21 The stiff hand and the spastic hand
Synopsis
 Flexion and extension contractures may result from contractures of structures volar or dorsal to the joint, capsular/pericapsular structures, and bony deformity.
Flexion and extension contractures may result from contractures of structures volar or dorsal to the joint, capsular/pericapsular structures, and bony deformity.
 Non-operative treatment is more effective in the early phase following injury and includes splinting, extremity elevation, compression gloves, moist heat, and ultrasound.
Non-operative treatment is more effective in the early phase following injury and includes splinting, extremity elevation, compression gloves, moist heat, and ultrasound.
 Surgery is indicated for residual flexion contractures refractory to nonoperative measures.
Surgery is indicated for residual flexion contractures refractory to nonoperative measures.
 Checkrein ligament release is key in PIP joint flexion contracture surgery.
Checkrein ligament release is key in PIP joint flexion contracture surgery.
 Postoperative splint application maintains surgical correction.
Postoperative splint application maintains surgical correction.
 Salvage procedures for PIP joint flexion include disarticulation at the PIP joint or bone shortening with PIP joint fusion.
Salvage procedures for PIP joint flexion include disarticulation at the PIP joint or bone shortening with PIP joint fusion.
 In the spastic hand, nonsurgical treatment for cerebral palsy includes splinting, occupational therapy, intramuscular botulinum toxin A and intrathecal baclofen.
In the spastic hand, nonsurgical treatment for cerebral palsy includes splinting, occupational therapy, intramuscular botulinum toxin A and intrathecal baclofen.
The stiff hand
Diagnosis/patient presentation
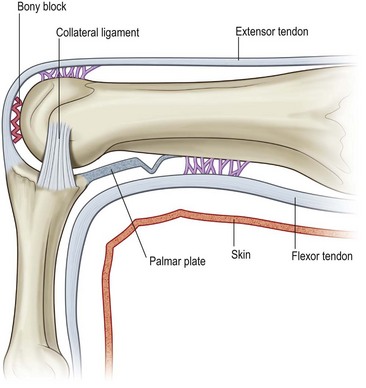
Flexion contracture (Fig. 21.1)
This may result from tightness in one or more of the structures on the palmar aspect of the joint1,2:
• Skin: Contracture from scarring results from lacerations or palmar burns
• Palmar fascia: Dupuytren’s contracture is the classic example
• Flexor tendon sheath: Shortening and contracture may occur
• Flexor tendon: This is due to tendon shortening or tendon adhesions. Temporary joint fixation in a particular position with locking and release by painful manipulation may result from a trigger finger within the tendon sheath but also may occur within the joint especially at the metacarpophalangeal (MP) joint (intracapsular tumors, loose bodies, osteophytes, articular surface distortions).
Capsular and pericapsular structures
Collateral ligament
The collateral ligament at the proximal interphalangeal (PIP) joint is taut in all positions of the joint and collateral ligaments are taut in flexion only at the MP joints.3 Thus, collateral ligament shortening never produces a flexion contracture at either joint. However, collateral ligament adherence to the lateral aspect of the proximal phalanx when the finger is flexed, does play a role in PIP joint flexion contracture.
Extension contracture
Limitation of flexion (extension contracture) (Fig. 21.2) can be caused by one or more structures on the dorsal aspect of the joint.1,2 However, they too can result from a “jamming” effect of volar structures that block flexion, such as a bone block or palmar plate adhesions.
Intrinsic muscles
Intrinsic contracture may follow ischemia, or muscle fibrosis may occur for nonischemic reasons (rheumatoid arthritis, cerebral palsy). The “intrinsic plus” position of the hand results in which the fingers are flexed at the MP joints and extended at the interphalangeal joints.3 A “saddle deformity”4 results from adhesions between lumbrical and interosseous muscles. With active intrinsic contraction, painful impingement on the deep transverse metacarpal ligament occurs with limitation of flexion (the transverse metacarpal ligament is the “saddle” and the two muscles are the “legs of the rider.”)
Capsular and pericapsular structures
Collateral ligaments
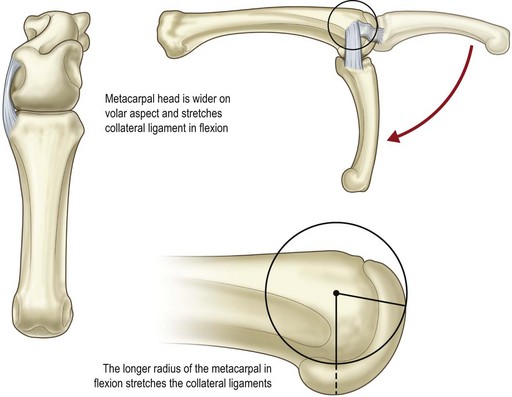
Adhesions to the head of the proximal bone may limit flexion. In contrast to flexion contracture, which is more common in interphalangeal joints (especially proximal), stiffness in extension from collateral ligament shortening is more likely at MP joints. Collateral ligaments at the MP joints are relaxed in extension and taut in flexion.5 Loss of MP joint flexion can come about simply from immobilization in the incorrect, extended position. Collateral ligaments are at their tightest (the cam arc effect of the metacarpal head) at a range between 70° and 90° flexion.
Volar plate
Flexion is prevented by volar plate adhesions to the palmar surface of the proximal bony head. Palmar plate adhesions and collateral ligament tightness may both be causes of MP joint extension contracture.1 They may be distinguished from each other. If the collateral ligaments are contracted, finger abduction–adduction in extension (normally about 45°) is greatly reduced. When palmar plate is the sole cause, attempted passive flexion produces an opening of the dorsal aspect of the joint. The volar lip at the base of the proximal phalanx jams against the adherent volar plate, and the unaffected (loose) collateral ligaments allow the flexion force to rock the dorsal lip away from the metacarpal head, felt as a subtle dorsal recess between head and base. This sign should always be sought intraoperatively as a residual impediment to passive flexion after tight collateral ligaments have been released.
Painful resistance to passive PIP joint flexion may indicate volar plate injury (volar plate test).6 Pain results from synovial involvement, and the most common cause is volar plate avulsion with or without a small bone fragment torn from the base of the middle phalanx. Positive volar plate test at 6–9 months following injury indicates that volar plate repair of the middle phalanx may be necessary.
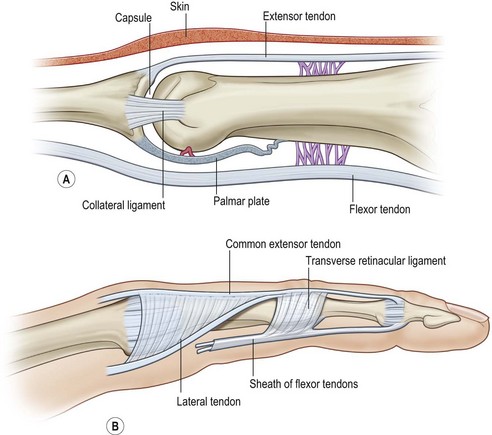
Transverse retinacular ligaments
Transverse retinacular ligaments may be adherent to the lateral capsular ligament at the PIP joint.
Bone
This may be a true block or result from intraarticular incongruity. Chondral fractures may not be radiographically apparent and so may present a diagnostic problem (Fig. 21.3). Persistent waxing and waning joint swelling with limited flexion may result from a chondral fracture, which is more likely at the MP joint. Questioning of the patient may lead to recollection of an injury that could have caused the proximal phalangeal base to impinge on the metacarpal head. Surgical exploration may reveal the chondral fracture and consequently loose body in the joint. Computed tomography scanning may help in arriving at the correct diagnosis.
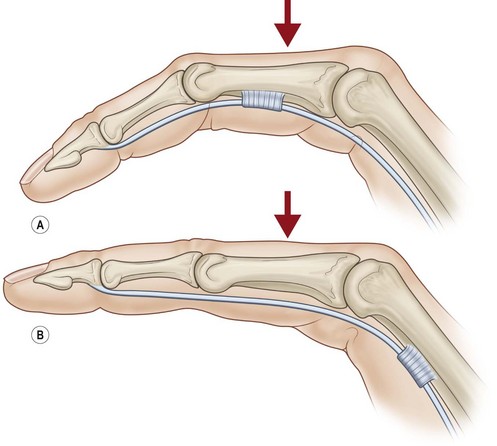
Seesaw effect
This results when a contractural element spans two joints. Presence of this sign helps in the diagnosis of structures that potentially contribute to a stiff joint.7 If one joint in a contracted system is flexed, the other joint can then be extended, and vice versa. This is seen, for example, when a longitudinal volar skin scar crosses both proximal and distal interphalangeal joints. The DIP joint can be extended only if the PIP joint is flexed. A similar effect is seen with adherent extrinsic flexor or extensor tendons (Fig. 21.4). For example, flexion of MP joints in the presence of a flexor tendon adhesion over the proximal phalanx has no effect on the flexion contracture of the PIP joint. If the adhesion lies proximal to the MP joint, flexion of that joint results in correction of the contracture apparently present in the PIP joint. Furthermore, with flexor tendon adhesions, passive flexion of the affected joint exceeds active flexion, provided the extensor tendon is healthy. Similarly, in the presence of a Volkmann contracture of the flexors in the forearm, passive extension of the finger joints is reduced with the wrist extended and not if the wrist is flexed.
