Chapter 35 Soft Tissue Coverage for Extensor Tendon Reconstruction
Outline
Wound Débridement
Choice of extensor tendon coverage, working from distal to proximal, will be based on the level of injury as well as the availability of nontraumatized soft tissue in the proximity of the wound. Clearly, replacing like with like is the ideal condition. All defects that are replaced with local tissue of similar color, texture, pliability, and sensation will provide a better outcome than non loco-regional flaps. The resulting defect, following radical débridement, will also be much larger than the initial wound size. Knowing that stable soft tissue coverage can be provided regardless of defect size should be impetus for providing aggressive initial débridement. This not only serves to expedite reconstruction but also helps minimize any risk of infection due to the presence of residual necrotic tissue (Figure 35-1).
Soft Tissue Coverage and Reconstruction
Reverse Cross-Finger Flap
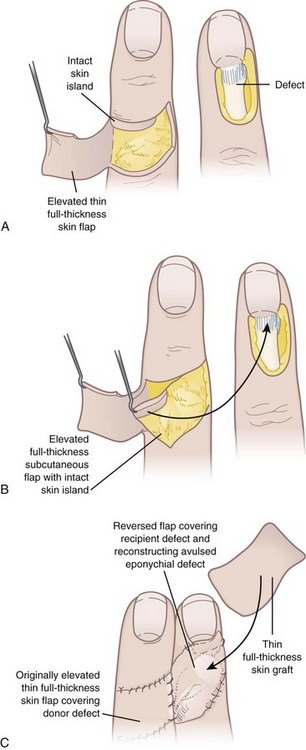
Extensor tendon exposure in zones 1 through 4 can be covered with reverse cross-finger flaps. The reverse cross-finger flap, first described by Pakiam in 1978, is an excellent local flap for soft tissue coverage of exposed extensor tendons in the dorsal digit. Its vascular supply is provided by the dorsal digital branches of the digital arteries, as well as small subcutaneous veins and venae comitantes from the dorsal digital branches. Subcutaneous veins from the cross-finger flap can also be used as venous flow through veins for replants to bridge both recipient and donor veins. The reverse cross-finger flap is then covered with either a split- or full-thickness skin graft for definitive coverage. The flap is elevated as follows: The adjacent donor digit is used for a cross-finger flap. The mid-axial skin incision is made proximal to the defect, and the skin flap is elevated just above the subcutaneous tissue in a direction that is opposite the side of the defect. The adipofascial flap is then harvested down through paratenon in the opposite direction of the elevation of the overlying skin flap. This is taken from mid-axial line to mid-axial line. Care is taken to not damage any of the dorsal branches of the digital artery when harvesting this flap. The flap is then turned over to cover the adjacent digit dorsal defect and provide good coverage for the exposed extensor tendon. The cross-finger adipofascial flap is covered with a split-thickness skin graft and the donor site is closed primarily with its hinged skin flap. The hand is immobilized for 2 to 3 weeks, preferably 3 weeks, and the division and inset of the flap is performed after 2 to 3 weeks, with revisions to the donor or recipient site as needed. The patient is splinted in a position of function for 3 weeks to minimize any contractures. In compliant patients, the patient can begin light active range of motion after the surgery but needs to be very compliant (Figure 35-2).
First Dorsal Metacarpal Artery Flap
The first dorsal metacarpal artery flap (FDMA flap, i.e., kite flap), described by Foucher and Braun,1 provides two major applications in hand reconstruction: (1) dorsal hand wound coverage and (2) thumb reconstruction.
In Foucher’s anatomical study of 30 injected cadaveric hands, the FDMA originated from the radial artery in 28 of 30 specimens and from the dorsalis superficialis antebrachialis artery in 2 of 30 cases. From there, it courses distal to the extensor pollicis longus tendon, and proximal to the radial artery’s entry between both heads of the first dorsal interosseous (DIO) muscle. The FDMA travels parallel to the dorsal surface of the second metacarpal, and superficial to the first DIO muscle fascia, with some fibers occasionally covering the vessel. The FDMA then continues distally and anastomoses at the level of the metacarpal neck with dorsal perforating branches from the palmar metacarpal arteries of the deep palmar arch. These perforator branches form the basis of the reverse flow FDMA island flap. They anastomose with three different arterial systems: (1) distally with the dorsal branches of the proper palmar digital arteries, (2) proximally with branches of the DMA, and (3) laterally with adjacent DMA perforating branches (Figure 35-3).