Chapter 26 Fleur-de-lis abdominoplasty including mons contouring
• Fleur-de-lis abdominoplasty addresses the vertical skin excess normally addressed with classic abdominoplasty and also the transverse skin excess by adding a vertical excisional component.
• The most common area of wound healing problems is at the junction of vertical and horizontal excisions, thus the vertical resection should be tapered at each end to minimize transverse tension.
• The vertical resection provides circumferential skin tightening, and can be modified based on existing scars.
• Preoperative markings must be made with the patient standing to achieve symmetry.
• The effects of weight gain in the mons area frequently remain after massive weight loss and can be addressed with liposuction or direct excision.
Preoperative Preparation
Patient Evaluation
Patients with complaints of abdominal tissue excess are evaluated for skin quality, stretch marks, subcutaneous adiposity, intertrigo, lymphedema and hanging skin. A careful evaluation of the entire abdomen, flanks, back and buttocks is carried out, noting previous surgical scars. Bimanual palpation is used to gauge redundant tissues and demonstrate to patients the degree of transverse skin tightening possible with the vertical resection (Fig. 26.1). Care is taken to diagnose hernias, particularly in patients with a history of open bariatric procedures. Repairing these hernias at the same time as body contouring is discussed with the patient, as well as the possibility of needing mesh (Fig. 26.2).

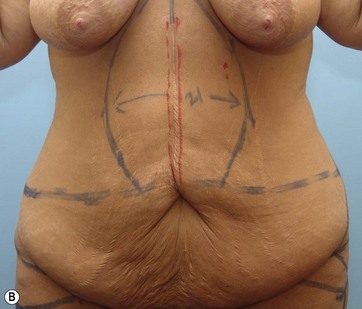
FIG. 26.2 Typical preoperative patient presenting for body contouring. The patient is marked for fleur-de-lis abdominoplasty. Note the hernia marked in red as a result of a prior open bariatric procedure. Frequently the hernia can be repaired and reinforced with midline muscle plication at the time of surgery. Postoperative results are shown in Fig. 26.10.
Preoperative Markings
The patient is asked to strongly lift their abdominal skin while in a standing position (Fig. 26.3). The low transverse marking is made at the level of the pubic symphisis, which ends up removing one third of the hair-bearing mons. This mons reduction coupled with the lift achieved during closure is typically the extent of mons contouring required. The low transverse incision is extended bilaterally to the level of the anterior superior iliac crest. The incision is measured to make sure each side is of equal length. If a body lift is planned, the markings are continued circumferentially.
The superior portion of the abdominoplasty incision is usually judged to be just above the umbilicus. The excess tissue in the transverse dimension is then marked using strong bimanual palpation (Fig. 26.1A). The planned vertical resection is elliptical, tapered at the xyphoid process superiorly and near the planned horizontal incision inferiorly (Fig. 26.1B). All markings should be double-checked intraoperatively prior to incision. Adjunctive liposuction marks are made along with existing scars and hernias. Midline scars are simply incorporated into the planned resection, but off-centered ones such as open cholecystectomy scars may require modification of the vertical resection to incorporate the previous surgical scar and bring the final planned closure off midline (Fig. 26.9).
Surgical Technique
If there is any doubt about needing the vertical component to achieve an aesthetic closure, the abdominal flap can be left intact until after rectus plication. If the decision has been made preoperatively to have a vertical scar, it is simpler to make the entire midline incision from xiphoid through the abdominal flap at this time (Fig. 26.4).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree