and Ziv Gil2
(1)
Division of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
(2)
The Head and Neck Center Department of Otolaryngology Head and Neck Surgery, Rambam Healthcare Campus, Haifa, Israel
Keywords
Infratemporal fossaPterionalOrbitozygomaticSphenoid boneMiddle fossa6.1 Introduction
Less than 1 % of all head and neck neoplasms originate in the lateral skull base. Tumors in this anatomical compartment can be either primary tumors, originating in the skull base itself, or secondary tumors, which infiltrate the skull base from adjacent organs. Primary tumors can originate from nerve, vessels, muscle, bone, cartilage, or connecting tissue. Secondary tumors are usually carcinomas and sarcomas. Common benign tumors include osteoma, fibrous dysplasia, meningioma, large juvenile angiofibroma, and schwannoma. Among the malignant tumors, squamous cell carcinoma, adenocarcinoma, adenoid cystic carcinoma, and sarcoma are the most common. These tumors may go undetected for a long time. They can present as an asymptomatic mass in the temporal area or can be associated with skin ulceration, severe pain, and neurological deficits.
The clinical presentation of these tumors is directly related to the location of the lesion and its histologic type. The patient should be questioned regarding symptoms of cranial nerve dysfunction, head- and earaches, trismus, bleeding from the ear, and otorrhea. Common symptoms and signs suggestive of tumors are facial swelling and asymmetry, palpable metastatic adenopathy, hearing loss, numbness or pain of the face, and neurological or ocular manifestations. Pain is a significant adverse symptom suggesting a malignant tumor. Comorbidity risk factors should be identified, including mental disorders and active abuse of alcohol, drugs, or tobacco.
The surgical approach is tailored according to the anatomical extent of the tumor, its histologic type (benign or malignant), and the patient’s medical history (previous surgeries or radiation treatment). This chapter describes the surgical approaches to the lateral skull base.
6.2 Preoperative Evaluation and Anesthesia
6.2.1 Physical Examination
Physical examination should include a meticulous survey of the temporal area and auricular and preauricular skin. The neck and parotid gland are palpated in a search for lymph node metastases. The function of the facial and other cranial nerves is evaluated. Otoscopy is used to define the extent of the tumor in the external auditory canal. If the tympanic membrane can be seen, its integrity is verified. Jaw movement and trismus are examined as a potential sign of extension of the tumor into the temporomandibular joint. Cranial nerve function is checked. The physical exam is completed by endoscopic evaluation of the nose, sinuses, nasopharynx, and oropharynx. Masses should be examined for friability, vascularity, bleeding, and signs of necrosis, possibly suggesting malignancy and necessitating additional investigation. Different entities may display specific and pathognomonic findings on physical examination (such as a vascular mass arising from the hypotympanum on otoscopic examination), but most tumors are similar in their initial and late symptoms and demand a high level of suspicion in order to reach the correct final diagnosis. This type of tumor will silently advance in size and extent until it has infiltrated a cranial nerve or grown sufficiently to obstruct the nasopharynx. Sites of potential donor tissue to be used for reconstruction also are examined.
6.2.2 Indications for Surgery
Indications for surgery include extirpation of benign and malignant tumors that originate in the lateral skull base or that invade this compartment from neighboring structures. Rarely, this approach is performed for treatment of infectious diseases, including local abscess or necrotizing fasciitis. Surgery can be considered in selected cases for palliative treatment, when other modalities are not possible. When contemplating treatment of a specific patient, the following key questions need to be addressed:
What is the goal of the treatment?
What is the appropriate extent and nature of surgical resection?
Is postoperative adjuvant therapy with radiation or chemoradiation anticipated?
What reconstruction techniques will be employed?
6.2.3 Contraindications
Tumors amenable to chemoradiation therapy (lymphoma, carcinomas of oropharyngeal or nasopharyngeal origin) and evidence of distant metastases are considered contraindications for surgery. Some sarcoma cases require neoadjuvant chemotherapy treatment before surgery and other malignancies such as sinonasal undifferentiated carcinoma (SNUC) may be managed by chemoradiation alone. Hence every cancer case should be consulted with the oncology team to prevent unnecessary damage to the patient. Cancer invasion of the prevertebral fascia, encasement of the carotid artery, invasion of the cavernous sinus, and considerable brain involvement are also considered contraindications for surgery (Fig. 6.1). Stable, small paragangliomas or schwannomas can be followed radiographically with MRI. Severe comorbidity, marked debilitated status, and dementia are considered relative contraindications for surgery. For patients with adenoid cystic carcinoma, resection should be considered even when distant metastases are present.