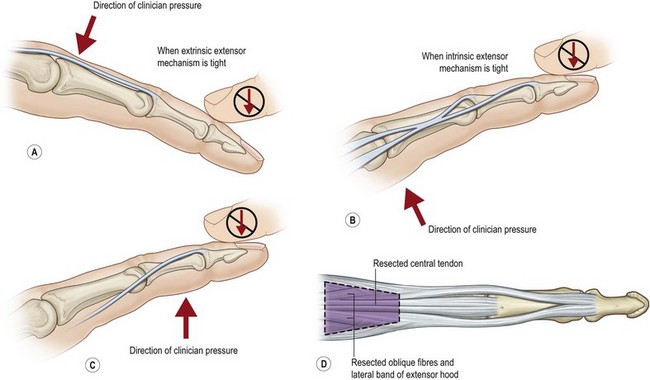
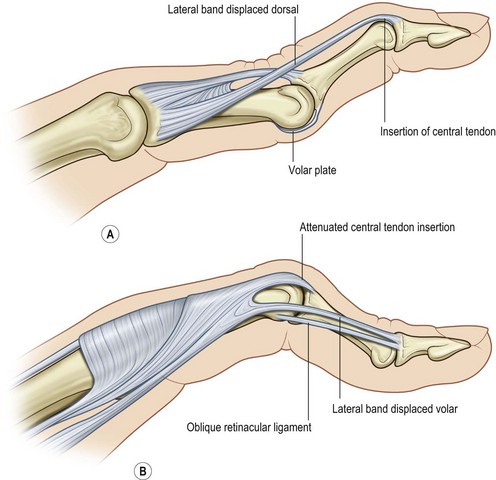
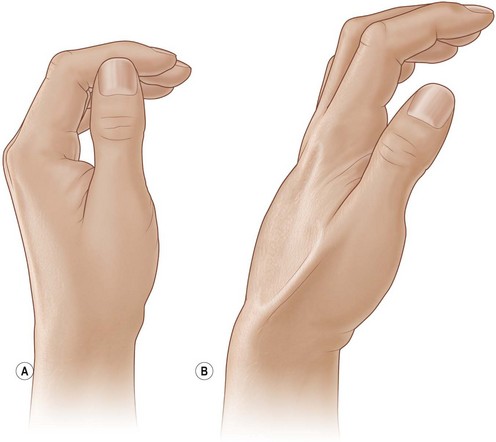
If the extrinsic extensor tendon is adherent to the metacarpal, the limitation of extensor tendon excursion distal to that joint prevents simultaneous flexion of MP and PIP joints. This is the test for extrinsic tightness (Fig. 21.5A).8,9 The test of Bunnell for intrinsic tightness results from the seesaw phenomenon in which the band acts across two joints but is an extensor of one joint and a flexor of the adjacent joint.10 If the intrinsic musculotendinous system is foreshortened, extension of the MP joint either actively or passively increases the tone in the system and restrains flexion of the PIP joint. This is tested by passively extending the MP joint and passively flexing the PIP joint (Fig. 21.5B). If flexion of the PIP joint is greater when the MP joint is flexed than when it is extended, intrinsic tightness is present. In the swan-neck deformity, not only is there an extension contracture of the PIP joint, but that joint hyperextends because of volar plate laxity. There is dorsal displacement of the lateral bands at the PIP joint. This slackens the distal tension on the extensor mechanism because of the fixed attachment of the central tendon at the PIP joint. Thus there is unopposed force of the flexor digitorum profundus at the distal joint, which then drops into flexion (Fig. 21.6A).9
A similar volar to dorsal seesaw effect occurs at the DIP joint secondary to action of the oblique retinacular ligament and lateral bands, resulting in extension contracture at that joint. This occurs with the boutonniere deformity. When the central tendon insertion into the dorsal base of the middle phalanx ruptures or attenuates, the PIP joint drops into flexion and the lateral bands move volar to the axis of motion of that joint.11 They will foreshorten and adhere in that position. Excess extensor pull that secondarily bypasses the PIP joint is imposed dorsally at the DIP joint with consequent recurvature at that joint (Fig. 21.6B). The oblique retinacular ligament is an extensor of the DIP joint and a flexor of the PIP joint.11 It also foreshortens and this permits the DIP joint to be flexed as long as the PIP joint is maintained in flexion. Passively extending the PIP joint brings the DIP joint into extension, making passive flexion increasingly more difficult. This maneuver is the Boutonniere test (Fig. 21.5C).
Volar plate and collateral ligament changes
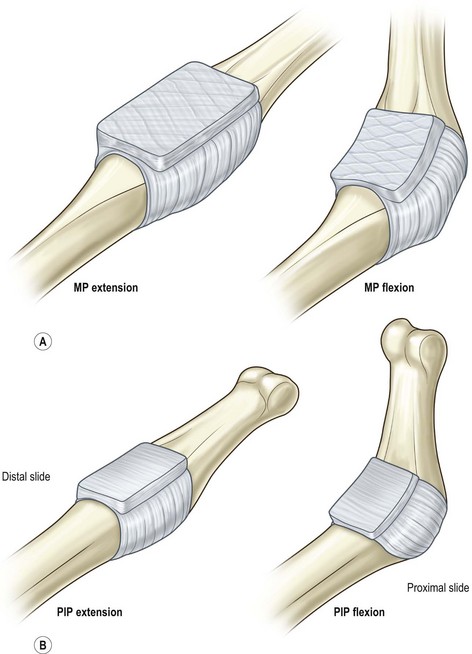
The protected position of MP joints is in flexion. The cam and volar flare shape of the metacarpal head places collateral ligaments in greatest tension during flexion (Fig. 21.7). The MP joint volar plate has criss-crossing bands of fibers that expand with joint extension and are collapsible with flexion.6 Thus, the volar plate at the MP joint is considerably longer in extension than in flexion (Fig. 21.8A).
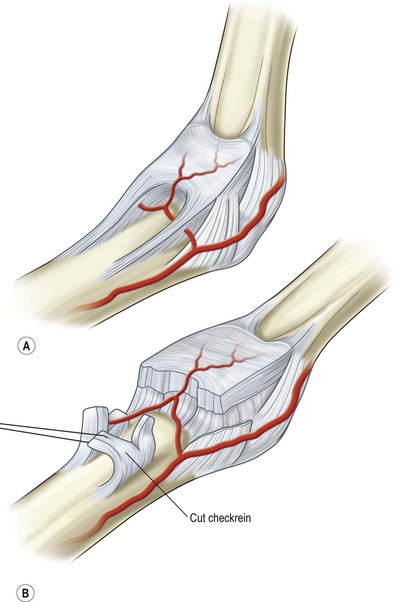
In contrast, the interphalangeal joint collateral ligaments do not change in tightness with joint flexion and extension. The volar plate is relatively uncollapsible. Rather, the volar plate slides proximally and distally with flexion and extension of the joint (Fig. 21.8B). The volar plate is not attached to the proximal phalanx as this would prevent full extension. The assembly lines are the two ridges on the volar lateral surfaces of the phalanx to which are attached the flexor sheath, Cleland ligaments, Grayson ligaments, oblique retinacular ligaments, and transverse retinacular ligaments, and the transverse metacarpal ligament and MP joint volar plate more proximally. Normally, there is no ligament structure between the volar plate of the PIP joint and the assembly line or extension of that joint would not be possible. Two bands (checkreins)6,12,13 form between the lateral proximal volar plate and the assembly lines after injury. These are pathologic structures (Fig. 21.9). They are thicker at the base attached to the volar plate and have a thinner longer proximal apex attached to the assembly line. The communicating artery of the vincula system passes deep to the checkreins. With interphalangeal joint contracture it is the checkreins that mainly prevent extension. Division of these checkreins and accessory collateral ligaments enables extension at the interphalangeal joint to be achieved when surgery is required. It is virtually never necessary to divide collateral ligaments.
Basic science/disease process
Injury, infection, excessive immobilization, and inappropriate splinting of the hand all predispose to joint stiffness. The initial response to any insult of the hand is edema formation. Unless edema accumulation is prevented, joints assume the posture in which their ligaments are most relaxed.1,14,15 Ligament contracture and fibrosis then cause joints to become immobile in this position (Fig. 21.10), which is:
This is the negative or injured hand position; wrist position and MP joint posture are the keys to its development. When the wrist is allowed to flex, increased tone in the extrinsic extensor tendons causes MP joints to extend. When nearly fully extended, the MP joint has maximum capsule and collateral ligament laxity as well as intracapsular fluid capacity. When the MP joint is fully flexed, intracapsular fluid capacity is minimal and the ligaments are taut. After injury, edema fluid drives the MP joints hydraulically into extension. In this position, tension is increased in the flexors and decreased in the extensors. Thus, fingers flex at PIP and DIP joints. There is no hydraulic drive at PIP or DIP joints because there is only minimal change in collateral ligament tightness and fluid capacity of flexed versus extended interphalangeal joints. Positional changes in interphalangeal joints are thus secondary to changes in MP joints. Slight wrist flexion occurs in the neglected edematous hand because total power of flexors exceeds the extensors.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree