11.1 Facelift
Principles
Synopsis
 Age-related changes occur in all layers of the face, including skin, superficial fat, SMAS, deep fat, and bone.
Age-related changes occur in all layers of the face, including skin, superficial fat, SMAS, deep fat, and bone.
 Patients presenting for facial rejuvenation surgery are usually middle aged or older, thus increasing the chance of underlying medical problems. Risk factors such as hypertension and smoking should be dealt with prior to facelift surgery.
Patients presenting for facial rejuvenation surgery are usually middle aged or older, thus increasing the chance of underlying medical problems. Risk factors such as hypertension and smoking should be dealt with prior to facelift surgery.
 A careful preoperative assessment will provide the surgeon with an aesthetic diagnosis regarding the underlying facial shape, the age related issues which predominate and the appropriate surgical procedures for every individual patient.
A careful preoperative assessment will provide the surgeon with an aesthetic diagnosis regarding the underlying facial shape, the age related issues which predominate and the appropriate surgical procedures for every individual patient.
 Almost all facelift techniques begin with a subcutaneous facelift flap. Careful incision placement, tissue handling, and flap repositioning are important in order to avoid the obvious stigmata of facelift surgery.
Almost all facelift techniques begin with a subcutaneous facelift flap. Careful incision placement, tissue handling, and flap repositioning are important in order to avoid the obvious stigmata of facelift surgery.
 Volume augmentation, and in some locations volume reduction, should be considered in all cases of facelift surgery.
Volume augmentation, and in some locations volume reduction, should be considered in all cases of facelift surgery.
 Facial aging is usually a pan-facial phenomenon. Therefore, in order to obtain a harmonious result, patients will often benefit from surgery to other components of their face.
Facial aging is usually a pan-facial phenomenon. Therefore, in order to obtain a harmonious result, patients will often benefit from surgery to other components of their face.
 The most common complication of facelift surgery is hematoma. This problem should be dealt with promptly.
The most common complication of facelift surgery is hematoma. This problem should be dealt with promptly.
Introduction
A complete discussion of facial rejuvenation would involve the periorbital region, forehead, cheek, neck, and perioral region. (The periorbital zone is reviewed in Chapter 8 and the forehead in Chapter 7.) In this chapter, we will be dealing with the middle and lower thirds of the face – the cheek and neck. Terminology for procedures which address these areas include rhytidectomy, rhytidoplasty, meloplasty and facialplasty, although in this text, the more common term, “facelift” will be used.
History
Facelift surgery dates from the early part of the 20th century. Its colorful history has been thoroughly reviewed by Stuzin,1 whose summary is reproduced here.
In the past, the history of aesthetic facial surgery has been reported by a number of authors, including: Rogers,2,3 Rees and Wood-Smith,4 Gonzalez-Ulloa,5 Rees6 and Barton.7,8
There is still doubt as to who performed the first facelift, but most sources date it to the first decade of the 20th century.3,9,10 According to Rogers,3 Hollander11 reported in a chapter entitled “Cosmetic Surgery” in Handbuch der Kosmetik that “as a victim of the art of feminine persuasion,” he removed pieces of skin at the margins of the hairline and in the natural aging skinfolds of a woman to freshen up “her wrinkles and drooping cheeks”. In this chapter, Hollander did not date the procedure, but in 1932 he stated that his original procedure had been performed in 1901 for a Polish aristocrat.12 Lexer,10 however, reported in 1931 that he had performed a facelift for an actress in 1906 and that he was unaware of any such operation before that date. Joseph9 reported in 1921 that he had performed an operation in 1912 for correction of aging cheek tissues in a 48-year-old woman. By the time Hollander, Lexer, and Joseph reported their first procedures, a number of other prominent surgeons in Europe, such as Noel, Passot, Morestin, Bourguet, and Lagarde, were busy performing cosmetic surgical procedures. In the United States, Miller and Kolle had large cosmetic surgery practices. Passot13 in 1919 published an illustrated article showing sites of elliptic skin excision of the hairline, the forehead, and the temporal and preauricular areas to tighten the skin and an elliptic excision of skin and fat to reduce submental fat deposits. Bourguet14 reported elliptic skin excisions similar to those of Passot. He was the first to report fat excisions to correct herniated periorbital fat pads (1924)15 and to publish preoperative and postoperative photographs of fat pad excision (1925).16 Noel published a book in 1926,17 La Chirurgie Esthetique: Son Role Social, describing facialplasty, blepharoplasty, forehead lifting, and correction of loose skin of the neck, burns, scars, protruding ears, and laxity of the upper arms. Although her procedures were not aggressive by modern standards, Noel was a true master of that era.
Miller18 published the first book in medical history devoted entirely to the subject of cosmetic surgery. Miller was described by Rogers3 as a “quack” on one hand and at the same time, “a surgical visionary years ahead of his academic colleagues … medicine’s first truly cosmetic surgeon.” Miller was a prolific writer. In 1906, he wrote the first article in the medical literature describing an attempt to remove excess skin from the eyelids.19 In 1907, he published the first article with a photograph illustrating lower eyelid incisions,20 and he also published three cosmetic surgery textbooks.18,21,22 Kolle was born in Germany and practiced in New York. His book Plastic and Cosmetic Surgery23 represented the second description of cosmetic surgery in medical history. The book was more than 500 pages in length and contained hundreds of illustrations, including preoperative and postoperative photographs of protruding ears; it took a rather aggressive surgical approach to the correction of excess skin of the eyelids. Bettman24 was the first to publish preoperative and postoperative facelift photographs and to describe a continuous temporal scalp, preauricular, postauricular, and mastoid area incision. With modifications, his incision is essentially that used for facialplasty today. Hunt25 published a book, Plastic Surgery of the Head, Face and Neck, that included facelifting and forehead/browlifting operations.
All the early facialplasty procedures were limited to skin excision and wound closure without subcutaneous undermining. Bames26 described subcutaneous face and neck undermining, skin redraping, and excision of excess skin. The continuous incision described by Bettman24 and subcutaneous undermining recommended by Bames26 essentially established the basic facelift procedure for the next 40 years. As discussed by Rees,6 a great deal of secrecy surrounded early facelift procedures. Surgeons were reluctant to share their techniques because of professional jealousy and greed. The disdain for “vanity” surgery by both the medical profession and the public restricted most facelift procedures to private offices and small clinics. The extent of surgery in such settings was necessarily limited. Many prominent plastic surgeons in major medical centers were forced to perform their facelifts in small clinics or to hide their cases by misnaming the procedures on the operating schedule. Renowned plastic surgeons after the First and Second World Wars, such as Gillies, Blair, Davis, Pierce, McIndoe, Mowlem, Conway, and others, did a great deal of cosmetic surgery but were reluctant to publish on the subject.6 The conventional facelift operation (skin dissection only) failed to address the effect of aging and the force of gravity on the structures (e.g. muscle, fat, and superficial fascia) deep to the skin. Likewise, the classic skin dissection facialplasty failed to account for the wide variation in facial, jaw line, and cervical deformities; in the location of fat deposits; in the asymmetry of anatomic structures; and in the genetically determined deformities, such as microgenia and the obtuse cervicomental angle.
Aufricht27 discussed the limitations of the subcutaneous facelift, particularly its failure to correct submental fat deposits and platysma bands. Adamson and colleagues28 discussed correction of the platysma bands in the submental area, and Millard and co-workers29 recommended extensive submental defatting. Pennisi and Capozzi30 and Baker and Gordon31 described suture plication of the deep tissues of the cheek and lateral neck. Tipton32 challenged the deep suture techniques in a study of 33 patients in whom he performed unilateral plication. Two years postoperatively, there was no obvious difference in the two sides of the face. Skoog33,34 described a technique of dissection of the superficial fascial layer in the face, in continuity with the platysma muscle in the neck and advancement of the myofascial unit in a cephaloposterior direction. This was the beginning of the modern era in facelifting. Mitz and Peyronie35 used cadaver dissections to define the limits of the superficial musculoaponeurotic system (SMAS) in the face and noted that tightening of this layer would be beneficial in facialplasty. SMAS-platysma facelifting, wide skin undermining, and extensive fat removal soon gained worldwide popularity. Surgery of the tissue layers deep to the skin of the face and neck is now established as an essential part of cervical and facialplasty operations. Many surgeons have described different SMAS-platysma techniques to improve the cervicofacial area and to remedy problems not corrected by conventional facialplasty.36–44 Furnas,45 in 1989, described the retaining ligaments of the midface, which led to a better understanding of anatomic areas where facial soft tissue is supported and the involvement of these ligaments in leading to the anatomic changes that occur with aging. These ligaments were further defined by others46,47 who thought that loss of the support from the retaining ligament system allowed facial fat to descend inferiorly in the face, deepening the nasolabial fold and forming facial jowls with aging. The importance and location of the retaining ligaments led to modifications in procedures involving retaining ligament release in sub-SMAS dissection,47–56 the primary goal of these procedures being to reposition descended facial fat to the anatomic location of youth. Other surgeons, preferring subperiosteal rather than sub-SMAS dissection to reposition fat, developed procedures whose similar goal is to resuspend descended malar fat to the malar eminences using the subperiosteal plane.57–59 A combination of subperiosteal and subcutaneous lifting has also been described.60
Anatomy and patient presentation
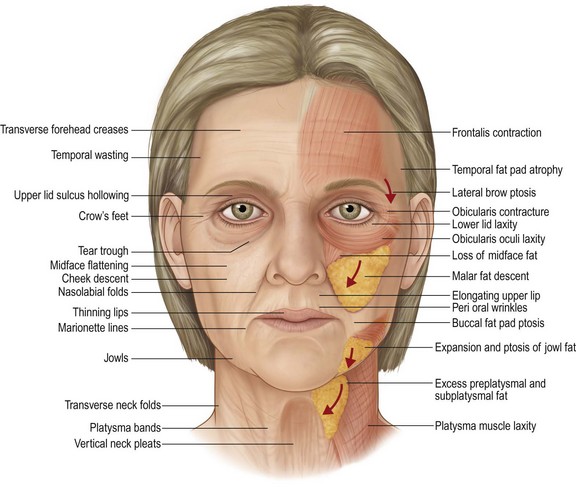
The classic stigmata of the aging face include:
• Visible changes in skin, including folds, wrinkles, dyschromias, dryness and thinning
• Folds in the skin and subcutaneous tissue created by chronic muscle contraction: glabellar frown lines, transverse forehead lines, and crow’s feet over the lateral orbital rim.
• Deepening folds between adjoining anatomic units: the nasojugular fold (tear trough), nasolabial folds, marionette lines and submental crease
• Ptosis of soft tissue, particularly in the lower cheek, jowls and neck
• Loss of volume in the upper two-thirds of the face which creates hollowing of the temple, the lateral cheek and the central cheek. The result is a more skeletal appearance in the temple, the periorbita and the malar region
• Expansion of volume in the neck and lateral jaw line which leads to the formation of jowls and fullness of the neck (Fig. 11.1.1).
The driving force behind our ability to explain these many changes has been an improved understanding of facial anatomy and the way this anatomy changes over time. Aging of the face occurs in all its layers, from skin down to bone; no tissue is spared. For the purposes of this discussion, the face will be viewed as a five-layer structure as described in Chapter 6: skin, subcutaneous fat, the superficial musculoaponeurotic system (SMAS) and muscles of facial expression, fascial spaces, and deep fascia. Underlying everything is bone, except over the oral cavity. The surgical significance of this concentric layer arrangement is that dissection can be done in the planes between the layers. Also, anatomical changes in each of the layers can be addressed independently, as required to treat the presenting problem.
Skin
Normal skin is directly adherent to underlying fat via the retinacular cutis system. In certain predictable areas the skin is tethered to bone or underlying muscle by condensed areas of connective tissue. In some places, these are string-like cutaneous ligaments, and in other areas, these are ribbon-like septae. Because nerves and vessels often reach the skin adjacent to these vertically running fibrous structures, dissection of skin is more difficult and bloody where the skin is tethered; McGregor’s patch is such an area because of its association with the zygomatic cutaneous ligaments and a perforating branch of the transverse facial artery. Changes in the skin of the face are some of the most obvious signs of aging. Skin aging over time is both intrinsic and extrinsic. Intrinsic aging is the result of genetically determined apoptosis. The skin becomes thinner; there is a decrease in melanocytes, a reduced number of fibroblasts and a loss of skin appendages. In the dermal matrix, there is fragmentation of the dermal collagen and impairment of fibroblast function.61,62 As the skin weakens and thins, the underlying contraction of facial muscles creates permanent skin folds in predictable locations (see Fig 11.1.5).
Extrinsic forces include sun exposure, cigarette smoke, extreme temperatures and weight fluctuations. The net result is that facial skin loses its ability to recoil, a condition called elastosis. This has surgical implications, because firm tight skin is youthful, and to varying degrees, the tightening of loose facial skin is part of a good surgical result. However, a facelift does not appreciably improve the quality or texture of the skin. Therefore, patients with good quality skin are likely to enjoy a better result from facelift surgery than the patient with poor quality skin. Alternatively, when skin quality is poor, other options such as injectable fillers and skin resurfacing may be more important for rejuvenation than facelift surgery. In most cases of facial rejuvenation, medical and surgical therapies can work in concert for a more complete result. (These complementary therapies are reviewed in Chapters 4 and 5.)