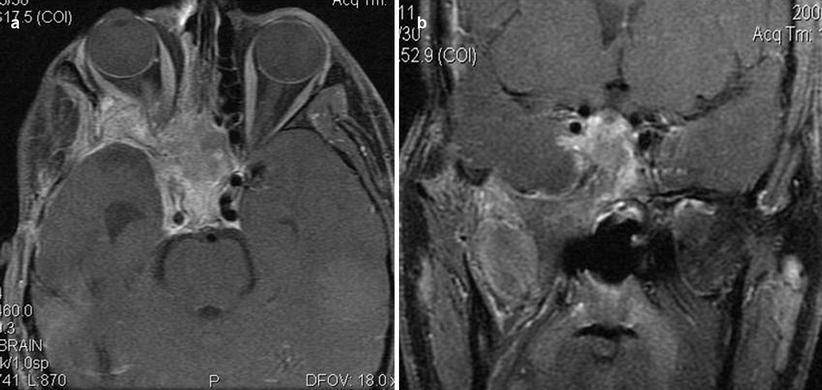
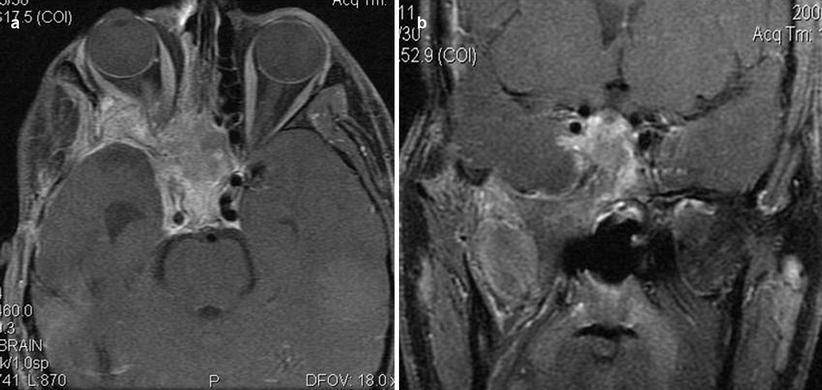
Fig. 6.1
Cancer invasion of the prevertebral fascia, encasement of the carotid artery, invasion of the cavernous sinus, or considerable brain involvement is considered a contraindication for surgery
6.2.4 Imaging Studies
Imaging is part of the preoperative evaluation and tailoring of treatment. A contrast CT scan and a basic MRI study with fat suppression are standard. A T2-weighted MRI study with fat suppression is usually added. Visualization of a vascular flow void on an MRI study is usually sufficient for the diagnosis of a vascular tumor such as a paraganglioma, but MR angiography (MRA) may be added for a more precise diagnosis. Three-dimensional reconstruction enables multiplanar imaging of tumor extension with bone involvement and vessel encasement. A hybrid of positron emission tomography (PET) and CT (PET/CT) is used as part of the preoperative staging paradigm, to assess the presence of distant metastases. The radiological evaluation must include the neck in any case of suspected malignancy, to evaluate for lymph node metastasis. Patients with highly vascular tumors (juvenile angiofibroma or paraganglioma) also require preoperative embolization a few days prior to surgery. If there is a risk of intraoperative injury to the internal carotid artery, angiographic study for contralateral blood supply through the circle of Willis is advisable.
6.2.5 Tissue Diagnosis
For extracranial tumors amenable to biopsy, tissue diagnosis should be an integral part of preoperative evaluation. Although radiological imaging could indicate the type of neoplasm, tissue diagnosis is essential for the diagnosis of both benign and malignant lesions. Fine needle aspiration (FNA) biopsy can be performed via ultrasound for suspicious lymph nodes. Some exceptions to preoperative biopsy include highly vascular tumors such as juvenile angiofibroma, hemangiopericytoma, and paragangliomas.
6.3 Surgical Technique
6.3.1 Operating Room Setting
The patient is placed in a supine position, without shaving hair at the surgical site. A lumbar spine catheter may be inserted for cerebrospinal fluid (CSF) drainage when dural resection is expected. Surgery is performed without muscle relaxation for monitoring of the spinal accessory, hypoglossal, and facial nerves during dissection.
Various incisions may be used for the resection of lateral skull base tumors (Fig. 6.2). After the induction of anesthesia, an oral endotracheal tube is inserted and secured contralateral to the surgical site. The patient is prepped and draped with the hemiface and calvarium exposed. Ointment is placed in both eyes, and the eyelid contralateral to the surgical site is taped shut. The patient’s hair is shampooed vigorously with 4 % w/v chlorhexidine (Septal Scrub®; Teva), parted with a sterile comb along the proposed incision line, and tied in tufts with rubber bands. We recommend cleansing the hair with chlorhexidine the day before the operation. The head is stabilized with a soft donut holder or Mayfield holder, and then the entire operating table is tilted at an angle with the head up, in order to minimize bleeding.
Fig. 6.2
Various incisions may be used for the resection of lateral skull base tumors
6.3.2 Skin Incision
The most commonly used incision is the question-mark incision. More extensive approaches may combine several incisions, including a preauricular modified Blair’s incision and an apron incision. Any variation of these can be used according to the tumor histology and location (Fig. 6.3). The skin is incised with a #15 blade or electrocautery and subsequent dissection of the subcutaneous tissue and the platysma is carried out with an electrocautery instrument at the lowest effective setting.