Aesthetic canthal suspension can be an effective adjunct to lower eyelid blepharoplasty. Understanding the anatomy and function of the lateral canthal tendon is critical for preoperative evaluation and surgical decision making. In this article, the authors discuss the lateral canthal terminology, anatomy, and aging changes. Various canthal suspension procedures, including open and closed canthal suspension, commissure sparing open canthoplasty, and canthopexy, are described. Finally, the preoperative evaluation, postoperative course, and complications of surgery are reviewed.
Key points
- •
Canthal suspension can be an important adjunct to lower blepharoplasty surgery.
- •
Understanding canthal anatomy, nomenclature, and function is an essential element of surgical success.
- •
The correct canthal suspension procedure selected depends on preoperative findings and the nature of the blepharoplasty procedure performed.
- •
A canthoplasty is a more complex and powerful procedure, which often leads to more patient complaints than canthopexy.
- •
Aesthetic canthal suspension surgery has evolved into less invasive procedures, which tend to preserve canthal anatomy and integrity.
Introduction/philosophy
Aesthetic canthal suspension (CS) is an often challenging stand-alone or adjunctive surgical procedure for the facial cosmetic surgeon. The authors believe this is because the procedure, and its variants, receives far too little detailed attention during surgical education (unless subspecialty trained), and because the literature is inconsistent in descriptions of canthal anatomy, nomenclature, and surgical interventions. , This weakness of surgical education makes operating in this very delicate area of the eyelid cumbersome and intimidating to many. The best way to develop a comfort with canthal surgery is to start at the beginning and attain a detailed and systematic understanding of these aspects of surgery.
Initial descriptions of aesthetic CS surgery surfaced in the 1960s as a means of suspending the lower eyelid as an adjunct to lower blepharoplasty. At the time, this surgery was almost exclusively performed via an open transcutaneous approach. , Postblepharoplasty lower eyelid retraction (PBLER) was, and still can be, a devastating complication of surgery. One of the primary etiologic factors predisposing to PBLER after lower blepharoplasty is unaddressed lower eyelid laxity. , , , , Because PBLER is a complex revisional procedure and, even in the best and most experienced of hands, often leads to ongoing functional and aesthetic issues and low patient satisfaction, CS has become an important adjunct to aesthetic lower blepharoplasty. ,
Some of the early accepted CS procedures involved complete disarticulation of the canthus, plus-minus eyelid shortening, with subsequent canthal reconstruction. , , , These interventions reliably aid in addressing age-related, posttraumatic, and other forms of acquired functional lower eyelid malposition. However, whenever the canthus is “taken apart,” modified, and reconstructed, it is never the same. , , The way the canthus looks, feels, and functions is usually altered. , , In functional surgery, patient complaints related to these changes are typically buried in their satisfaction with eyelid repair as their primary problem is resolved. In aesthetic interventions, where the drive for surgery is appearance and well-being, adding a potential canthal compliant to surgery is hazardous, at best, to the surgeon. For example, the patient with an acquired involutional ectropion or entropion who needs such a procedure to relieve symptoms will often forgive a postoperative change in lower lid slant, canthal height disparity, or a minor canthal web. This is not true of the patient seeking cosmetic lower blepharoplasty. When canthal integrity is altered negatively in aesthetic surgery, an elective procedure can lead to functional and cosmetic impairment, which is not an acceptable outcome. This thinking fueled the development of various modifications of canthal surgery, which have evolved into more sophisticated and less-invasive procedures, which are less disruptive of canthal anatomy, and which often access of the canthus through smaller incisions and via distant sites. , , , The sole purpose of these modifications is to preserve canthal structure and function as much as possible to reduce the incidence of patient complaints and postoperative complications. This is where the challenge of aesthetic CS surgery surfaces. There is a delicate balance between preserving canthal architecture while performing a procedure that meets the task of supporting the lower eyelid adequately. The aesthetic eyelid surgeon must understand this and evolve in their palate of CS techniques to have success with lower blepharoplasty surgery. , , ,
It should also be noted that good CS surgery is not about a belt-and-suspenders tightening of the lower eyelid. , This is an antiquated view of surgery, which unfortunately is still pervasive today. Eyelid malposition after lower blepharoplasty is more related to poor patient evaluation and selection, and to how the skin, muscle, and fat of the lower lid are addressed, than to the CS procedure performed. No CS procedure can overcome poorly planned and performed blepharoplasty. , , Contemporary thought on CS surgery is that it is about creating a physiologic and tension-free degree of lower eyelid support, which acts to re-create a normal canthal angle. It is not about pulling tighter; rather, it is about support and maintaining appearance and integrity. This concept is the first and most basic concept to understand to yield reliable, consistent, and generally complication-free outcomes with aesthetic CS surgery.
In this article, the authors guide the reader through their perspective on canthal terminology, anatomy, aging changes, procedure variants, preoperative evaluation, postoperative course, and complications of surgery. Although this is just 1 view, the authors have found it to be very predictive of good surgical results.
Canthal anatomy/function
The lateral canthal tendon (LCT) is a fibrous continuation of the terminal pretarsal and preseptal (palpebral) orbicularis fibers, which attach to the lateral orbital rim. , , , There is an upper and lower lid contribution to the tendon, the upper crus and the lower crus, which are collectively called crura. The LCT is approximately 1 mm thick, 3 mm wide, and 7 mm in length. It is a 3-dimensional structure with both horizontal and vertical components. Horizontally, it has both an anterior and a posterior component, which attaches to the lateral orbital rim. The most critical attachment is 3 mm posterior to the lateral orbital rim at the Whitnall tubercle, which sits approximately 10 mm below the frontozygomatic suture ( Fig. 1 A). , , This posterior horizontal attachment maintains eyelid apposition to the globe and must be re-created surgically to prevent both eyelid and ocular surface deficits. It is also attached anteriorly to the orbital rim to provide a degree of structural integrity to the tendon. The significance of this insertion is far less than the more critical posterior attachment. Vertically, the LCT sits 2 mm higher than the medial canthal tendon, giving rise to the normal canthal tilt. , If this slant is altered during CS surgery, patient satisfaction is reduced significantly.
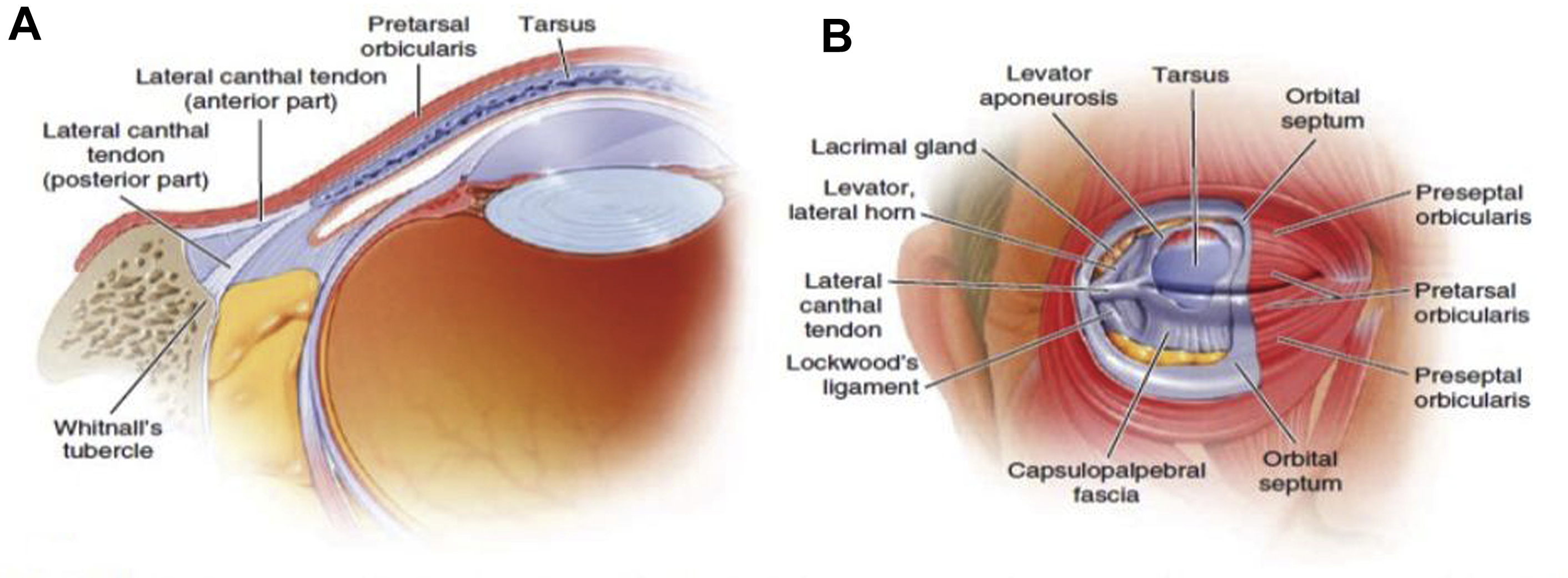
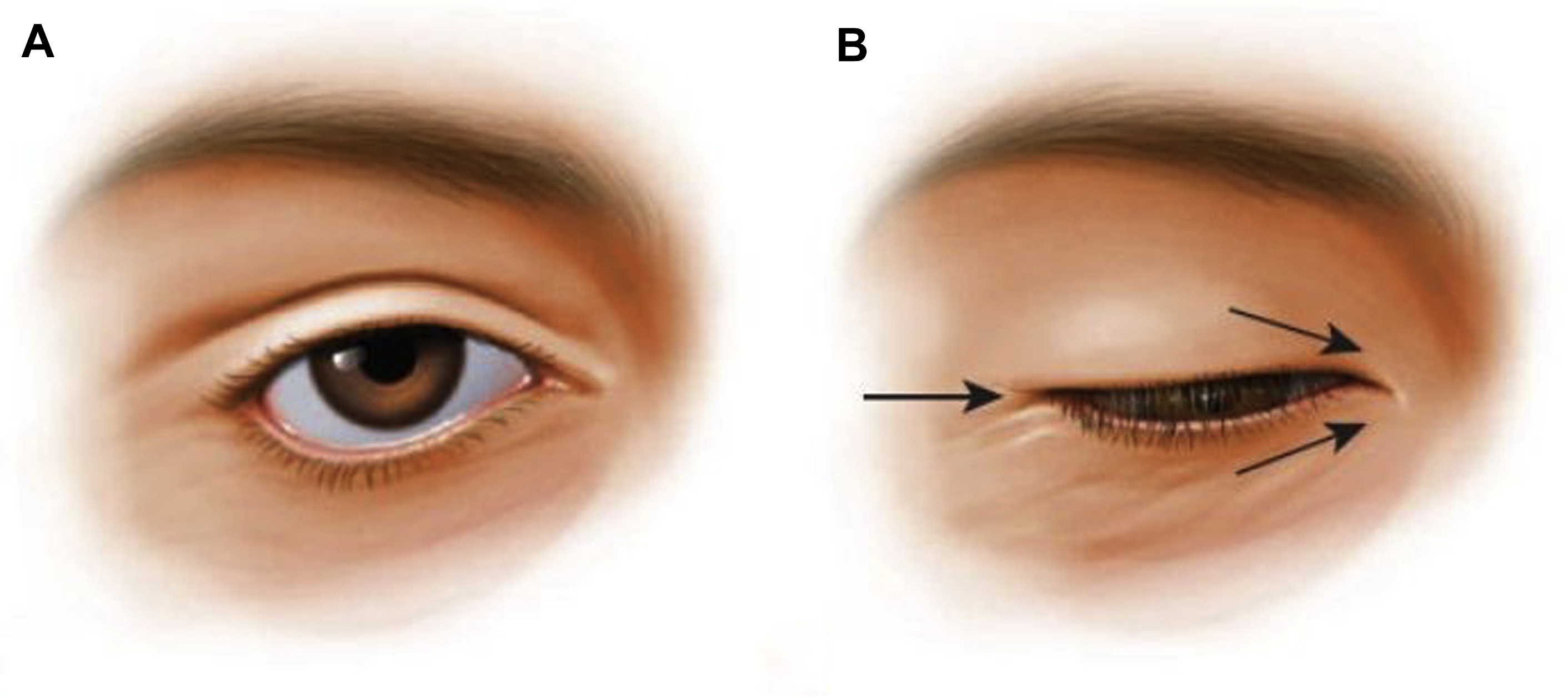
Traditional thinking is that the LCT solely provides support to the lower eyelid to maintain its position after surgery. This thought pattern is flawed, which underscores the many facets of this very complicated anatomic structure. The LCT plays a role in upper (not just lower) eyelid position, as it is associated with the orbital septum and the lateral horn of the levator aponeurosis ( Fig. 1 B). , , If these structures are imbricated during CS surgery, temporary or permanent ptosis can occur. Similarly, this can occur if the upper crus of the tendon is inadvertently “tucked” in surgery. The tendon plays some role in ocular motility, as the check ligament of the lateral rectus is closely associated with it, leading to a few millimeters of lateral movement of the canthus with globe abduction. , , , There is also a fat pad (Eisler fat pad), which is thought to be distinct from orbital/eyelid fat pads and rests in a pocket between the lateral horn of the aponeurosis and the LCT. Its exact function is unknown. The authors believe it may play a role in smooth movement of the aponeurosis over the tendon. Finally, the tendon is an active part of normal eyelid closure. The orbicularis muscle, or eyelid protractor, functions as a sphincter as it passes circumferentially around the eyelid aperture. For normal eyelid closure to occur, the muscle must be anchored medial and lateral by the canthal tendons. When the LCT dehisces or is anchored poorly, eyelid closure changes from a strong and primary vertical excursion (ie, up and down) to one that is weaker with medialization of the lateral canthus with each attempt at closure. This has been referred to as “fishmouthing” ( Fig. 2 ) and is presumed to reduce the biomechanical function of the orbicularis sphincter. As such, eyelid closure is deficient. Each described aspect/function of the LCT can be altered by CS surgery, and modern CS should primarily be founded on an understanding of this. Therefore, in the setting of aesthetic canthal surgery, when the correct blepharoplasty procedure is performed (of primary importance), less manipulation of the canthus is prudent and typically enough.
Canthal aging changes
As with all areas of the face, senescence imparts functional, physiologic, and aesthetic alterations of normal anatomy. It is now widely accepted that tissue loss (both bone and fat) plays at least an equal role in facial/eyelid aging as does tissue descent. Although historically great awareness has been placed on general facial aging changes as a whole, and on specific facial areas, such as the forehead/eyebrows, eyelids, nose, midface, and neck, little such attention has been placed on lateral canthal aging changes. However, an understanding of these changes is an essential component of mastering CS surgery. With age, the palpebral aperture changes from one that is horizontally oval (wider in that plane) to one that is rounder as the canthus migrates medially. This process is a multifactorial process related to loss of integrity (laxity) of the LCT, , , loss of orbital bone in specific areas, , loss of orbital fat (involutional enophthalmos), and most likely changes in suspensory support of the globe. All these changes collectively affect the canthus, and it’s many functions previously stated. This in part explains why more aggressive canthal manipulations can lead to a variety of canthal symptoms/complaints, even in the face of what appears to be excellent surgery.
Canthal terminology
One of the most confusing aspects of canthal surgery is deciphering the many names given to canthal structures and procedures. , For simplicity, the authors will designate all canthal “tightening” procedures as a form of CS. This can further be subdivided into both open and closed variants of surgery, and then into either a canthoplasty or canthopexy. Open canthal surgery involves a canthotomy (canthal incision) to suspends the lower lid, , , whereas closed surgery does not. , , Open surgery provides direct access and anatomic visibility to critical canthal structures and allows precision of lower lid placement. The tradeoff is that it can predispose to canthal deformity and malalignment. Conversely, in closed canthal surgery, canthal entry is from a distant site (ie, temporal upper lid crease), which can limit anatomic exposure and precision of lid placement. It does, however, more favorably preserve canthal anatomy and integrity, mitigating the chances of postoperative canthal deformity. Finally, in a canthoplasty, the LCT or terminal lower lid is cut plus-minus shortened and secured to the lateral orbital rim periosteum. , Alternatively, in a canthopexy, these lid structures are not modified, but rather the LCT or terminal lateral orbicularis muscle is secured to the lateral orbital rim with a plication suture. , Both canthoplasty and canthopexy can be performed in an open or closed fashion, with the canthoplasty variant being the more powerful and complicated procedure, which is fraught with more potential complication.
In relation to anatomic terminology, the lateral canthus is the general area where the lateral upper and lower lids meet, the commissure is their point of union, and the lateral raphe is the union of the upper and lower orbicularis fibers at and beyond the canthus. , The LCT is the connective tissue structure that connects the eyelids to the lateral orbital rim. It has also been called the lateral palpebral ligament. The lateral retinaculum is also used to describe the LCT. A retinaculum is a band around tendons to hold them in place. Because the LCT has an association with numerous other and integral canthal components, including the orbital septum, the check ligament of the lateral rectus, and lateral horn of the levator aponeurosis, the combination of these structures can be considered a structural retinaculum ( Table 1 ).
| Nomenclature | Definition |
|---|---|
| Open canthal suspension | Requires a canthal incision (canthotomy) to access the canthal tendon or terminal tarsus |
| Closed canthal suspension | The LCT is accessed through a distant site. The tendon can be modified and suspended, but it is done so without a canthotomy |
| Canthoplasty | The temporal lower lid is modified and/or shortened and secured to the lateral orbital rim, with or without surgery on the LCT |
| Canthopexy | The lower eyelid is suspended to the lateral orbital rim with a plication suture without modification of the LCT |
| Canthotomy | Lateral canthal skin incision |
| Lateral canthus | The general area where the upper and lower lids meet laterally |
| Lateral commissure | The point of union of the upper and lower lids at the lateral canthus |
| Lateral canthal tendon | Connective tissue structure that secures the upper and lower terminal eyelid to the lateral orbital rim |
| Lateral retinaculum | Another name used to describe the LCT. The confluence of several of the soft tissue structures of the lateral upper and lower eyelid that have connections with the LCT |
| Lateral palpebral ligament | Another synonymous name for the LCT |
| Lateral raphe | An area of fine fibrous bands where the terminal orbicularis muscle of the upper and lower lids meet |
| Orbitofacial vector | The relationship of globe projection to the lower lid and midface. When the globe and midface are aligned in a horizontal plane, the vector is neutral. When the globe projects more anterior than the midface, the vector is negative; when the globe sits posterior to the midface, the vector is positive |
| Ab externo | Suture passage starts outside the wound (outside in) to secure the lateral retinaculum to the Whitnall tubercle |
| Ab interno | Suture passage starts inside the wound to secure the lateral retinaculum to the Whitnall tubercle |
Preoperative evaluation
Identifying the need for and type of CS is an essential element of successful lower blepharoplasty. This begins and ends with a proper preoperative assessment. First, a determination of the need for lower eyelid skin excision made. This is performed by having the patient look up and open their mouth widely. This places the lower eyelid on maximal stretch. There should not be inferior displacement of the eyelid with mouth opening. Such induced retraction suggests there is not a quantitative skin excess for excision. In this setting, skin excision predisposes to PBLER. If skin excess exists, conservative excision can be performed. When skin excision is added to lower blepharoplasty, the authors almost always add CS to surgery. Although this is not an absolute, the authors believe even minimally invasive CS is a safeguard against PBLER in these cases. The other essential element of the preoperative examination is to identify the presence of lower eyelid laxity, which is the primary factor that mandates the need for CS surgery. This can be assessed in 2 basic ways. First, the eyelid distraction test is performed ( Fig. 3 ). The lower eyelid is pulled horizontally away from the lobe. If the lower eyelid can be distracted more than 8 mm from the globe, the test is positive and confirms lower eyelid (canthal tendon) laxity exists. , The second test is the eyelid snap-back test ( Fig. 4 ). This test is performed by displacing the lower eyelid inferiorly and assessing its return to normal position without patient blink. If this is delayed, it suggests orbicularis deficit and the presence of lower eyelid laxity. , In the setting of lower blepharoplasty, it is prudent to lower one’s standards for positive tests, as even subtle degrees of laxity can lead to changes on lower lid position. With the evolution to less invasive and disruptive CS techniques, it is best to err on the side of caution when determining the need for CS and add minimally invasive surgery as needed. This is especially true (as stated) if lower lid skin excision is added, as this step increases the risk of postoperative lower eyelid malposition.