Facial fat: ptosis, volume loss and volume gain
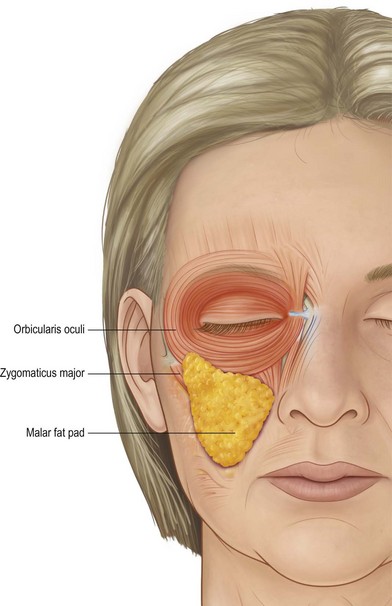
The face is carpeted in a layer of superficial fat which lies immediately deep to the dermis. Between individuals, there is much variability in the thickness of the superficial fat layer. This has surgical implications, because a heavier patient will have thicker, heavier tissues to reposition, but the dissection of the facelift skin flap will be easier. Conversely in a thin patient, facial layers are packed closely together, like an onion, necessitating greater care if the surgeon wishes to separate skin from SMAS and SMAS from underlying structures. Superficial facial fat also varies in thickness depending on the area of the face. The most important area of thickened subcutaneous fat is the malar fat pad.54 This is a triangular shaped mass of fat bordered by the nasolabial fold, the infraorbital arch and a diagonal line across the mid-cheek. Its apex is over the malar eminence. The malar fat pad is present throughout life (Fig. 11.1.2).
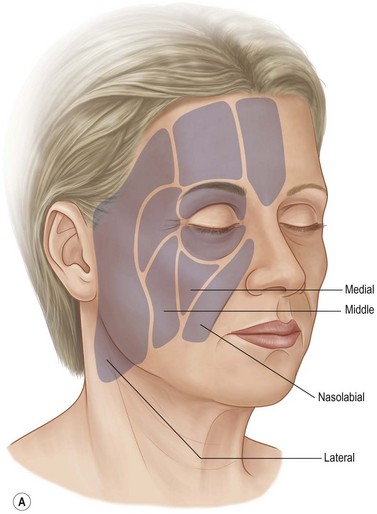
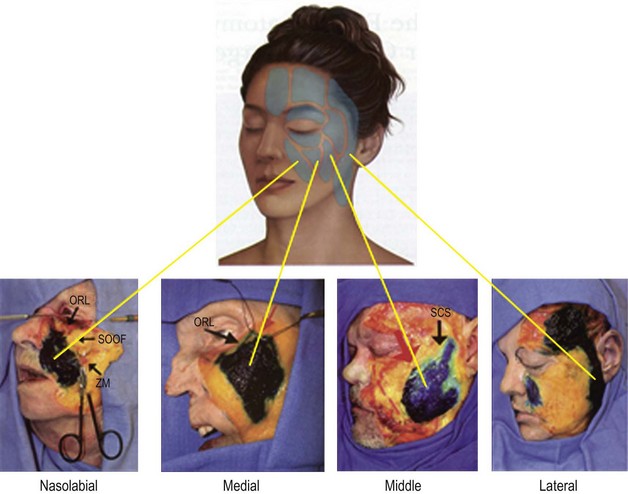
One study looked at fat volume in the cheek area and found 56% of the fat superficial to the SMAS and 44% was deep to the SMAS and the muscles of facial expression.63 The superficial fat is separated by vertical septae into five distinct compartments: nasolabial, medial cheek, middle cheek, lateral temporoparietal, and the inferior orbital fat (Fig. 11.1.3A).64
The deep fat is also divided into compartments (Fig. 11.1.3B). The most significant is the deep medial fat compartment, which lies directly against bone and is bordered above by the orbicularis retaining ligament, laterally by the zygomaticus major and buccal fat pad and medially by the pyriform aperture65 (Fig. 11.1.3C).
The authors who identified this compartment propose that age related deflation of deep medial fat compartment leads to “pseudoptosis” of the overlying superficial fat and skin – ptosis which is real, but which is caused by lack of underlying support.65
This in turn is thought to cause deepening of the nasolabial fold and development of the “inverted V deformity” inferior to the infraorbital rim.66 Adjacent and lateral to the deep medial fat is the suborbicularis oculi fat (SOOF), which itself is divided into a medial and lateral component.
Generally in youth, facial fat is tightly packed, creating surface contours which undulate smoothly from convexity to concavity. Cosmetic highlights rise above areas of depression. The malar fat pad which extends over the body of the zygoma creates the principle cosmetic highlight zone in the youthful face, immediately above the normal depression overlying the buccal recess. Make-up artists accentuate this zone by highlighting the apex and simulating a depression immediately below. In the aging face, fat is less tightly packed, and facial contours become more abrupt. In areas of tight ligamentous attachment, such as the preparotid area, the anterior jowl border and the zygomatic ligament insertions, there appears to be an acceleration of volume loss with indenting of the surface contour.67 With more advanced aging, there is malar fat atrophy, leading to a more skeletal appearance of the zygoma. Simultaneously there is an apparent ptosis of the malar fat pad which causes bunching of fat and deepening of the nasolabial fold. Surgeons have traditionally viewed superficial fat in the cheeks as a ptotic layer which requires correction for facial rejuvenation to occur. In support of this theory, it has been demonstrated that the primary muscles of facial expression in the mid-cheek (zygomaticus major and minor) do not change in length, while the overlying fat appears to migrate inferiorly.68 Another study, using CT scans, confirmed the presence of facial fat compartments and identified age related inferior migration of the midfacial fat compartments as well as inferior volume shift within the individual compartments.68a
At the time of writing, it is unclear whether the cause of superficial fat ptosis is gravitational due to relaxed fixation, or if it relates to pseudoptosis caused by the loss of volume in the deep fat compartments. Also, it is uncertain whether volume of facial fat is lost equally from the deep and superficial fat layers, or if it lost equally or differentially from the various fat compartments which have been identified.65
In the lower face, the area of the jowl just posterior to the marionette lines appears to become thicker with age, making the mandible appear wider. This phenomenon has been called “radial expansion” (Lambros, pers. comm. 1999).69 This may be due to fat accumulation, or it may be caused by soft tissue ptosis within the premasseteric space, a natural glide plane.69a Below the mandible, a similar expansion occurs in the neck as soft tissue falls away from deep tissue attachments and fat tends to accumulate.
Change in facial shape
The loss of facial volume is an important phenomenon which surgeons recognized much later than the more obvious ptosis of soft tissue. To arrive at this conclusion, astute observations were made about changes in surface contours which lead to inferences about internal volume loss.65,67,70,71
The combination of volume loss in some areas, volume gain in others, and soft tissue ptosis creates a cascade effect which results in the loss of natural youthful curves (Fig. 11.1.4).
Gradually, there is a reversal of facial shape as the cheek prominence of youth gives way to the jowl prominence of age. Effectively, in youth, the cheeks are full, but with age, the jowls and neck become full. The face changes from a heart shape to a more rectangular shape, or from an egg sitting on its narrow end to an egg resting on its broad end. This change has been called losing the “inverted cone of youth”, and has been likened to a reversal of the “Ogee” curve, a natural S-shaped curve seen in architecture.60,72
Superficial musculoaponeurotic system
Immediately deep to the subcutaneous fat is the superficial musculoaponeurotic system (SMAS), described by Mitz and Peyronie in 1976.73 The SMAS, or its analogues can be thought of as a continuous fascial sheath which encompasses the entire face and neck. Superiorly, it continues into the temple as the superficial temporal fascia (temporoparietal fascia) and then into the scalp as the galea aponeurotica.74 Inferiorly, into the neck, the SMAS becomes the superficial cervical fascia which envelopes the platysma muscle. Clinically, the thickness and strength of the SMAS varies between patients, and also varies in every individual face, being thicker and adherent over the parotid, and thinner anteriorly. The SMAS is most tenuous under the malar fat pad where it splits to encompass the zygomaticus major and the orbicularis oculi.53,75 The SMAS has important surgical implications because its fibrous attachments to skin allow it to act as a carrier for overlying subcutaneous fat; also it has been shown to be much more resistant to stretch than skin.76 Furthermore, below the zygomatic arch, all branches of the facial nerve are deep to the SMAS.
The relationship of the SMAS (superficial fascia of the face) to the deep fascial structures of the face, involves areas of mobility interspersed between areas of attachment. The superficial fascia is tethered to the deep fascia by retaining ligaments in the following locations: over the parotid gland, at the inferior border of the zygomatic body, and along the anterior edge of the masseter. (These ligaments are described in Chapter 6 and are reviewed later in this chapter.) Between areas of fixation the SMAS is free to move over the underlying deep fascia. These are the suprazygomatic zone where superficial temporal fascia slides over the deep temporal fascia, the mid-cheek, where SMAS rides over the parotid masseteric fascia (premasseteric space), and the neck where the platysma overlies the underlying strap muscles.
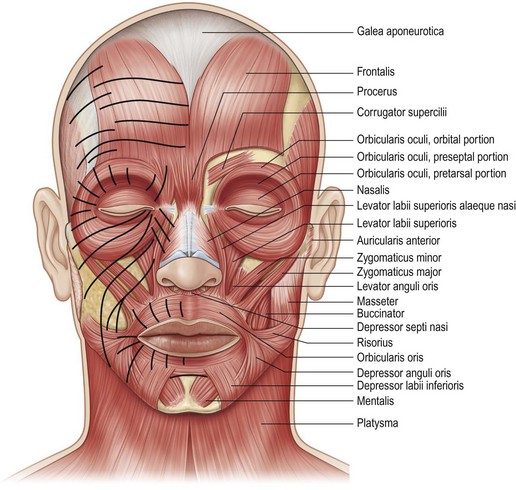
Facial muscles
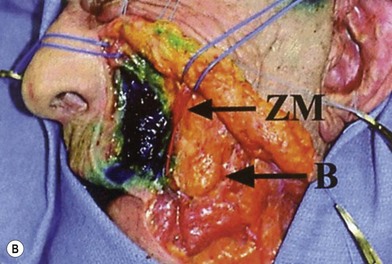
The muscles of facial expression are found in a superficial layer and a deep layer. The superficial muscles are orbicularis oculi, orbicularis oris, zygomaticus major, zygomaticus minor, levator labii superioris, risorius, and depressor anguli oris. All of these muscles are innervated on their deep surface by branches of the facial nerve (VII). Consequently, surgical dissection on the superficial surface of these muscles will not endanger their innervation. The only facial muscles innervated on their superficial surface are the muscles in the deep layer: levator anguli oris, mentalis and buccinator. The three facial muscles which are most important to surgeons are orbicularis oculi and platysma, because they are often manipulated during facelift surgery, and zygomaticus major because it is used as a landmark in certain facelift techniques (Fig. 11.1.5).
While most muscles of facial expression do not change appreciably with age, the orbicularis oculi and the platysma are thought to undergo age-related changes. Both of these muscles have a large surface area but are relatively thin – a configuration which lends them to potential redundancy if they lose tone or if there is attenuation of their deep tissue attachment. For example, in some individuals redundancy develops in the lower half of the orbicularis, a condition which has been speculated to cause lower eyelid festoons.77 Some have suggested that it is the loss of support of the orbicularis through attenuation of the orbicularis retaining ligament (orbitomalar ligament), which contributes to deformities of the lower eyelid/cheek junction.66 Similarly, the paired platysma muscles, which are encased by SMAS, appear to gradually fall away from their deep cervical attachment carrying the overlying fat and skin. The net result is a more obtuse cervico-mental angle and the development of visible platysma bands at the anterior platysmal border. Another issue common to orbicularis oculi and platysma is that these are the only facial muscles which are undermined during certain surgical procedures, thus imperiling some of their motor innervation. Fortunately, the orbicularis has multiple motor nerve branches which provide a level of collateral innervation.78 There is a less elaborate innervation to the platysma; two or three cervical branches can be identified just inferior and anterior to the angle of the mandible in the plane between the deep cervical fascia and the undersurface of the platysma. Preservation of these branches is potentially important because the platysma acts as a support structure and also influences lower lip depression, especially in those individuals with a “full dentition” smile.79
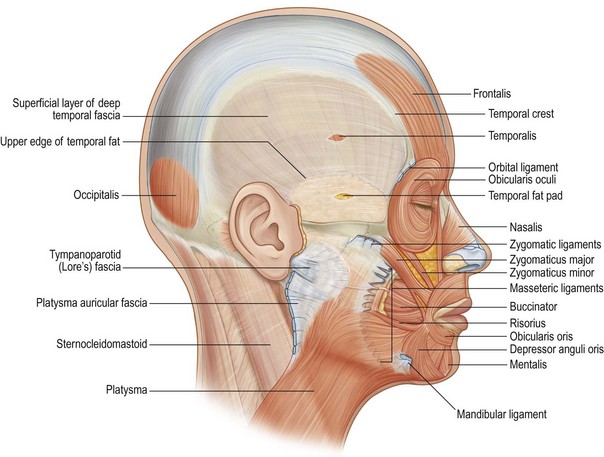
Retaining ligaments
Facial soft tissue and skin is held in place by retaining ligaments which run from underlying fixed structures through facial fat, inserting into the dermis.45,48,80 Effectively, these ligaments attach the superficial fascia (SMAS) and the overlying skin to the underlying deep fascia and bone (Fig. 11.1.6).
There are two ligament systems. The first group is true osteocutaneous ligaments, which tether skin to bone: the orbital, zygomatic and the mandibular ligaments. The orbital ligament is found at the junction of the superior and lateral orbital rims and constitutes the inferior thickening of the temporal crest line zone of fixation (zone of adhesion). (This area is reviewed in Chapter 7.) The zygomatic ligament is actually a group of ligaments which originate from the lower half of the zygomatic body where it joins the zygomatic arch. The zygomaticus major inserts into bone at this location. These ligaments stabilize the overlying malar fat pad, going through this structure to the overlying skin. In this area, a perforating branch of the transverse facial artery courses from deep to superficial, contributing to the clinical bleeding seen when the zygomatic ligaments are released in this area during superficial skin flap dissection (McGregor’s patch). A branch of the zygomaticofacial nerve also accompanies the ligaments in this area, coursing directly from bone to skin providing sensation to the skin of the malar cheek prominence. As described in Chapter 6, the zygomatic ligaments constitute the lower border of the prezygomatic space and must be released if the malar fat pad is to be fully mobilized and elevated. The mandibular ligament is a short but strong structure originating from the parasymphysial mandible, which tethers the overlying skin and contributes to formation of the marionette lines.
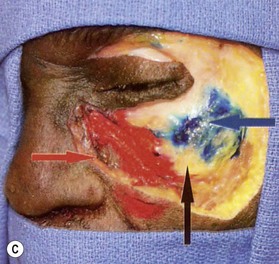
The second ligament system involves tethering structures which do not originate from bone, but rather, tether the superficial fascia (SMAS) to the deep fascia. Along the anterior border of the masseter, the masseteric ligaments extend in a line from the zygoma down to the lower cheek.80 These ligaments support the anterior cheek and are more clinically significant superiorly, where they intermingle with the zygomatic ligaments. The most superior fibers of the platysma can also be seen terminating in the most superior masseteric ligaments. Over the parotid gland with an extension down along the posterior border of the platysma, the superficial fascia is firmly attached to the deep fascia. A number of authors have identified the importance of this area, and with some subtle differences, a number of different names have been applied to the same soft tissue attachment: platysma-auricular fasica,81 platysma-auricular ligament,45 parotid cutaneous ligament,80 and a localized area called Lore’s fascia.82,83 In this zone, the SMAS and the overlying skin are tethered to such a degree that soft tissue in this area does not become ptotic with age. A prime surgical significance is that the “fixed SMAS” of the posterior cheek can be used to support the surgically mobilized portion of the more anterior “mobile SMAS”. A number of facelift techniques depend on this concept (Fig. 11.1.7).
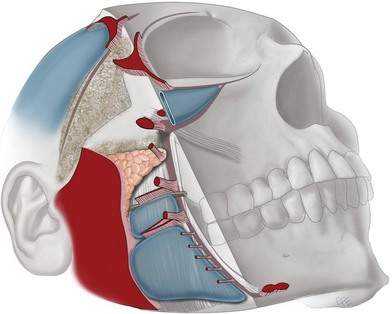
Figure 11.1.7 Mendelson’s interpretation of soft tissue attachments (Ch. 6). The fixed posterior soft tissue is held in place by the platysma auricular fascia (large red area). The anterior face is fixed by a vertical column of attachments: orbital ligament, lateral orbital thickening (superficial canthal tendon), zygomatic ligaments, masseteric ligaments, mandibular ligament). In the mid-cheek, there is some mobility of these ligaments, while there is limited mobility over the platysma auricular fascia. The so-called “fixed SMAS” is that portion attached to the parotid and the posterior border of the platysma. Anterior to this, is the “mobile SMAS”.
(Courtesy of Dr Levent Efe, CMI.)
The importance of retaining ligaments in the aging process is potentially two-fold. One theory holds that with age, ligaments relax, leading to a gravitational shift of overlying superficial fat and skin. In youth, the superficial fat and skin appear to be firmly adherent to underlying bone and deep fascia, while with age the same soft tissue appears to become ptotic. One area where this has been proposed is along the infraorbital rim, where the orbicularis retaining ligament may relax, leading to the V-deformity at the lid cheek junction.66,84–86 Over the malar highlight area, the ligament relaxation theory suggests that the zygomatic ligaments become attenuated and the malar fad pad becomes ptotic, causing a migration of fat medially and inferiorly, deepening the nasolabial fold.
The second way that retaining ligaments become an issue with aging is through their tethering effects. The concept of “pseudoptosis” holds that it is primarily the loss of facial fat volume which leads to ptosis, but the ligaments tether the skin, leading to depressions and grooves in the surface contour of the face. Examples of tethering include: the mid-cheek groove, caused by the zygomatic ligaments, the nasojugular groove, partly caused by the orbicularis retaining ligament (orbitomalar ligament) and the jowl/marionette line caused by the mandibular ligament.81–83,85
Deep fascia
The deepest layer of the face is the deep fascia, which covers deep muscles and overlies the oral cavity (Ch. 6). In the face, this fascia is a continuation of the deep cervical fascia in the neck which covers the superficial surface of the strap muscles and the sternocleidomastoid. The equivalent layer in the temple is the deep temporal fascia covering the temporalis. In the cheek, this fascia is found covering the masseter muscle, where it is called masseteric fascia, and covering the parotid gland, where it is called the parotid fascia or capsule; the combined complex is called the parotid masseteric fascia (parotidomasseteric fascia). When the SMAS is raised surgically, just anterior to the parotid gland in the premasseteric space, the parotid masseteric fascia can be seen as a thin shiny membrane – an important landmark, because in the cheek (unlike the neck and temple), all branches of the facial nerve are deep to this deep fascial layer. Superficial to this layer, but deep to the SMAS, there is often an additional thin layer of fat, the sub – SMAS fat, which adds further protection to the underlying nerves when the SMAS is raised. In the neck along the posterior border of the platysma, the SMAS becomes fused with the deep cervical fascia where the deep fascia covers the sternocleidomastoid muscle. This is important, because a surgeon planning to mobilize a platysma flap to address the neck, will have to release the platysma’s attachment to the deep cervical fascia in this area.87
Bone
The bony skeleton of the face was once thought to be quite stable in volume and shape as the body aged. However, there is ample evidence that atrophy in certain portions of the facial skeleton is a significant factor in facial aging.88–93
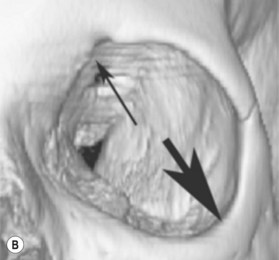
Computed tomography of young and old skulls has shown a retrusion of the infraorbital rim as well as recession of the maxillary face below the infraorbital rim (Fig. 11.1.8).90
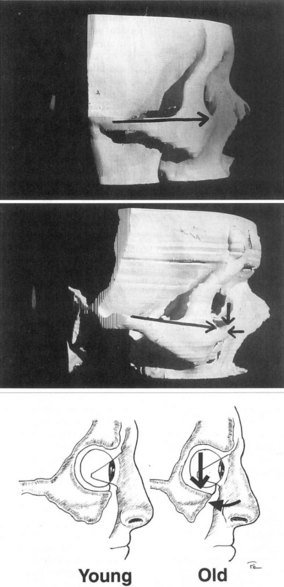
Figure 11.1.8 Computed tomography of young and old skulls has demonstrated a retrusion of the infraorbital rim.
(Courtesy of Pessa JE. An algorithm of facial aging: verification of Lambros’s theory by three-dimensional stereolithography, with reference to the pathogenesis of midfacial aging, scleral show, and the lateral suborbital trough deformity. Plast Reconstr Surg. 2000;106:479.)
This has been confirmed by others who have demonstrated an enlarging orbital aperture (Fig. 11.1.9).94
The loss of bone has surgical implications because it contributes to an overall loss of volume, and more specifically, to loss of soft tissue support in critical areas such as the infraorbital rim. This contributes to development of the tear trough deformity and age related flattening of the anterior midface. Following the principle of replacing like with like, bone loss can be replaced with solid objects such as facial implants (Ch. 15), or with soft tissue volume enhancement such as with fat grafting (Ch. 14).
Nerve anatomy
Facial nerve
In fact, there is considerable variation in the anatomy of facial nerve branches. One study identified up to eight branches exiting the parotid, with multiple connections between these branches.95–97
The temporal branches exit the parotid superiorly, coursing obliquely and superiorly across the middle-third of the zygomatic arch. Like all other facial nerve branches, the temporal branches start out deep to the deep fascia of the mid-cheek (parotid masseteric fascia), but unlike all other facial nerve branches in the cheek, they become more superficial. At a point 1.5–3.0 cm superior to the zygomatic arch, the temporal branches transition from deep to superficial, travelling at first on the undersurface and then within the superficial temporal fascia (temporoparietal fascia), staying there until they terminate in the frontalis muscle, upper orbicularis and frown musculature. The surgical implication is that a SMAS flap can be safely raised from a point just superior to the zygomatic arch providing that surgical dissection does not extend superiorly to the level where the temporal branch transitions superficially.98
A classic external landmark for the course of the temporal branch has been along a line drawn from a point 0.5 cm below the tragus to a point 1.5 cm lateral to the lateral eyebrow.99
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree