30 Cleft and craniofacial orthognathic surgery
Synopsis
 Dentofacial deformities, in particular maxillary retrusion resulting in class III malocclusion, are typical of the cleft lip population. Of patients in this group, 25–30% have midface retrusion severe enough to require orthognathic surgery
Dentofacial deformities, in particular maxillary retrusion resulting in class III malocclusion, are typical of the cleft lip population. Of patients in this group, 25–30% have midface retrusion severe enough to require orthognathic surgery
 Orthognathic surgery should ideally be performed after facial growth is complete. If surgery is performed earlier, the likelihood is high that additional (though possibly less complicated) surgery may be required when the patient reaches skeletal maturity
Orthognathic surgery should ideally be performed after facial growth is complete. If surgery is performed earlier, the likelihood is high that additional (though possibly less complicated) surgery may be required when the patient reaches skeletal maturity
 Treatment should favor expansive movements (anterior and inferior repositioning) to achieve class I occlusion rather than contractile movements (superior and posterior repositioning) in order to minimize premature aging.
Treatment should favor expansive movements (anterior and inferior repositioning) to achieve class I occlusion rather than contractile movements (superior and posterior repositioning) in order to minimize premature aging.
Introduction
Orthognathic surgery is the term used to describe surgical movement of the tooth-bearing segments of the maxilla and mandible. Candidates for orthognathic surgery have dentofacial deformities that cannot be adequately treated with orthodontic therapy alone. Children with cleft lip and palate as well as certain craniofacial anomalies are especially prone to develop malocclusion. Indeed, where approximately 2.5% of the general population have occlusal discrepancies that warrant surgical correction, 25–30% of patients who undergo surgical correction of cleft lip and palate in infancy will have severe enough midface retrusion to require orthognathic surery.1 Maxillary hypoplasia resulting in class III malocclusion is the typical deformity seen in patients with cleft and craniofacial deformities, but class II malocclusion, anterior open bites, occlusal cants and many other dentofacial deformities can also occur. Regardless of the etiology, patient examination and treatment-planning principles remain the same. The goal of orthognathic surgery, therefore, is to establish ideal dental occlusion with the jaws in a position that optimizes facial form and function.
Historical perspectives
Much has changed since those early surgeries. Perhaps the greatest impact to the field was brought about by Hugo Obwegeser, an Austrian-born dentist who is credited with modernizing the field of orthognathic surgery and introducing it to the US. Amongst his credits, the sagittal split osteotomy for mandibular advancement and the intraoral approach to the osseus genioplasty clearly advanced lower-jaw surgery. But it was not until 1965, when Obwegeser2 demonstrated that the maxilla could be completely mobilized in one procedure and reliably and stably repositioned, that modern orthognathic surgery gained widespread appeal.
Basic science
Growth and development
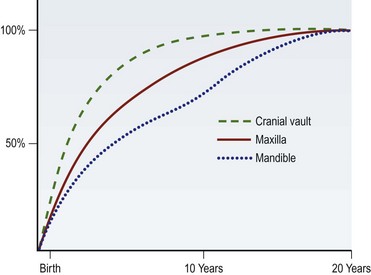
The osteogenesis of the maxillofacial skeleton occurs by way of two well-understood processes: intramembranous ossification and endochondral ossification. The cranial vault, upper face, midface, and a majority of the mandible arise from the former mechanism. Although there is a great amount of variability between individuals and genders, skeletal maturation generally progresses in a cranial-to-caudal direction with the cranial vault reaching close to adult size in early adolescence, followed closely by the upper face in the early teen years, the maxilla in the mid-teens, and the mandible in the late teen years (Fig. 30.1).3
Dental eruption patterns proceed in a similar stepwise fashion, and the transition from mixed dentition (6–12 years of age) to permanent dentition (12–20 years of age) mirrors the maturation of the maxillofacial skeleton. Indeed, midface and lower face development is, in part, mediated by the budding deciduous and permanent dentition, providing regional signals to the alveolus and stimulating bony deposition. During this period, an alteration of tooth position can, in turn, alter the direction of growth of both the maxilla and mandible. Orthodontists take advantage of this active phase of development through their use of braces, palatal expanders, and various external devices to alter maxillary and mandibular growth trajectories.4 For this reason, surgical intervention is usually delayed until skeletal maturity is reached and orthopedic movements are no longer effective.
Diagnosis/patient preparation
Preoperative evaluation
The history and physical examination
If the patient desires surgical correction of the deformity, presurgical orthodondics will upright and decompensate the occlusion, thereby reversing the compensation that has occurred. This has the effect of exaggerating the malocclusion, but it also allows the surgeon to maximize skeletal movements. If the patient is ambivalent or not interested in surgery, mild cases of malocclusion may be treated by further dental compensation, which will camouflage the deformity and restore proper overjet and overbite. The importance of a commitment to surgery prior to orthodontics lies in the fact that dental movements for decompensation and compensation are in opposite directions, so this decision needs to be made prior to orthodontic therapy.5
Patient selection
Cephalometric and dental evaluation
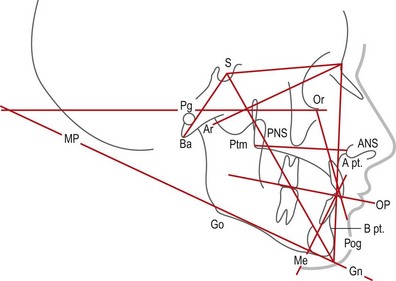
A cephalometric analysis and comparison to normative values can help the surgeon plan the degree of skeletal movement needed to achieve both an optimal occlusion and an optimal aesthetic result. A lateral cephalometric radiograph is performed under reproducible conditions so that serial images can be compared. This film is usually taken at the orthodontist’s office using a cephalostat, an apparatus specifically designed for this purpose, and a head frame to maintain consistent head position. It is important to be certain the surgeon can visualize both the bony and soft-tissue features in order to facilitate tracing every landmark. Once the normal structures are traced, several planes and angles are determined (Fig. 30.2).
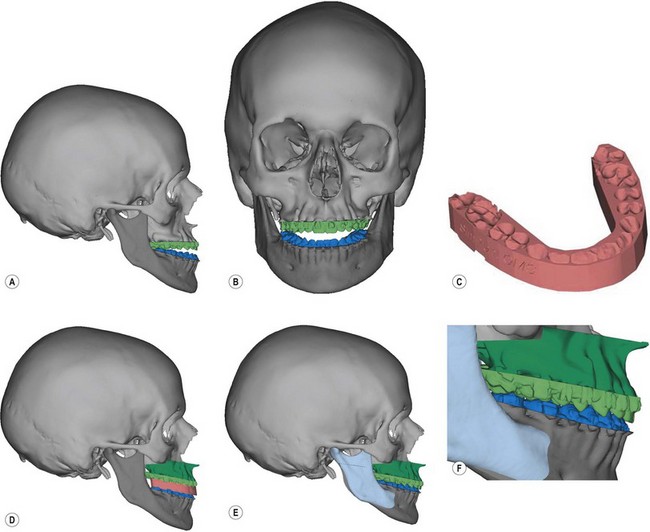
3D CT modeling
There are several computer-assisted design (CAD) programs that are now commercially available that can assist the surgeon with some or all of the preoperative patient preparation. A computed tomography (CT) scan is obtained with the patient wearing a bite jig that correlates natural head position to the three-dimensional (3D) CT image of the patient’s face. Although conventional helical CT scans with fine cuts through the face are ideal, cone beam CT scans offer a comparable image quality with considerably less cost and radiation exposure (50 µSv compared to 2000 µSv). A cephalometric analysis can then be performed as well as simulated movements of the jaws and chin in any dimension. Once the osteotomy movements are verified by the surgeon, CAD/CAM technology is used to fabricate surgical splints for the patient. If necessary, 3D models of the patient can be made showing the exact proposed movement (Fig. 30.3). Some systems can actually “wrap” a 2D digital image around the soft-tissue envelope of the 3D CT image, thus replicating a 3D image of the patient’s face in color.