■ Posterior mediastinal goiters are rare, but when present, the RLN may be anteriorly displaced.
■ In rare cases, substernal goiters may not be contiguous with the cervical thyroid gland.
Approach
■ The cervical vascular supply, anterior position, and rarity of bilateral intrathoracic extension typically facilitate complete removal of substernal goiters transcervically.5
■ Less than 10% of substernal goiters require sternotomy or thoracotomy.
■ Relative indications for sternotomy include the following:
■ Prior mediastinal surgery
■ Retroesophageal/posterior mediastinal location
■ Goiter abutting the carina
■ Intrathoracic malignancy with extrathyroidal extension
■ Intimate association with the great vessels
■ Massive substernal goiters that physically cannot be removed through the neck
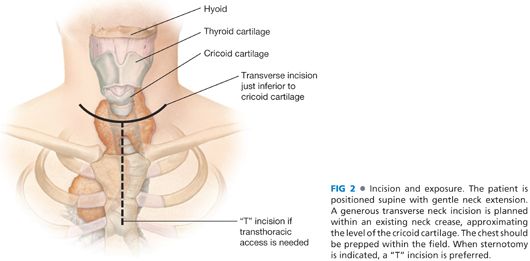
■ When sternotomy is indicated, a “T” incision is frequently preferred.
■ Transcervical dissection and ligation of vessels occur prior to opening the chest. However, in cases with venous obstruction, sternotomy precedes vessel ligation in order to limit intrathoracic venous distension.
■ The sternotomy may be partial or complete.
■ Care is necessary in order to identify and manage aberrant mediastinal vascular tributaries supplying the thyroid gland.
■ The intrathoracic trajectory of the RLNs can be identified and preserved under direct vision.
■ Lateral thoracotomy typically provides suboptimal visualization of critical structures but may be preferred in specific cases.
■ Video-assisted thoracic surgery may also be considered.
TECHNIQUES
INCISION AND EXPOSURE
■ Exposure is critical, as satisfactory access facilitates appropriate visualization. Thus, a generous transverse neck incision is planned within an existing neck crease, approximating the level of the cricoid cartilage.
■ The strap muscles are identified and divided along the midline raphe. In order to obtain sufficient access, the strap muscles are transected at least on the side of intrathoracic extension (FIG 2).
MOBILIZATION OF THYROID GLAND
■ As the thyroid is gently and bluntly freed from surrounding areolar tissue, meticulous attention is necessary to ensure extracapsular dissection in order to maintain a bloodless field.
■ The middle thyroid vein is isolated and divided.
■ The superior parathyroid gland is identified and preserved, given that the inferior glands are at higher risk for injury during dissection of the substernal extent of the thyroid gland.
■ When necessary, devascularized or excised parathyroid glands may be autotransplanted into the sternocleidomastoid muscle. Perform frozen section confirmation of histology prior to reimplantation.
■ The superior thyroid pedicle is isolated and divided close to the superior pole, taking care not to injure the superior laryngeal nerve or superior parathyroid gland.
IDENTIFICATION OF RECURRENT LARYNGEAL NERVE
■ The RLN is identified. The size and bulk of the thyroid gland may make this dissection difficult, and the nerve may be displaced from its standard anatomic position. In general, its entry into the larynx at the cricothyroid joint is the most consistent and reliable location for identification.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








