■ In patients with primary HPT, 85% to 90% will have a single adenoma, 5% to 10% hyperplasia, 3% to 4% double adenoma, and less than 1% carcinoma.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ Primary HPT occurs in 1 out of every 500 women and 1 out of every 2,000 men. It most commonly occurs in women between the ages of 50 and 60 years.
■ Most patients with primary HPT are diagnosed as a result of the incidental hypercalcemia detected on blood work that is obtained for an unrelated medical problem. Patients often have nonspecific symptoms such as fatigue, weakness, constipation, and depression.
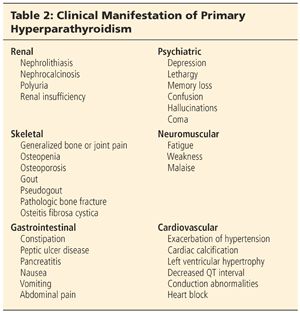
■ Patients with primary HPT may present with plethora of clinical manifestations (Table 2). Nephrolithiasis is the most common metabolic complication of primary HPT occurring in 15% to 20% of patients; however, only 2% to 5% of patients with kidney stones have primary HPT.
■ Approximately 3% of patients may present with hyperparathyroid crisis manifested by severe hypercalcemia (serum calcium >14 mg/dL), nausea, vomiting, dehydration, and central nervous system dysfunction including coma.1
■ Primary HPT is associated with a higher risk of cardiovascular disease and mortality that decreases after parathyroidectomy.2
■ A prior history of head or neck radiation in childhood, radioiodine treatment, and long-term lithium therapy are associated with a greater prevalence of primary HPT.
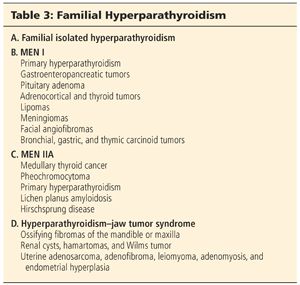
■ In 5% of patients, primary HPT is an inherited syndrome, underscoring the importance of obtaining a thorough family history. Familial HPT is inherited as an autosomal dominant syndrome with primary HPT occurring as an isolated entity or as part of multiple endocrine neoplasia (MEN) I, MEN IIA, or the hyperparathyroidism–jaw tumor syndrome (Table 3). Patients with hyperparathyroidism–jaw tumor syndrome have more severe hypercalcemia and a 10% to 15% incidence of parathyroid cancer.
■ In most patients with primary HPT, the physical examination is normal. Less than 5% of patients with primary HPT will have a palpable parathyroid tumor. Patients with hyperparathyroid crisis are more likely to have a palpable neck mass.
■ A palpable neck mass in patients with primary HPT should raise suspicion for parathyroid cancer or an associated thyroid nodule.
■ Rare patients may have band keratopathy, a condition characterized by calcium phosphate deposition in the cornea, which can be identified by slit lamp examination.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ A diagnosis of primary HPT is made by an elevated serum calcium level and an elevated or inappropriately normal intact serum PTH level.
■ Up to 20% of patients have normocalcemic primary HPT with a serum calcium level in the normal range. Most patients with normocalcemic primary HPT are diagnosed as a result of evaluation for kidney stones, osteoporosis, or osteopenia. Vitamin D deficiency, excess phosphate intake, low calcium set point, and hypo- or hypermagnesemia may be contributory factors to normocalcemic HPT.
■ Patients with primary HPT may have low or low normal serum phosphate and high serum chloride, alkaline phosphatase, and uric acid levels. Alkaline phosphatase is elevated in patients with bone disease.
■ Patients may also have a mild metabolic acidosis, which occurs because of the inhibitory effect of PTH on phosphorus and bicarbonate reabsorption in the kidney.
■ Prior to the introduction of sensitive immunoradiometric and chemiluminescence assays for measurement of intact PTH levels, a chloride to phosphorus ratio greater than 33:1 was used to make the diagnosis of primary HPT.
■ Blood urea nitrogen, serum creatinine, and glomerular filtration rate should be measured and followed, because renal insufficiency is a known complication of primary HPT.
■ Bone mineral density should be measured at the lumbar spine, hip, and distal radius using dual energy x-ray absorptiometry.
■ A calcium:creatinine clearance ratio should be determined if familial hypocalciuric hypercalcemia (FHH) is suspected. FHH is a rare autosomal dominant disorder characterized by asymptomatic hypercalcemia, hypocalciuria, and variable PTH elevation that results from a higher renal setpoint for calcium secretion. Patients with FHH have one or more first-degree relatives with hypercalcemia, a calcium:creatinine clearance less than 0.01, and a 24-hour urine calcium less than 100 mg. Parathyroidectomy is not indicated.
■ Once a diagnosis of primary HPT has been established, imaging should be performed to localize an abnormal parathyroid gland or glands. When an abnormal parathyroid gland can be localized preoperatively, a focused parathyroidectomy can be performed with intraoperative PTH measurement to confirm cure of the primary HPT. This minimizes dissection, shortens the operation, and reduces cost.
■ Localization studies should only be performed once a diagnosis of HPT has been established and a decision to proceed with surgical therapy has been made. The role of localization studies is to help determine the site of the incision and where in the neck to begin the exploration.
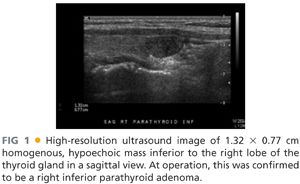
■ Office-based, high-resolution ultrasonography is the initial imaging study performed. A parathyroid adenoma appears as a homogeneous, hypoechoic, oval- or bean-shaped mass posterior to the thyroid gland (FIG 1). Occasionally, a parathyroid adenoma may be multilobulated. Ultrasound is also of value in identifying concomitant nodular thyroid disease.
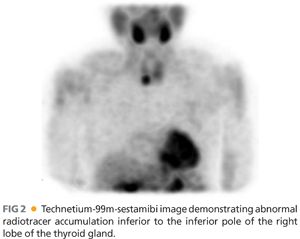
■ Technetium-99m-sestamibi with single-photon emission computed tomography (SPECT) is a combined functional and anatomic imaging study, which is obtained prior to operation. It is particularly beneficial for identifying ectopic parathyroid glands (FIG 2).
■ Four-dimensional computed tomography and positron emission tomography/computed tomography (PET/CT) fusion imaging are other potentially valuable imaging studies to help localize abnormal parathyroid glands but are usually reserved for patients with persistent or recurrent HPT.
■ Intraoperative PTH monitoring is most valuable in patients with discordant lesions on ultrasound and technetium-99m-sestamibi. It has been suggested that intraoperative PTH monitoring is unnecessary in patients with concordant lesions detected on ultrasound and technetium-99m-sestamibi imaging.
SURGICAL MANAGEMENT
■ All patients with primary HPT should be presented with option of surgical therapy, because parathyroidectomy is the only curative treatment. The classical symptoms of primary HPT (nephrolithiasis, osteoporosis, osteitis fibrosa cystica, and neuromuscular dysfunction) are well-established indications for surgery.
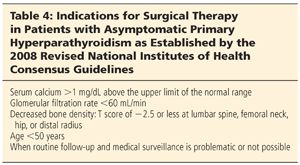
■ In patients with asymptomatic primary HPT, indications for surgical therapy have been defined by the 2008 revised consensus guidelines sponsored by the National Institutes of Health3 (Table 4). Parathyroidectomy is recommended in all patients younger than 50 years of age because at least 25% will develop one or more complications of HPT during their lifetime, which can be irreversible. Significant hypercalcemia, renal dysfunction, reduction in bone mineral density, and inability or unwillingness to participate in subsequent medical surveillance and follow-up are other indications for parathyroidectomy in patients with asymptomatic primary HPT.
■ Open neck exploration for primary HPT is performed as an outpatient procedure under general anesthesia or local anesthesia with sedation. Various intraoperative adjuncts may be used including ultrasound, PTH monitoring, and radio guidance.
■ Intraoperative ultrasound may be used to help determine the best site for the incision.
■ Intraoperative PTH monitoring may be used to help determine that all hyperfunctioning parathyroid tissue has been excised and to confirm cure of primary HPT.
■ Administration of technetium-99m-sestamibi prior to operation and use of a gamma probe intraoperatively is used by some surgeons to help localize abnormal parathyroid tissue and confirm ex vivo that a sestamibi-avid parathyroid gland has been removed and that no sestamibi-avid glands remain in the neck. Some of the limitations of this technique include that hyperplastic parathyroid glands are most often not sestamibi-avid, and thyroid nodules may also retain sestamibi, producing false-positive results.
■ For a single adenoma localized preoperatively, a unilateral focused parathyroidectomy with intraoperative PTH monitoring to confirm cure of primary HPT is performed.
■ Bilateral neck exploration is indicated for patients with negative preoperative imaging or when bilateral disease is detected preoperatively and for patients with a higher likelihood of multiglandular disease such as patients with MEN I, MEN IIA, or lithium-associated HPT. It may also be necessary for patients with associated thyroid disease. Bilateral neck exploration may also be preferentially used in all patients with primary HPT.
■ Patients with a double adenoma are treated with resection of the two enlarged glands.
■ Patients with parathyroid hyperplasia are preferentially treated with subtotal parathyroidectomy, leaving a well-vascularized parathyroid remnant that approximates the weight and size of one normal parathyroid gland. A bilateral transcervical thymectomy is also performed because of a 5% to 15% incidence of supernumerary parathyroid glands, which are most commonly found in the thymus. Alternatively, a total parathyroidectomy and parathyroid autotransplantation into the brachioradialis muscle of the nondominant forearm may be performed (see Chapter 42).
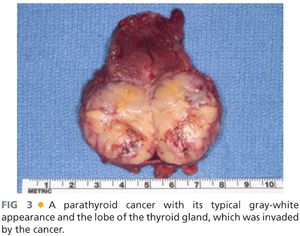
■ Patients with parathyroid cancer are treated with an en bloc resection of the tumor and the surrounding structures that are invaded. This usually involves resection of the lobe of the thyroid gland and the strap muscles.
■ Patients with parathyroid cancer usually present with marked elevation in serum calcium and PTH levels and they may have a palpable neck mass. Parathyroid cancer typically has a gray-white appearance and diagnosis is confirmed by the presence of local invasion of surrounding structures (FIG 3).
Preoperative Planning
■ Serum levels of 25-hydroxy-vitamin D and alkaline phosphatase are measured preoperatively. Patients with low 25-hydroxy-vitamin D and elevated alkaline phosphatase levels are at increased risk for symptomatic postoperative hypocalcemia.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








