva-Holevich technique must have suffered injuries of both flexor tendons to the affected digit with serious scarring and a nonfunctional flexor apparatus. More specifically, indications include (1) flexor tendon reconstruction in Boyes 2 to 5 injuries in zone 2 with considerable scarring of the tendon bed; (2) finger replantation with damage to the fibroosseous canal; and (3) failed previous flexor tendon reconstruction.11
In cases where FDS of the injured finger is intact this technique cannot be used, since a distal interphalangeal (DIP) tenodesis or arthrodesis is the treatment of choice.11 A relative contraindication is scarring in the palm that may compromise the anatomic integrity of the FDS.
This procedure greatly facilitates staged flexor tendon reconstruction in children with minor modifications in the rehabilitation program.15 Indications and contraindications of a modified Paneva-Holevich in children are the same as in adults.
Operative Technique
The surgical technique includes two stages with a minimum of a 3-month time interval.11 In both stages, the use of magnifying loupes is mandatory.
Stage 1
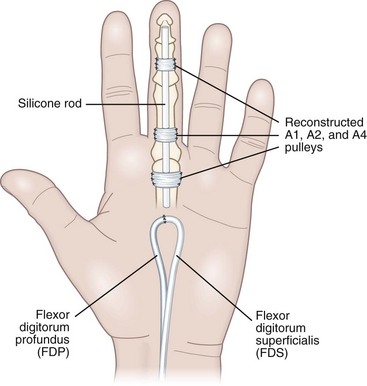
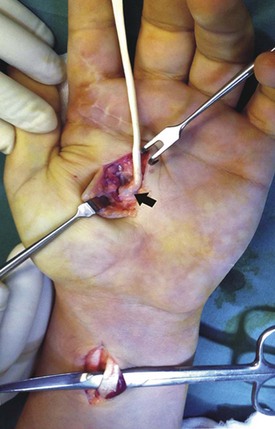
A second incision is made in the palm (inverted L) and is center near thenar for index and middle finger and near hypothenar for the ring and small finger (Figure 29-1). The FDS and FDP tendon ends of the injured finger are retrieved, freed of adhesions, and sutured together with a loop at the lumbrical level in an end-to-end fashion (Figure 29-2). A silicone rod is chosen corresponding to the diameter of the FDS tendon (usually No. 3 to 5). The implant is inserted and its distal insertion is secured with direct sutures to the profundus stump and is reinforced with pull-out suture to the distal phalanx. The proximal part of the silicone rod is cut to the lumbrical level and is left free underneath the FDS-FDP loop after checking its free motion.

Figure 29-1 A Bruner incision in the digit and an L incision in the palm for the FDS-FDP loop junction.
We usually reconstruct at least A1, A2, and A4 pulleys using pieces of the removed tendons (see Figure 29-2). The technique used for pulley reconstruction is suturing these pieces of flexors to the lateral sides of the fibro-osseous canal. Pulley reconstruction should follow silicone rod insertion in order to accurately match the selected implant. Any necessary secondary procedures, such as nerve repair, interphalangeal (IP) or metacarpophalangeal (MCP) joint arthrolysis, and web space plasty, are performed at this point, and the skin is closed without tension.
Stage 2
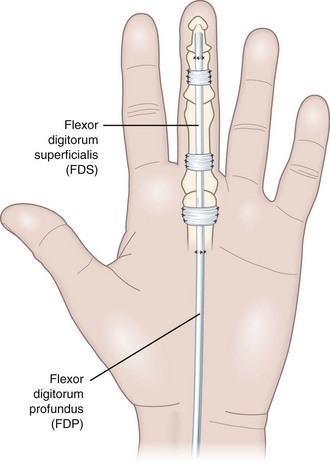
The stage 2 surgery is done after an interval of 3 months and consists of three steps: (1) a mid-palmar inverted L incision for loop retrieval; (2) an antebrachial incision for transsection of the FDS at the musculotendinous junction; and (3) an angular incision over the DIP joint for graft retraction and anchoring the graft (FDS) to the distal phalanx (Figures 29-3 to 29-5).
A longitudinal antebrachial incision is used to identify the FDS tendon to the same finger. The tendon is cut at the musculotendinous junction after a measurement is done for the needed length. The cut FDS is then pulled out to the palmar incision through the carpal tunnel (see Figure 29-5). The FDS stump is sutured to the proximal end of the silicone rod.
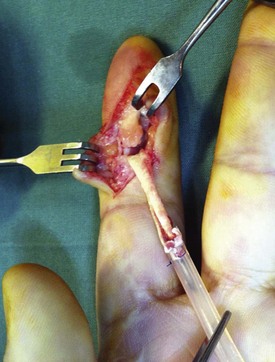
A third angular incision is made over the DIP joint and the silicone rod with the graft sutured to its end is gently retracted through the pseudo-sheath (Figure 29-6). The silicone rod is then discharged and the tension of the graft is estimated by temporary stabilization with a hypodermic needle through the skin of the distal phalanx. The desired tension is adjusted so that the reconstructed finger is kept in slightly more flexion than the adjacent fingers in flexion and extension of the wrist. Then, the graft is secured to the profundus stump in the distal phalanx with three or four interrupted 3-0 nonabsorbable sutures. To avoid nail deformities, pull-out sutures should exit proximal to the nail matrix on the dorsum of the phalanx. In the recent years, we used a small anchor inserted in the palmar aspect of the distal phalanx, securing the distal part of the graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree