Chapter 34 Transverse medial thigh lift
Introduction
The medial upper thigh area is often subject to ptosis and skin wrinkling, due to the thinness of the skin and the frequent fat deposition. The unsightly appearance of this region results in a number of patients, some as young as 35 years, seeking consultation and correction. Unfortunately, the transverse, superior and medial thigh lifts still have a poor reputation among plastic surgeons and patients alike due to the high complication rate and unsightly esthetic results. Complications previously encountered with traditional procedures included scar visibility at the upper aspect of the thigh, vulvar dehiscence, hypertrophic scarring mainly in the gluteal groove, wound dehiscence, infection, skin necrosis, and lymphocele.1
A well-conducted operation should aim at avoiding any lymphatic, venous or arterial vessel impairment as well as any skin trauma, and result in limited or no skin tension. These goals are possible, and have been advocated and clearly demonstrated for many years.2–5
Preoperative Preparation
Good communication and avoidance of unreasonable expectations is essential, especially in those patients with large thighs.6 We classify our patients into four types:
Type I: The patient presents with isolated fat excess of the upper inner thigh. This should respond well to liposuction alone.
Type II: The patient shows a limited skin laxity.
Type III: The patient shows important skin laxity or excess, but limited to the upper third of the inner thigh. Type II and type III will require skin resection in a vertical manner, for a proper “lift” of the inner thigh.
Type IV: The patient has a skin laxity extending to the lower part of the inner thigh. Type IV patients will require additional skin resection, to tighten the thigh transversally, with a vertical scar extending gradually down to the knee according to the importance of the necessary resection.
Anatomical Considerations
Fat Layers
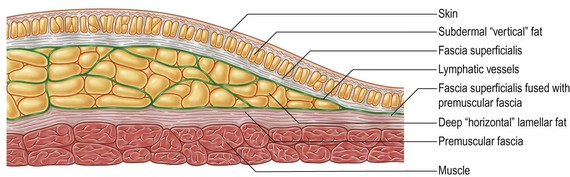
Fat distribution under the human skin is uneven (Fig. 34.1). There is an almost uniform superficial layer, where lobules are organized in a “vertical” manner, perpendicular to the skin surface. In these areas, the fascia superficialis is fused with the deep, premuscular fascia. In some areas, there is another layer, deep to the fascia superficialis, where the fat is organized in a “horizontal”, lamellar fashion, parallel to the skin surface. Liposuction allows for the elimination of most of the fat in the different layers, achieving not only volume reduction but also skin release. Skin retraction is best in those areas of deep fat, as retraction of the superficial, “vertical” fat layer often leads to surface irregularities.
Lymphatic Distribution
The lymphatic vessels of the skin (Fig. 34.1), after collecting from the surface, join into vessels situated just deep to the fascia superficialis. Therefore, in areas where there is deep fat, it is of the utmost importance that dissection stays superficial, in order to avoid any impairment of the lymphatic drainage. In some anatomical areas this boundary is not particularly obvious, for example in the outer thigh. Nevertheless, due to the frequently described lymphatic complications,7 dissection should stay superficial.
Skin Particularities
The skin of the upper inner thigh is very thin. Its blood supply will not tolerate excessive tension, which will subsequently lead to wound dehiscence or necrosis. Deep anchorage will prevent not only excessive tension on the suture line, but also secondary deformity, such as scar migration or vulvar dehiscence.8
Surgical Technique
Preparation and Positioning
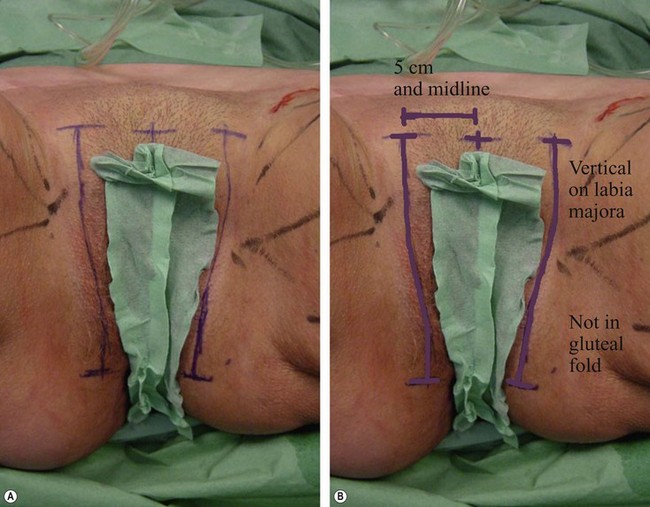
The incision line should avoid the inguinal crease, where there is a major risk of impairment of the lymphatics.2,9–11 Our incision is vertical within the pubis, starting from below the hairline, medial to the groin crease, 3 to 4 cm away from the midline on either side. Another reason for a pubic positioning is that superficial dissection in the groin region to preserve lymphatic vessels will result in a very thin skin flap, which will not tolerate any tension. The incision is then extended vertically toward the pubic tubercle along the labia majora. If the amount of skin resection is major, it seems preferable, as advocated by Le Louarn,11 to extend the marking of the incision to the inner part of the buttock toward the ischial tuberosity and the anal margin. This is a superior incision line as opposed to the gluteal fold, as this area is very prone to hypertrophic and painful scarring and is technically difficult to correct.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree