Chapter 13 Breast reshaping after massive weight loss
Autologous tissue techniques
• Breast reshaping after massive weight loss can be achieved by applying concepts of parenchymal reshaping and redistribution of autologous lateral chest wall tissue into the breast mound.
• Careful assessment of parenchymal volume, amount of redundant skin envelope, and extent of lateral skin/fat roll is necessary for planning the procedure. Importantly, medial displacement of the nipples is a common finding in the massive weight loss patient.
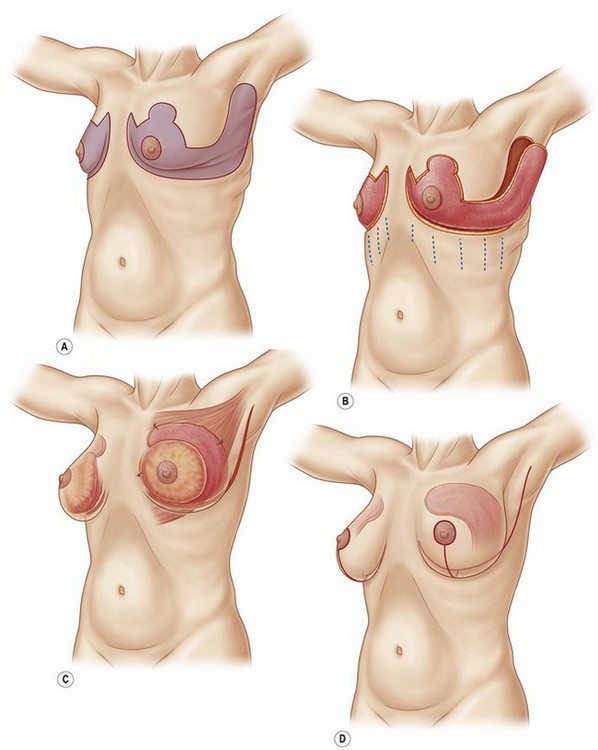
• The spiral flap procedure uses adjoining lateral thoracic and epigastric flaps. The de-epithelialized lateral thoracic flap, supplied by intercostal trans-serratus perforators, takes a spiral course to augment the superior pole of the breast over the pectoralis major muscle and is suture suspended to the third costal cartilage. The de-epithelialized epigastric flap is supplied by descending branches from the sixth intercostal and flips up to augment the inferior pole of the breast and is suture suspended to the fifth costal cartilage.
• The dermal suspension mastopexy involves de-epithelialization of an extended Wise pattern with elevation of medial and lateral fasciocutaneous flaps, auto-augmentation using the lateral flap, suspension of flaps to rib periosteum, and parenchymal reshaping by plication of the broad dermal surface.
![]() For additional online content visit http://www.expertconsult.com
For additional online content visit http://www.expertconsult.com
Introduction
Typically, the breasts flatten, sag and descend on the chest. Superior pole fullness is almost nonexistent. The breasts are displaced and broadened by descended inframammary folds (IMF). The IMF descent progressively increases from medial to lateral. The nipple–areola complexes (NACs) are ptotic and usually distorted and medially displaced. Surrounding the breasts are rolls of mid torso skin shaped by transverse subcutaneous fascial adherences to underlying muscular fascia. This manifests as characteristic lateral rolls that obliterate the lateral curvature of the breast and blend the breast seamlessly with the upper torso.1
The strategy for correcting the breast deformity in the MWL patient considers the degree of NAC ptosis, current and desired breast volume and shape, skin quality and quantity, descent of the IMF, neighboring skin deformity, extent of available tissue excess for breast augmentation and suspension, and prior breast surgery. In many MWL patients, the breasts descend 1–4 cm on the chest. As the IMFs approach the costal margins, women admit that they have to uncomfortably pull up their brassieres to raise their breasts. The surface of the posterior aspect of the breast on the chest wall has been called a footprint, which is the “foundation for the overlying three-dimensional structure of the breast”.2 Blondeel et al further subdivide the pertinent breast esthetics into breast conus, skin envelope quality and quantity.2 “The breast conus refers to the three-dimensional shape, projection, and volume of the tissue (or implant) on top and anterior to the footprint of the breast”.2 The determinate issues are volume, shape (breast conus), the breast footprint, the severity of the deformity, the need and acceptance of extensive incisions to correct the breast, and the availability of neighboring tissue for augmentation and suspension. The major goals are central projection and superior fullness, appropriate nipple positioning, and three-dimensional shaping that restores the lateral curvature of the breast.
In the spiral flap technique, excess skin and fat of the epigastrium and lateral thorax are de-epithelialized in continuity with the central breast mound and appropriately positioned, then tailored and buried under Wise pattern flaps.3 The inevitable twisting and turning of this compound flap led to the name “spiral flap”.4 The epigastric flap is an inferior extension of the central breast pedicle nourished through descending intercostal perforating vessels. The lateral chest flap is a tongue-like lateral fasciocutaneous extension of the central pedicle, similar to the lateral thoracic flap described by Holstrom in 1987 with confirmed utility and safety.5–8 It is a fasciocutaneous flap based on perforators through the serratus muscle. Borud based his breast reshaping after MWL on this flap, which he referred to as the intercostal arterial perforator (ICAP) flap.9 Closure of the donor site removes the lateral chest and back roll, usually leaving a tight transverse closure along the bra line.
The dermal suspension mastopexy10–13 employs a well vascularized central dermoglandular pedicle.14,15 A modification of the traditional Wise pattern allows for the precise control of the skin envelope and nipple position16 with an extended lateral wing of the Wise pattern used to both eliminate the lateral roll and convert the redundant tissue to a fasciocutaneous flap that is transposed into the breast mound. The dermal suspension techniques of Qiao, Frey, Cerqueira and others lay the historical foundation for the use of parenchymal suspension and extensive sculpting via dermal plication and fixation to the chest wall.17–22 Holmstrom’s lateral thoracodorsal transposition flap, as mentioned above, is the basis for auto-augmentation with adjacent chest wall tissues.5 Medial fullness is achieved via the elevation and manipulation of a medial breast flap. Great control over both skin envelope and parenchymal shape may be gained with this procedure.
Preoperative Preparation
Autogenous breast reshaping is offered to MWL women who desire body contouring. They are eligible as soon as 1 year after their bypass surgery, if their weight loss has been stable for 4 months, and if there is no expectation for further weight loss. A thorough review of their medical history, with emphasis on the evolution of obesity-related comorbidities is important. The patient must be under optimal management of their remaining medical diseases with no acute issues.23 Their nutritional status is evaluated and specific mineral, vitamin and protein deficiencies corrected.24,25 Most patients are also started on high protein supplements with a goal of 75–100 g of protein per day. Patients with BMI between 25 kg/m2 and 30 kg/m2 are the best candidates. Moderately obese patients with BMIs between 30 kg/m2 and 35 kg/m2 are advised to attempt further weight loss before surgery and may be at greater risk for wound healing complications.26 Patients with severe obesity must lose weight before they are candidates for complex body contouring procedures. All MWL patients should be counseled on expected results and expectations balanced. Patients who have obviously unrealistic goals should be deferred.
Surgical Procedure
Spiral Flap of Hurwitz with Upper Body Lift
Wise pattern mastopexy with spiral flap augmentation integrates breast reshaping with UBL.3,4 Fundamental to an UBL is removal of the mid torso skin rolls and improved contour. If appropriate, the secondary component of the UBL is superior repositioning of the breast footprint and IMF.
With the patient standing, the excess skin of the upper abdomen is vigorously pushed superolateral. When all excess skin is gathered – the abdominal skin is tight and the umbilicus is pulled slightly cephalad – a mark is made where the gathered abdominal skin meets the new IMF position along the nipple line. With the tissues still suspended, the new parasternal and anterior axillary line attachments of the breasts are sighted and marked. The gathered tissues are dropped. The curvilinear incision line that serves both the reverse abdominoplasty and the new IMF is then drawn. This line starts at the marked parasternal breast attachment and descends to the upper abdominal marked nipple line point and then ascends to the marked point at the anterior axillary line. This line is similar to the IMF incision line of the Wise pattern, except that it includes all the redundant abdominal skin with the central breast pedicle. Obviously the reverse abdominoplasty, which removes excess skin of the epigastrium which was not corrected by prior abdominoplasty, can be performed without changing the location of the IMF. The IMFs are the upper line of excision of excess skin. The inferiorly based abdominal flaps are discontinually undermined to the costal margins. The closure ends along the newly designated IMFs, and unless there is symmastia, it does not cross the sternum. Occasionally, too much upper midline skin excess remains and then an inverted “V” of skin is excised over the xiphoid. The discontinuously undermined reverse abdominoplasty flap will be advanced and suture secured along the sixth rib (Fig. 13.1).
In patients with less than severe back skin laxity or who refuse a mid back scar, the long posterior flap extension of the Wise pattern has been, over the past 5 years, turned superior along the mid lateral chest to end at the axilla. Often this excision is continued into an L-brachioplasty. To capture mid lateral back rolls, the flap curves inferiorly, forming a “J” shape. The entire operation can be performed in the supine position. After harvest of this mid lateral chest flap for breast augmentation, the J cut out back flap is suture advanced to the anterior serratus muscular fascia. The lateral breast is thereby bordered by tight chest wall conforming skin.27
The vascularity of the lateral thoracic flap is confirmed and then the inferior breast with its superiorly based epigastric extension is elevated from its descended location near the eighth rib to the sixth. Despite descended NACs, this interruption of the inferior border of the breast has had no NAC vascular compromise. That is because our breast mobilization, Wise pattern thin skin flap elevation, and positioning of the spiral flaps have not interrupted the critical transverse blood supply to the breast along the fourth and fifth intercostal septum of the breast.13 We and others have anatomically and clinically confirmed Wuringer’s anatomical vision, making the distance of NAC elevation during mastopexy essentially irrelevant as long as the mid glandular septum is preserved.14
Usually, an L brachioplasty is performed concurrently.28 The short descending limb excision of the L may extend to the bra line closure. The full width of lateral chest excision awaits the breast closure, because the lateral chest laxity is taken in by the autogenous enlargement of the breast. Clinical examples are shown in Figs 13.2, 13.3, 13.4, 13.5, 13.6, 13.7, 13.8, 13.9, 13.10, 13.11 and 13.12.
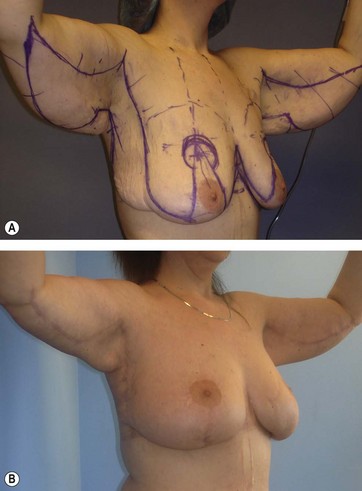
(A) Patient is 39 years old, BMI of 28.7, who lost 63 kg (139 pounds) 6 years after Roux-en-Y bypass. She had a previous abdominoplasty. As this and subsequent views (Figs 13.3–13.5) show, there is grade 3 ptosis with deflated and flat breasts, having no fill of the superior poles. Most of her back roll is immediately lateral to her breasts and will be incorporated into the J thoracoplasty for augmentation and suspension of the superior pole as indicated in the preoperative drawings on her body. The Wise pattern has 10 cm long vertical limbs to accommodate the anticipated flap augmentation. The brachioplasty markings are freehand drawn hemi ellipses along the bicipital groove, which then have measured equal distances confirmed from the elbow to the deltopectoral groove and the elbow to the end of the advancement point along the posterior border. (B) One year later, the entire breasts are higher on the chest, greatly augmented and better shaped. The raised IMFs and back skin are advanced superiorly and laterally to firmly frame the soft and well-projecting breasts. The arms were significantly reduced in volume and sag with a natural curved posterior border. The curving medial scar ascends through the minimally concaved axilla and takes a right angle turn below the deltopectoral groove to descend between the lateral breast and chest wall.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree