4 TMJ dysfunction and obstructive sleep apnea
Synopsis
 Tomography and magnetic resonance imaging (MRI) are used to evaluate the patient with temporomandibular joint (TMJ) pain if physical exam demonstrates limitation of movement.
Tomography and magnetic resonance imaging (MRI) are used to evaluate the patient with temporomandibular joint (TMJ) pain if physical exam demonstrates limitation of movement.
 Occlusal splinting is the mainstay of management of patients with TMJ myofascial pain without abnormality of the joint.
Occlusal splinting is the mainstay of management of patients with TMJ myofascial pain without abnormality of the joint.
 Surgical treatment of TMJ dysfunction often begins with arthroscopy, which allows joint examination, biopsy, and lavage.
Surgical treatment of TMJ dysfunction often begins with arthroscopy, which allows joint examination, biopsy, and lavage.
 Diagnosis of obstructive sleep apnea (OSA) requires review of subjective symptoms and objective data, including polysomnogram (PSG).
Diagnosis of obstructive sleep apnea (OSA) requires review of subjective symptoms and objective data, including polysomnogram (PSG).
 Surgical management of OSA consists of several phases based on the severity and location of anatomical obstruction.
Surgical management of OSA consists of several phases based on the severity and location of anatomical obstruction.
 The last phase of surgical management consists of maxillomandibular advancement (MMA) by a LeFort I osteotomy and bilateral sagittal split osteotomy of the mandible. The success of this procedure has resulted in its increased use as the primary surgical management of OSA patients.
The last phase of surgical management consists of maxillomandibular advancement (MMA) by a LeFort I osteotomy and bilateral sagittal split osteotomy of the mandible. The success of this procedure has resulted in its increased use as the primary surgical management of OSA patients.
Temporomandibular joint dysfunction
Key points
• Temporomandibular pain may result from masticatory dysfunction, pain syndromes, or internal derangement of the joint.
• History and physical examination identify those individuals who require imaging work-up.
• Diet modification, nonsteroidal therapy, and occlusal splints are the first line of treatment.
• Surgical treatment is directed toward the underlying cause of joint derangement.
The prevalence of TMJ and muscle disorder-type pain in a recent survey of over 30 000 Americans was 4.6%.1 Numerous studies have suggested an association of pain with gender, age, socioeconomic factors, or previous dental and orthodontic interventions. Persons with TMJ disorders can suffer from displacement of the articular disc, termed “internal derangement” of the TMJ.2 However similar symptoms of pain and functional limitations of mouth opening may result from myofascial pain syndromes, congenital disorders, inflammatory conditions, and trauma. Medical and occlusal therapies control symptoms for many patients. For those who require surgical intervention, treatment options range from arthroscopy to joint replacement. An understanding of the normal function of the TMJ and the pathophysiology of its degenerative disorders are key to directing treatment.
Historical perspective
The first description of TMJ disc repair was in 1887 by Thomas Annandale. He reported the treatment of two patients with clicking jaws by disc repositioning. He wrote that tearing or stretching of the tissues connected to the articular cartilage resulted in its displacement.3 Annandale utilized an incision over the joint. Reports from the early 1900s describe L-shaped incisions located both above and below the zygomatic arch.4,5
The term “snapping jaw” was applied for several decades, with no consensus on its etiology, to painful popping jaws that became stuck in one position. Controversy existed as to whether disc displacement or joint subluxation produced the condition. The direction of disc displacement was also debated. As a result, many procedures were described. Proponents of joint subluxation performed procedures to tighten the joint capsule and limit jaw movement,6,7 while others performed discectomy and repair of ligaments.5,8
In 1936, Costen reported in the Journal of the American Medical Association9 on a series of patients with headache, ear pain, neuralgia, and complaints of abnormal jaw movements. He theorized that pressure exerted through posterior occlusion led to pressure on the TMJ and subsequent destruction and nerve compression. The theory was widely accepted and “snapping jaw” was known for several years as “Costen’s syndrome.” The treatment advocated was dental in nature to open the posterior occlusion. Laskin also shifted the emphasis away from the joint in what he termed myofascial pain syndrome. He associated the masticatory muscle dysfunction with the observed psychological symptoms accompanying the jaw condition.
Ankyloses treatment furthered the development of TMJ surgery. The early descriptions of arthroplasty and interposition of autologous and alloplastic materials were in the treatment of ankyloses.4,10
With the descriptions of TMJ function and pathology offered by Farrar and McCarty2 and Dolwick et al.,11 interest was renewed in joint surgery. Athroscopy of the TMJ had appeared in the Japanese literature in 1975.12 After publication in the English literature in 1986,13 it was readily adopted as a technique in North America. The development of alloplastic joint replacement for TMJ has paralleled that of joint replacement and osseointegrated implants in other fields with the adoption of titanium alloys and computed tomography (CT)-aided fabrication and surgical planning.
Basic science/disease process
Anatomy
The articular disc is a dense fibrous connective tissue structure that separates the joint into two spaces.14 The upper joint space volume of 1 mL extends from the glenoid fossa to the articular eminence. The lower joint space volume of 0.5 mL begins above the insertion of the lateral pterygoid muscle anteriorly and then spreads out over the condyle. The articular disc is an avascular, noninnervated fibrous sheet with some cartilaginous component. The pars gracilis is the thin central zone. The anterior band or pes meniscus is superiorly attached to the articular eminence and superior belly of the lateral pterygoid. Inferiorly, the anterior band attaches to the condyle by a synovial membrane along the attachment of the lateral pterygoid muscle. The posterior band is highly innervated and vascularized tissue, a bilaminar zone or retromeniscal pad. The upper layer of the bilaminar zone attaches to the tympanic plate of the temporal bone, while the lower runs from the posterior meniscus to the neck of the condyle. The disc is not attached to the capsule laterally or medially, but instead bound to the medial and lateral poles of the mandibular condyle.
The retromeniscal or retrodiscal pad is believed to be the origin of pain in TMJ dysfunction. If there are abnormal loading forces on the joint surfaces as a result of disc disease, this can lead to TMJ disorders.15 The fibrous joint capsule attaches to the condyle inferiorly and the zygomatic arch superiorly. It is reinforced anteriorly and laterally by the temporomandibular ligament. The auriculotemporal, masseteric, and deep temporal branches of the trigeminal nerve supply innervation to the TMJ.16
Myofascial problems
The cause of myofascial pain and dysfunction (MPD) is usually related to the masticatory muscles. MPD was first described by Laskin17,18 and is characterized by a limited range of motion, aching pain, and severe tenderness on palpation of the muscles. Certain trigger points within the masticatory muscles refer the pain. The masseter muscle, producing an ache in the jaw, is the most common. Next most common is pain in the temporalis muscle, producing pain in the side of the head. The lateral pterygoid muscle can generate an earache or pain behind the eye. Medial pterygoid involvement causes pain on swallowing or stuffiness in the ear.
Inflammation
Osteoarthritis
Osteoarthritis is a chronic disease that characteristically affects the articular cartilage of synovial joints and is associated with remodeling of the underlying subchondral bone and the development of a secondary synovitis. It is the most common disease affecting the TMJ. It has a gradual onset. Usually, only one side is affected. Radiographically, sclerosis of the subchondral bone, osteophytic lipping, cyst formation, flattening of the condyle, and decreased height of the ramus are observed19 (Fig. 4.1). Chronic anterior disc displacement is associated with posterior–superior condylar resorption, seen as flattening and loss of bone in this area. An open bite deformity and mandibular retrusion may result. Treatment frequently involves drug therapy, occlusal appliance therapy, physical therapy, and, when most severe, surgery.
Rheumatoid arthritis
Rheumatoid arthritis is a chronic inflammatory disease that primarily affects the periarticular structures, such as the synovial membrane, capsule, tendons, and ligaments. More than 50% of rheumatoid arthritis patients have involvement of the TMJ during the course of their disease.20
Progression of the disease includes condylar resorption and fibrous and bony ankylosis. The classic malocclusion is caused by loss of the height of the condyles. Juvenile rheumatoid arthritis affects patients before the age of 16 years. Up to 40% of children with juvenile rheumatoid arthritis have involvement of the TMJ.21 Defective development of the mandible leads to micrognathia. MRI can delineate disc destruction, condylar bone erosion, and cartilaginous thinning. The radiographs of the TMJ include loss of joint space and condylar resorption with anterior subluxation of the condyle.
Condylar problems
Condylar fractures are discussed extensively in Chapter 2. A history of condylar fractures can lead to subsequent pain and limitation of the TMJ.
Idiopathic condylar resorption can also occur in either juvenile or adult individuals. In both forms there is a diminished condylar head. In the juvenile form the exact cause is unknown and is multifactorial but leads to decreased mandibular growth and a class II malocclusion. The adult can follow orthognathic surgery to the mandible or disc displacement. Both types are self-limiting and are treated conservatively until the condition stabilizes. Surgery may then be indicated.22,23
Internal derangement
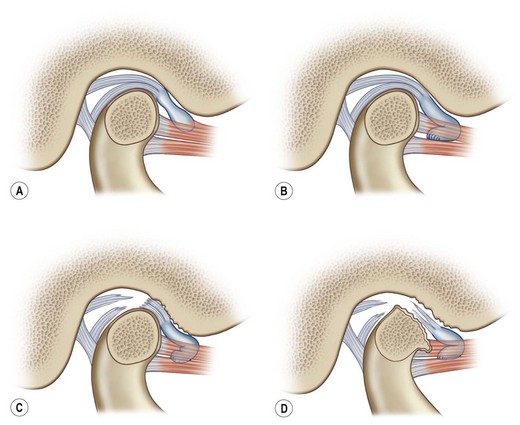
Wilkes established five stages of internal derangement based on clinical and imaging criteria.24 In patients with early stage I derangement, the patient complains of clicking in opening and closing of the jaw (Fig. 4.2). On imaging, the disc is slightly displaced forward on opening, but it is “reduced,” or returns to its normal position, at maximal opening. The oral excursion and lateral movements of the jaw should be within the normal range. The audible clicking sound is produced by reduction of the disc.
Chronic internal derangement without disc reduction (stage IV) results in injury to the retrodiscal tissue. Pain may diminish because of fibrous changes occurring in the retrodiscal tissue.25 Limited mouth opening is common here as the disc blocks full condylar translation. In stage V, remodeling of the temporal and condylar bone components occurs. This final common pathway of cartilage destruction and bone remodeling is shared with other conditions such as osteoarthritis. Yet there are few long-term longitudinal data to indicate the progression of disc displacement. A reducing disc disorder may be stable for years.26
Diagnosis
Diagnostic imaging
Tomography provides sectional images in the sagittal or coronal views, usually taken in the open and closed positions. This modality demonstrates bone pathology and range of condylar motion but provides no information on soft-tissue disease. One study showed that up to 85% with TMJ disease patients had normal tomography.27
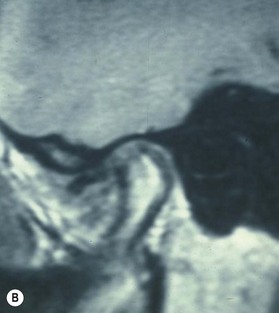
The evaluation of the TMJ soft tissue and disc was traditionally with contrast arthrography. Arthrography can be performed either as single-contrast lower compartment2 or as dual-space contrast arthrotomography.28 The information from TMJ arthrography is highly reliable in determining disc disease but has been replaced by the noninvasive modality MRI. It can also give information about the swelling and inflammation in the joint. In sagittal images, the disc is located anteriorly to the condyle in the closed-mouth position (Figs 4.3 and 4.4). Several MRI studies of adults have demonstrated disc displacement in 20–30% of asymptomatic volunteers;29 however the type of disc displacement may be different. Affected patients with disc displacement demonstrated largely complete anterior or complete anterolateral displacement. MRI may also provide insight into the bone marrow abnormalities of the condyle. If the central area of the condyle has a low signal, this may suggest a pathologic condyle consistent with avascular necrosis.
Treatment
Noninvasive management
The goal of medical management is to break the cycle of pain and anxiety of myofascial dysfunction. Nonsteroidal anti-inflammatory agents are combined with a soft diet. Muscle relaxants, antidepressants, and local anesthetics for diagnostic blocks are adjunctive measures.30 Recently the use of botulinum toxin in areas of muscle spasm has been reported.31,32 The use of oral corticosteroids is effective for acute pain, but prolonged use will lead to osteoporosis, including of the TMJ. Intra-articular injections of corticosteroids are also effective for acute pain management and diagnosis, but repeated injections risk the destruction of articular cartilage. Physical therapy using modalities of heat, massage, ultrasound, transcutaneous electrical nerve stimulation, and biofeedback may also help in these patients.
Occlusal splints reduce the loading of the joint, muscle hyperactivity, and articular strain due to bruxism. The ease of insertion of the appliance and compliance of the patient affect the success of occlusal therapy. The various types of splints include the muscle relation appliance, anterior bite plate, pivot splint, and the soft appliance. Appliance therapy remains a common treatment of TMJ pain, though a review of studies has shown no definite benefit for its use, or for a specific type of splint.33
Surgical management
Arthrocentesis and arthroscopy enable the surgeon to perform endoscopic joint examination, biopsy, and lavage. In addition to the arthroscope (1.8–2.6 mm in diameter), a high-intensity light source, video camera, and monitor are required. Measured landmarks for TMJ entry have been reported.34 The point of entry is along a line from the tragus to the lateral canthus of the eye. The site is 10 mm anterior to the tragus and 2 mm inferior to the line. Using these landmarks will help to prevent complications involving the temporal branch of the facial nerve and the auriculotemporal branch of the trigeminal nerve. A needle is inserted at the posterior entry point to insufflate the TMJ with Ringer’s lactate. After the superior compartment of the joint is distended, the arthroscope is gained through the same entry, or the single-portal technique (Fig. 4.5)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree