and Ziv Gil2
(1)
Division of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
(2)
The Head and Neck Center Department of Otolaryngology Head and Neck Surgery, Rambam Healthcare Campus, Haifa, Israel
Keywords
SubfrontalAnterior skull baseFrontalCribriform plateTransglabellarThe subcranial approach is a single-stage open procedure for patients with tumors involving the anterior skull base. It is also known as the subfrontal or the transglabellar approach. The concept of a broad subcranial approach to the entire anterior skull base was first introduced by Raveh for cases of traumatic injuries and was later adapted for surgical removal of tumors involving this anatomic region. The extent of exposure of the subcranial approach includes the frontal sinus anteriorly, the clivus posteriorly, the frontal lobe superiorly, and the paranasal sinuses inferiorly. Laterally, the boundaries of this approach are both superior orbital walls. The subcranial approach has advantages over the traditional craniofacial resection: (1) it affords a broad exposure of the anterior skull base from below rather than through the transfrontal route; (2) it provides excellent access to the medial orbital walls and to the sphenoethmoidal, nasal, and paranasal cavities; (3) it allows simultaneous intradural and extradural tumor removal and safe reconstruction of dural defects; (4) it does not require facial incisions; and (5) it is performed with minimal frontal lobe manipulation. Although endonasal surgery replaced some of the indications that were traditionally managed by this approach, there are still indications for subcranial resection, including tumor infiltration to the frontal sinus skin and subcutaneous tissue, mid and lateral orbital planes, palate, nasal bones, lacrimal sac, and massive dural and brain parenchyma.
The subcranial approach involves coronal incision and osteotomy of the naso-fronto-orbital bone segment, which allows access to the intra- and extracranial compartments of the anterior skull base. Although the subcranial approach permits complete tumor resection in the majority of cases, there are still situations in which the inferior, lateral, or posterior aspects of the tumor are not adequately exposed. These situations include neoplasms with extensions to the lateral maxillary wall, palate to the cavernous sinus posteriorly, to the orbital apex, pterygopalatine fossa laterally, and inferior aspect of the clivus inferoposteriorly.
For some of these tumor extensions in adjacent compartments, the subcranial approach may be coupled with the midfacial degloving, pterional orbito-zygomatic, or transnasal endoscopic approaches.
In this chapter we describe the surgical procedure of the subcranial approach that is used in our institution for removal of tumors involving the anterior skull base and paranasal sinuses.
5.1 Preoperative Evaluation and Anesthesia
All patients scheduled for operation are evaluated preoperatively by a head and neck surgeon, a neurosurgeon, and an anesthesiologist. Patients younger than 18 years are also examined by a pediatric oncologist. If a free flap is planned, preoperative physical examination by a reconstructing surgeon is essential. Radiologic evaluation of the patients includes axial and coronal computed tomography (CT) and magnetic resonance imaging (MRI, MRA) of the head and neck. Neuroangiographic evaluations may also be performed in cases of highly vascular tumors invading the skull base or the cavernous sinus for preoperative balloon-occluding testing or preoperative embolization. Figures 5.1 and 5.2 show typical preoperative CT and MRI scans of patients with tumors involving the anterior skull base.
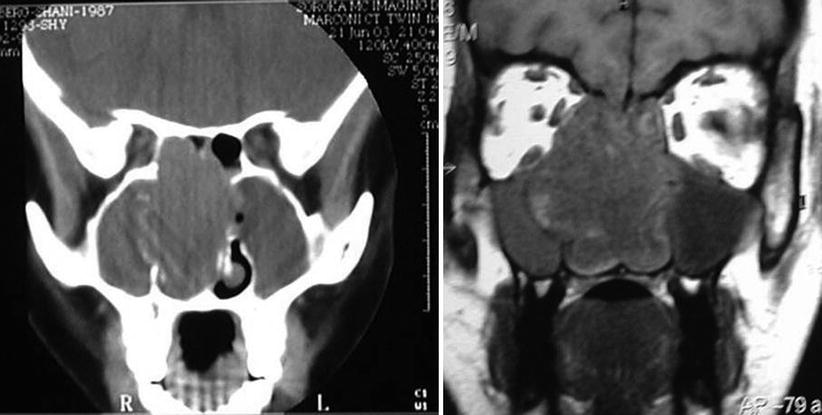
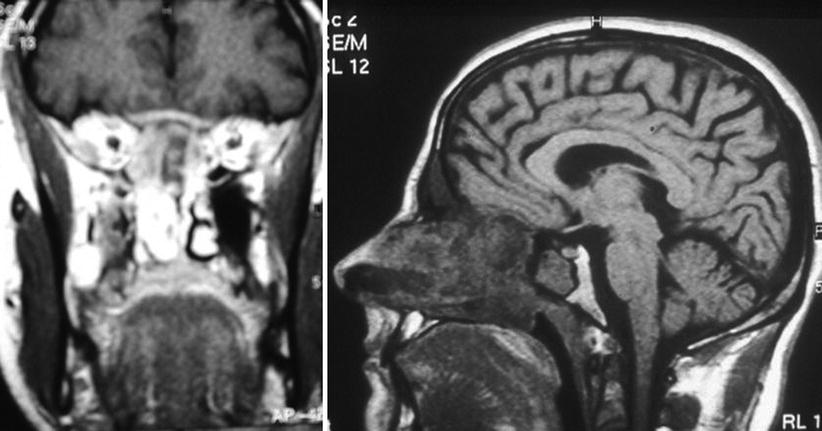
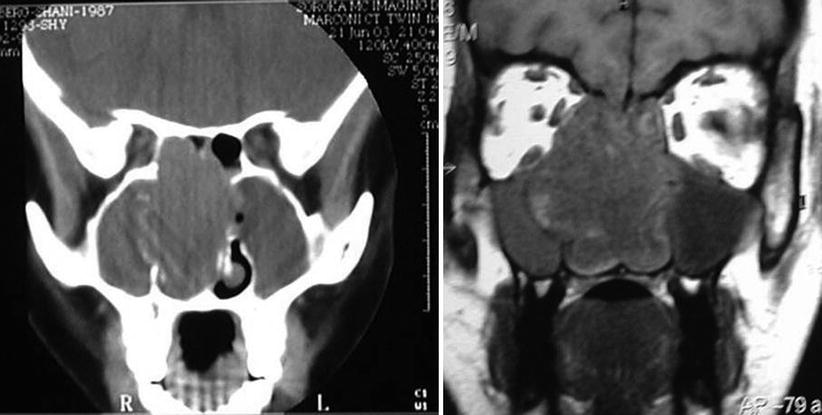
Fig. 5.1
A preoperative coronal CT (left) and MRI (right) of a 16-year-old girl with esthesioneuroblastoma invading the anterior skull base, nasal cavity, and right maxillary sinus
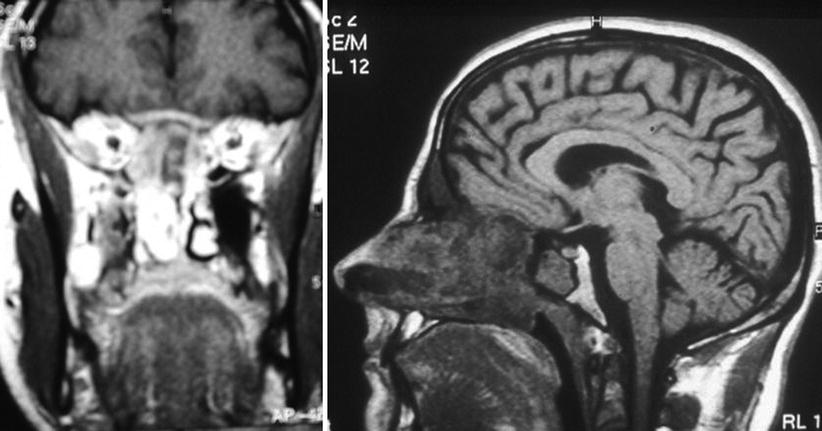
Fig. 5.2
A preoperative MRI of a 53-year-old man with recurrent squamous cell carcinoma invading the anterior skull base, nasal cavity, and frontal sinus
Tissue diagnosis is performed in all cases amenable for biopsy. This can be quiet easily performed with the use of the transnasal endoscopy.
Patients who have undergone prior skull base or craniofacial procedures for extirpation of malignant tumors are also evaluated using a positron emission tomography-CT hybrid (PET-CT) prior to the operative procedure. The PET part of PET-CT is performed twice, using two-dimensional and three-dimensional acquisition protocols for comparison purposes. We reported an upstaging of 20 % of the patients (10 of 50) using this method. Electromyographic monitoring of the cranial nerves and neuronavigation may be also used.
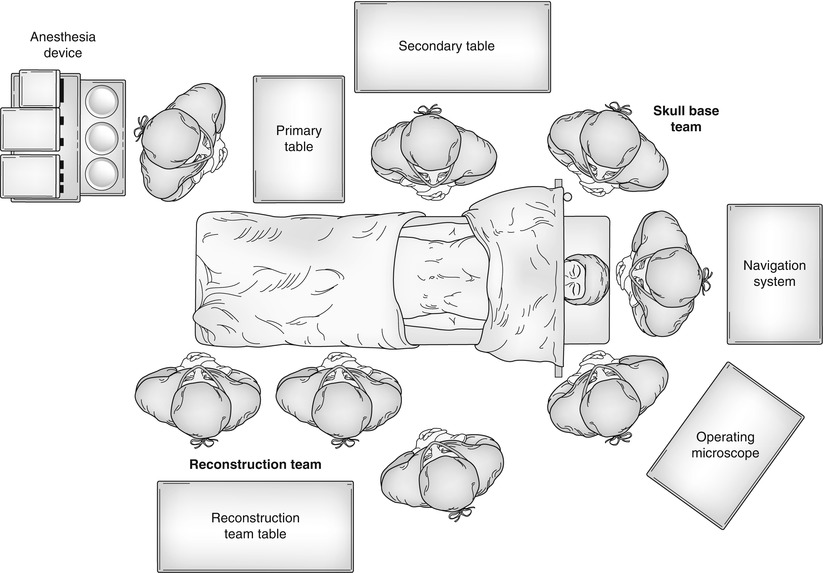
5.1.1 Operative Room Setting
We recommend routinely shampooing the patient’s head with chlorhexidine (Septal Scrub [Teva Medical; Ashdod, Israel]) the night before the operation. Broad-spectrum antibiotics are given perioperatively. All patients are operated on in the supine position, and the hair is not shaved at the surgical site. A tracheostomy is not performed. A lumbar spine catheter may be inserted for a period of 3 days for cerebrospinal fluid (CSF) drainage to facilitate frontal lobe retraction and to reduce the risk of postoperative CSF leak.
5.2 Surgical Technique
After the induction of anesthesia, the patient’s hair is shampooed vigorously with 4 % weight per volume (w/v) chlorhexidine, parted with a sterile comb along the proposed incision line, and tied in clumps with rubber bands. The hair is not shaved. The operative field is then scrubbed with surgical sponges containing chlorhexidine solution (0.05 % w/v) and draped with sterile towels that are clipped in place with surgical staples.
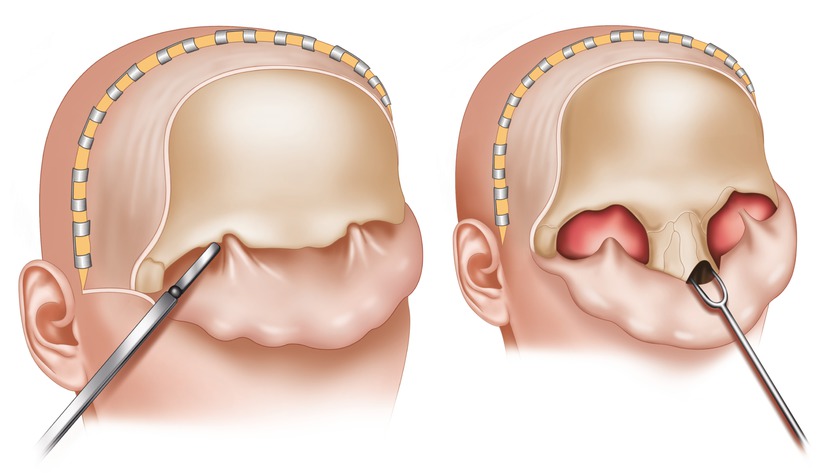
The skin is incised above the hairline and a bicoronal flap is created in a supraperiosteal plane. A flap is elevated anteriorly beyond the supraorbital ridges and laterally superficial to the temporalis fascia (Fig. 5.3). The pericranial flap is elevated up to the periorbits, and the supraorbital nerves and vessels are carefully separated from the supraorbital notch. The lateral and medial walls of the orbits are then exposed, and the anterior ethmoidal arteries are clipped or coagulated. The pericranium is elevated above the nasal bones, and the flap is rotated forward and held over the face throughout the rest of the procedure (Fig. 5.3). Titanium micro- or miniplates are applied to the frontal bones and removed before performance of the osteotomies to ensure the exact repositioning of the bony segments at the end of the operation. An osteotomy of the anterior or the anterior and posterior frontal sinus walls, together with the proximal nasal bony frame, part of the superior and medial wall of the orbit, and a segment of the superoposterior nasal septum, is then performed. For a type A osteotomy, the anterior frontal sinus wall and the proximal nasal frame are osteotomized and removed in one block (Fig. 5.4 top). This approach is usually used in cases of anteriorly located, mostly benign tumors. If a type B osteotomy is planned, burr holes are made and the posterior frontal sinus wall is resected after the dura has been detached from the frontal, orbital, and ethmoidal roofs (Fig. 5.4 bottom). A part of the distal nasal bone is preserved in order to support the nasal valve. In cases of lateral invasion of a tumor, the osteotomy lines can be extended to include the lateral segments of the orbital roofs. After the fronto-naso-orbital bone segment is osteotomized, it is stored in saline until the reconstructive procedure (Fig. 5.5). A bilateral ethmoidectomy and a sphenoidotomy are then performed: this approach enables the exposure and assessment of the tumor in its circumference (Fig. 5.6). The tumor is removed at this stage (Fig. 5.7), and the dura or brain parenchyma is also resected when involved by tumor (Fig. 5.8). Frozen sections may be taken during surgery in order to assess the tumor’s margins. One side of the cribriform plate and olfactory filaments can be preserved whenever possible in order to prevent postoperative anosmia.