Chapter 36 Treatment of Boutonnière and Swan-Neck Deformities
Outline
Post-Traumatic Deformity
Post-Traumatic Boutonnière Deformity
Post-traumatic boutonnière (or “buttonhole”) deformities, characterized by hyperextension of the metacarpophalangeal (MCP) joint, flexion of the proximal interphalangeal (PIP) joint, and hyperextension of the distal interphalangeal (DIP) joint, are caused by disruption of the central slip. Attenuation of the triangular ligament allows the lateral bands to migrate volar to the PIP joint axis of rotation, transforming the lateral bands into a flexion force at the PIP joint and extension force at the DIP joint (Figure 36-1).
Physical examination findings supportive of an acute central slip injury include: (1) A 15° to 20° extension lag at the PIP joint with the wrist and MCP joint held in full flexion.1 (2) Absence or weakness of resisted active extension of the PIP joint with the PIP joint starting in 90° of flexion.2,3 (3) Elson test: The patient attempts to extend actively the PIP joint of the involved finger against resistance from a 90° starting position over the edge of a table. The absence of extension force at the PIP joint accompanied by fixed extension of the DIP joint confirm disruption of the central slip as extension forces are being transferred to the DIP joint by the lateral bands.4,5 (4) Boyes test: A positive test may be found in progressive stages of boutonnière deformity but is not reliable for the diagnosis of acute central slip injuries.5 Loss of active flexion of the DIP joint with the PIP joint held in passive extension due to tension across the lateral bands following disruption of the central slip. Active flexion of the DIP is possible with the PIP joint flexed.
After a traumatic injury to the central slip, the boutonnière deformity generally progresses through five stages6:
1 Disruption of the central slip results in resting flexion of the PIP joint and weak extension of the middle phalanx via the lateral bands
2 Absent active PIP joint extension combined with attenuation of the triangular ligament and contracture of the transverse retinacular ligaments results in the volar migration of the lateral bands
3 Extension forces are transmitted through the lateral bands, causing hyperextension at the DIP joint
4 Progressive contracture of the PIP joint volar plate and the oblique retinacular ligament causes fixed flexion contracture at the PIP joint
5 Progressive articular degeneration occurs after prolonged and untreated pathology
Post-Traumatic Swan-Neck Deformity
The post-traumatic swan-neck deformity may progress through four characteristic stages7:
1 Full passive PIP joint range of motion
2 Intrinsic tightness secondary to prolonged hyperextension of the PIP joint
3 Fixed hyperextension of the PIP joint regardless of MCP position due to attenuation and contraction of the transverse retinacular ligament and dorsal subluxation of the lateral bands
4 Articular degeneration and fixed hyperextension deformity of the PIP joint
Rheumatoid Deformity
Rheumatoid Boutonnière Deformity of the Fingers
Rheumatoid boutonnière deformities occur due to progressive erosion of the central slip, transverse retinacular ligaments, and the triangular ligament by the destructive synovitis characteristic of rheumatoid arthritis. As the restraints provided by triangular ligament are lost, the lateral bands migrate in a volar direction, transforming them into a flexion force at the PIP joint. The continued flexion deformity of the PIP joint results in contractures of the oblique retinacular ligament, the volar plate, and the collateral ligaments; progression from a flexible to a fixed deformity of the PIP joint occurs with time. The classic boutonnière deformity involves flexion of the PIP joint and hyperextension of the DIP and MCP joints and evolves through three stages.8 Stage I is considered a mild, involving PIP joint synovitis and a passively correctable flexion deformity of the PIP joint. Stage II, or a moderate deformity, involves a flexion contracture of the PIP joint and concomitant MCP joint hyperextension. Stage III involves a fixed contracture of the PIP joint and destruction of the articular surfaces.
Rheumatoid Swan-Neck Deformity of the Fingers
Swan-neck deformities associated with rheumatoid disease are characterized by hyperextension of the PIP joint and concurrent MCP and DIP flexion deformities. A swan-neck deformity may be caused by primary pathology affecting the MCP, the PIP, or the DIP joint.7
 MCP joint pathology: The characteristic rheumatoid digital deformity of flexion and ulnar drift leads to imbalance of the extensor mechanism. The PIP is hyperextended by the extension force exerted across the PIP by the dorsal shift of the lateral bands. The MCP joint component of a swan neck deformity is flexion, which can be secondary to chronic synovitis with degeneration of the sagittal bands, intrinsic tightness, and/or articular destruction resulting in volar subluxation of the MCP joint.
MCP joint pathology: The characteristic rheumatoid digital deformity of flexion and ulnar drift leads to imbalance of the extensor mechanism. The PIP is hyperextended by the extension force exerted across the PIP by the dorsal shift of the lateral bands. The MCP joint component of a swan neck deformity is flexion, which can be secondary to chronic synovitis with degeneration of the sagittal bands, intrinsic tightness, and/or articular destruction resulting in volar subluxation of the MCP joint.
 PIP joint pathology: The volar plate of the PIP joint, the collateral ligaments, and the insertion of the flexor digitorum superficialis (FDS) tendon can become attenuated in rheumatoid disease, resulting in PIP hyperextension. Also, progressive attenuation of the transverse retinacular ligaments results in a loss of the normal restraints to the dorsal migration of the lateral bands, leading to PIP joint hyperextension.
PIP joint pathology: The volar plate of the PIP joint, the collateral ligaments, and the insertion of the flexor digitorum superficialis (FDS) tendon can become attenuated in rheumatoid disease, resulting in PIP hyperextension. Also, progressive attenuation of the transverse retinacular ligaments results in a loss of the normal restraints to the dorsal migration of the lateral bands, leading to PIP joint hyperextension.
 DIP joint pathology: Synovitis of the DIP joint may cause attenuation and eventual rupture of the terminal extensor tendon. Subsequently, the extensor forces are concentrated at the PIP joint, resulting in a hyperextension deformity of the PIP joint.
DIP joint pathology: Synovitis of the DIP joint may cause attenuation and eventual rupture of the terminal extensor tendon. Subsequently, the extensor forces are concentrated at the PIP joint, resulting in a hyperextension deformity of the PIP joint.
Nalebuff classified rheumatoid swan-neck deformities into four distinct types7:
 Type I—Fully mobile and flexible PIP joint, regardless of MCP joint position
Type I—Fully mobile and flexible PIP joint, regardless of MCP joint position
 Type II—Active and passive PIP joint motion is limited with MCP joint held in extension due to intrinsic tightness
Type II—Active and passive PIP joint motion is limited with MCP joint held in extension due to intrinsic tightness
 Type III—Decreased PIP joint motion in all positions of MCP joint flexion and extension
Type III—Decreased PIP joint motion in all positions of MCP joint flexion and extension
 Type IV—Fixed extension contracture of the PIP joint with degeneration of PIP joint articular cartilage
Type IV—Fixed extension contracture of the PIP joint with degeneration of PIP joint articular cartilage
Rheumatoid Thumb Deformity
Thumb deformity associated with rheumatoid disease may be classified based on changes specific to the carpometacarpal (CMC), MCP, and interphalangeal (IP) joints, as outlined by a modified classification system of six types initially proposed by Nalebuff.9,10
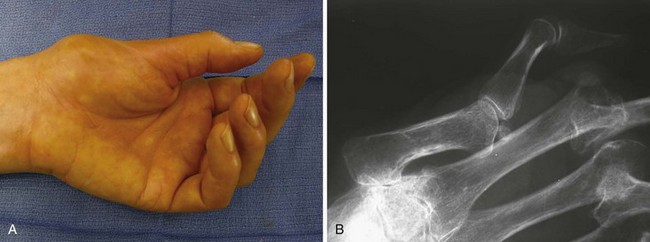
The second most common rheumatoid thumb deformity is the type III (swan-neck) deformity (Figure 36-2).9,11 CMC joint synovitis leads to erosion of the articular surface and capsular attenuation, which contributes to the dorsal and radial subluxation of the CMC joint. An adduction contracture of the metacarpal develops due to the alteration in forces across the CMC joint with daily activities such as pinch and grasp. Compensatory MCP joint hyperextension and IP joint flexion, characteristic of a type III swan-neck deformity, is potentiated as functional compensation for the progressive adduction contracture.12
Methods of Treatment
Post-Traumatic Boutonnière Deformity
Operative Management
Surgical intervention should be considered for patients who have failed 3 months of conservative treatment, such as extension splinting, and for open injuries or patients with fixed deformity and associated degenerative joint changes. Full passive extension of the PIP joint should be sought prior to surgical reconstruction. Burton and Melchior emphasized that boutonnière reconstructions are generally more successful in patients with flexible joints and that a first-stage joint contracture release, followed by an exercise and splinting program, can sometimes obviate the need for further procedures.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree