The Skin and Disorders of the Alimentary Tract, the Hepatobiliary System, the Kidney, and the Cardiopulmonary System: Introduction
|
Diseases of the skin frequently indicate, or associate with, diseases of the alimentary tract, the hepatobiliary system, the kidneys, and the cardiopulmonary system. Just as a full physical examination should be part of a full dermatologic assessment, it is important to examine the skin in a patient presenting with a systemic problem. This chapter is presented in the same order that a physician performing a full physical examination might approach the patient. The cutaneous manifestations that indicate internal disease are discussed for each step of the examination.
General Skin Changes
The presence of pallid, dry, rough, and scaly skin that is usually itchy in patients with malabsorption, chronic renal disease, or chronic hepatic disease is nonspecific. Asteatotic eczema may develop. Some patients itch without any visible abnormality of their skin.
Hyperelastic velvety skin that rebounds to the original position after being stretched, “cigarette-paper” scars, and hyperextensible joints are characteristic of the Ehlers–Danlos syndrome. Mitral and tricuspid prolapse, dilatation of the aorta and pulmonary artery, arterial rupture, myocardial infarction, and emphysema may accompany this syndrome (see Chapter 137).1
Progressive looseness of the skin with pendulous folds and droopy eyelids may be associated with generalized hyperelastosis leading to aortic dilatation and rupture, congestive heart failure, or cor pulmonale with pulmonary artery stenosis and progressive emphysema (see Chapter 137).
The skin of patients with pseudoxanthoma elasticum (PXE) is thick, lax, and yellowish, especially over the axillae, antecubital area, and neck. Yellow patches may occur on mucous membranes, especially the labia. The alterations in the ABCC6 gene responsible for PXE may also lead to arteries becoming calcified, the aortic and mitral valves thickened, and cardiovascular symptoms, such as angina pectoris and claudication are frequent symptoms (see Chapter 137).2
In Hutchinson–Gilford syndrome (progeria) and progeroid states such as Werner’s syndrome, the skin appears atrophic and tight from a very early age. There is marked loss of subcutaneous tissue, with leg ulceration. Coronary atherosclerosis frequently leads to premature death by myocardial infarction (see Chapter 139).
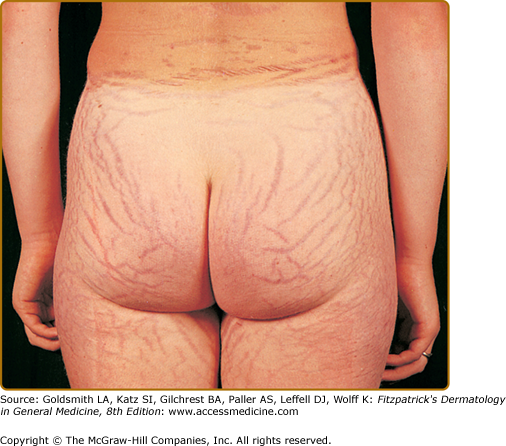
Skin changes are very common in chronic liver disease.3 Hormone-induced changes of the skin include loss of forearm, axillary, and pubic hair in both sexes. Men may experience a decreased rate of growth of facial hair, pectoral alopecia, and a female pubic hair distribution, as well as loss of libido, testicular atrophy, and oligospermia. Striae distensae occur in both men and women (Fig. 150-1). Gynecomastia, together with Dupuytren contracture and swelling of the parotid gland, is associated with cirrhosis.
Many of these changes occur more commonly in those where alcohol is the underlying cause. Patients with chronic alcoholism also develop a “pseudo-Cushing syndrome,” even in the absence of liver disease; signs include facial mooning, truncal obesity, and proximal muscle wasting. These changes may regress if the patient discontinues alcohol.
Patients with chronic liver disease often have telangiectatic changes, mainly on light-exposed skin. Numerous tiny telangiectases sometimes give the impression of a diffuse, almost exanthematic redness. They are known as “dollar paper markings” after the small threads visible in paper money held up against the light. They fade on pressure with a glass slide and rarely pulsate.
The skin of patients with chronic renal failure (CRF) is frequently dry, often with ichthyosis-like scaling,4 possibly resulting in part from altered vitamin A metabolism.5 The fluid volume shifts of dialysis may exaggerate this.
Skin color is altered in CRF. The skin is pale due to anemia and often exhibits a distinctive muddy hue, due to accumulation of carotenoid and nitrogenous pigments (urochromes) in the dermis, although its etiology is complicated and may depend in part on treatment modalities used.6
An increase in the absolute amount of desaturated (reduced) hemoglobin results in a purple–blue discoloration of the skin. Cyanosis is classified into “central” and “peripheral” types: the terms referring to the level of arterial oxygen saturation rather than the anatomic source of cyanosis. Thus, central cyanosis occurs in states that produce low arterial oxygen saturation, such as congenital heart disease with intracardiac or intrapulmonary right-to-left shunting, or severe lung disease. Peripheral cyanosis develops when there is normal arterial oxygen saturation but reduced blood flow, such as low-output cardiac failure and local vasoconstriction. Pulmonary embolism may result in a combination of central cyanosis and peripheral cyanosis.
Central cyanosis is usually visible on warm areas of the skin like the tongue, oral mucosae, and conjunctivae. Peripheral cyanosis is seen on cooler areas such as the nose, lips, earlobes, and fingertips. In the anemic patient, detection of cyanosis may be impossible because the absolute amount of reduced hemoglobin is not increased. Cyanosis fades when pressure is applied because the coloration is within the blood vessels.
Redness of the skin is caused by an increase in the amount of saturated hemoglobin, an increase in the diameter or actual number of skin capillaries, or a combination of these factors. Edema of the face, arms, and hands associated with redness and/or cyanosis may indicate obstruction of the superior vena cava due to mediastinal disease.
Primary polycythemia may produce a characteristic “ruddy” complexion but, in secondary disease especially, may also cause a peculiar ruddy cyanosis. This is most pronounced on the tongue, lips, nose, earlobes, conjunctivae, and fingertips. It is due to increased amounts of saturated hemoglobin producing erythema with increased amounts of desaturated hemoglobin producing cyanosis because of the inability of the body to fully oxygenate the increased absolute amounts of hemoglobin. The absence of nail clubbing in polycythemia vera may help differentiate patients with from those patients with cardiopulmonary disease who develop secondary polycythemia. In addition, the hypervolemic state of polycythemia vera is associated with increased stroke volume and may lead to high-output cardiac failure. Pulmonary emboli may result from venous thrombosis secondary to hyperviscosity.
Paroxysmal intense flushing of the face, neck, chest, and abdomen, often with telangiectases of the face and neck, may occur in patients with carcinoid tumors, systemic mastocytosis, and pheochromocytoma, alone or in Sipple syndrome.
In addition to jaundice (see below), both diffuse and circumscribed pigmentary changes may occur in chronic liver disease. A diffuse muddy gray color in patients with long-standing cirrhosis is due to basal cell melanin.
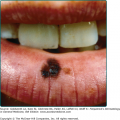
Melanosis is common in primary biliary cirrhosis (PBC) and may be an early presenting sign. It initially involves exposed areas, but gradually becomes generalized. Blotchy, circumscribed areas of dirty brown pigmentation are also occasionally evident. Accentuation of normal freckling and areolar pigmentation can occur. Localized linear pigmentation may appear in the creases of the fingers and palms. Pigmentation resembling chloasma may localize to the perioral and periorbital areas. Guttate hypomelanosis, a condition in which small white macules, sometimes with a central spider, appear on the skin of the buttocks, back, thighs, and forearms, may occur in cirrhosis and, rarely, in PBC.7 The yellow and orange lesions of dermal, subcutaneous, and tendon xanthomas and also xanthelasma are common in PBC and can be extensive (see Chapter 135).
The generalized metallic gray or bronze-brown color of the skin in hemochromatosis can be striking. There is accentuation in sun-exposed and traumatized skin, and occasionally there is buccal and conjunctival pigmentation.8
The etiology and pathogenesis of hyperpigmentation in chronic liver disease remains obscure and varies from disease to disease. The pigmentation in PBC is due predominantly to excess melanin with no stainable iron, while in hemochromatosis, pigmentation results both from the presence of hemosiderin in the skin and excess melanin. After phlebotomy, histologic siderosis and pigmentation decrease, even though melanosis remains histologically.
Pellagra gives rises to lichenified, and often deeply pigmented skin in sun-exposed sites and can develop in patients with alcoholic liver disease. Vitamin B12 deficiency causes pigmentation of the distal extremities in a glove and stocking distribution. Diffuse hyperpigmentation occurs in folate deficiency. Kwashiorkor produces generalized depigmentation (see Chapter 130).
|
In jaundice, raised plasma bilirubin produces a generalized coloration of the skin, mucous membranes, and other body tissues varying in hue from faint golden to dark green–yellow. Both jaundice and pigmentation are most prominent in extrahepatic biliary obstruction and in PBC.
Jaundice results from increased cellular or connective tissue binding of bilirubin and its metabolites in the skin. Bilirubin has an affinity for elastin, but circulates almost exclusively as a tightly bound complex with albumin. Eighty-five percent of bilirubin comes from the degradation of heme, the remainder from other heme-containing proteins, such as myoglobin and cytochromes. Jaundice results from an imbalance between tissue production and hepatic clearance of bilirubin.
Tissue-serum equilibration is slow, and so the intensity of clinical jaundice often fails to reflect the concurrent serum bilirubin level. Hyperbilirubinemia may, therefore, antedate the onset of detectable jaundice, and jaundice may persist despite falling or normal serum bilirubin levels. The correlation between skin color and serum pigment levels is especially poor in newborns. The intensity of jaundice and levels of serum bilirubin in patients with biliary atresia, acquired bile duct obstruction, or defective bilirubin conjugation tend to stabilize despite continued pigment production. Congestive cardiac failure may cause hyperbilirubinemia and jaundice secondary to raised intrahepatic pressure.
Clinically detectable jaundice appears when sufficient amounts of bilirubin become tissue bound. Involvement of the sclerae differentiates jaundice from other causes of skin pigmentation, including carotenemia, the yellow skin pigmentation produced by quinacrine and busulfan, and lycopenemia due to the ingestion of tomato juice.
The urine becomes dark yellow and even brown in color as conjugated serum bilirubin rises. Because most of the brown color of normal feces is due to urobilins derived from degradation of bilirubin in the intestine, the jaundice of impaired bilirubin excretion or bile obstruction is associated with “clay-colored” stools. Ultraviolet radiation enhances degradation of bilirubin; this is the rationale for phototherapy to prevent kernicterus in severe neonatal jaundice.
The jaundice of biliary obstruction resolves after the obstruction is relieved. Jaundice in patients with acute hepatitis resolves spontaneously. The jaundice of chronic liver disease may improve after transplantation. Jaundice in chronic active hepatitis can decrease after glucocorticoid therapy. Neonatal jaundice may respond to phototherapy (see Chapter 237).
Pruritus
One of the most common and distressing symptoms of hepatobiliary disease is pruritus. Although retained cutaneous bile acids have been implicated, there is a poor correlation between the plasma bilirubin and the severity of pruritus. However, the partial relief of itching by bile salt-chelating resins and the disappearance of pruritus when liver cells fail strongly indicates that the liver must manufacture at least one of the contributing agents.
Opiate agonists, such as morphine, induce pruritus. Animal studies show that the intracerebral presence of morphine induces pruritus that is reversed by the opiate antagonist nalaxone,9 demonstrating that opiate agonists induce itching centrally. In addition, the administration of the opioid antagonist nalmefene to patients with PBC produces a reaction similar to that of opiate withdrawal, and the injection of plasma from patients with PBC into monkeys produces pruritus. Taken together, these studies suggest that opioidergic tone increases in cholestasis.9 These studies do not, of course, tell us which agent(s) cause the pruritus of cholestasis, nor whether it originates peripherally (e.g., in the liver) or centrally.10
Pruritus more commonly occurs in conditions causing cholestasis and ranges from mild and transient to severe and prolonged. Pruritus may be debilitating in patients with PBC, mechanical biliary obstruction, or intrahepatic obstruction. Drugs, especially erythromycin, oral contraceptives, phenothiazines, chlorpropamide, para–aminosalicylic acid, and nitrofurantoin, induce cholestasis accompanied by pruritus. Pruritus is the presenting symptom in more than 50% of cases of PBC and may precede jaundice by months or even years. However, in viral hepatitis, itching is frequently missed as an early sign of the disease until it occurs in the later, icteric phase.
Pruritus is usually most marked on the extremities and only rarely involves the neck and face, and genitalia. There is little correlation between the severity of cholestasis and the severity of perceived pruritus: a spontaneous decrease in the intensity of pruritus may signal the development of hepatocellular failure rather than improvement. Scratching gives only very temporary relief in the pruritus of cholestasis. There may be no visible skin changes except excoriations, although lichenified plaques, nodular prurigo or peforating collagenoses may be seen (see Chapter 69).
Pruritus rapidly decreases when cholestasis secondary to mechanical bile duct obstruction is relieved. Drugs to relieve cholestasis such as ursodeoxycholic acid do not consistently relieve pruritus, nor do the anion exchange resins cholestyramine and cholestipol, which are thought to bind intestinal pruritogens and prevent them making their way to the skin. Neurotransmitter receptor antagonists such as oral nalmefene have been advocated for the pruritus of cholestasis11 Intravenous naloxone has short-term efficacy12 as has oral naltrexone.13 However, while these, together with sedating antihistamines or ultraviolet light can help, long-term results with any approach, including plasmapheresis, charcoal hemoperfusion, and hepatic enzyme inducers (such as rifampicin) have been disappointing.14
Renal pruritus is a major problem4 and reported to be as high as 90% in patients undergoing hemodialysis.15–17
Renal pruritus has been thought to be caused by a combination of increased serum histamine, vitamin A, and parathyroid hormone (PTH); mast cell hyperplasia; peripheral polyneuropathy; xerosis.16,18; and inflammatory factors.19 Clinically, the skin may appear normal or demonstrate a variety of lichenified or hyperkeratotic lesions.20
Topical moisturizers alleviate pruritus associated with xerotic skin. Topical glucocorticoids and ultraviolet phototherapy21,22 are often used to suppress inflammation in treated areas. Topical capsaicin depletes substance P from nerve endings, thereby suppressing itch sensation.23 Gabapentin and the κ-opioid-receptor-agonist nalfurafine have also been found useful.19 Improving the efficacy of dialysis and/or changing the dialysate concentration may help to alleviate pruritus.24 Some patients have responded to treatments with intravenous lidocaine, heparin, and cholestyramine.22 Surgical options include subtotal parathyroidectomy, electric needle stimulation, and renal transplantation. Erythropoietin lowers plasma histamine concentrations with subsequent improvement in pruritus.25 There are reports of success with oral evening primrose oil,26 and endocannibinnoids.27 Thalidomide, pentoxiphylline, and topical tacrolimus ointment may help some patients.19,28
Sweating may be prominent in a number of cardiopulmonary states such as acute myocardial infarction, cardiogenic shock, left ventricular failure, massive pulmonary emboli, and pulmonary edema. Pallor and clamminess/coldness of the extremities and exposed surfaces are also often found. Excessive sweating may suggest pheochromocytoma when associated with hypertension.
The sodium and chloride content of sweat is increased in patients with cystic fibrosis and may lead to an increase in skin wrinkling after immersion, as when bathing.29
(See also Chapter 153)
Many skin changes occur in association with malignancies.
Dry skin (acquired ichthyosis) with asteatotic dermatitis as well as hyperpigmentation is not uncommon.
(See Chapter 156)
Adult onset dermatomyositis is associated with underlying malignant disease in a significant minority of cases.30 Blind CT scans may help uncover occult malignancy in these patients.31 Pancreatic, gastric, and colorectal cancers are the third most common after bronchogenic and ovarian cancers in Europe and North America. In China, nasopharyngeal carcinoma is common. The rash and myopathy can regress after removal of the tumor.
Interstitial lung disease occurs32 with bronchiolitis obliterans, subcutaneous emphysema, and spontaneous pneumothorax. Upper pharyngeal weakness can lead to chronic aspiration an, exertional dyspnea can occur because of weakness of the respiratory muscles. Lung disease is associated with anti-Jo-1 antibodies.
(See Chapter 151 and 153)
In two-thirds of patients with acanthosis nigricans and cancer, the tumor is gastric. The changes may regress if the tumor, usually an adenocarcinoma of the stomach or bowel, is removed.
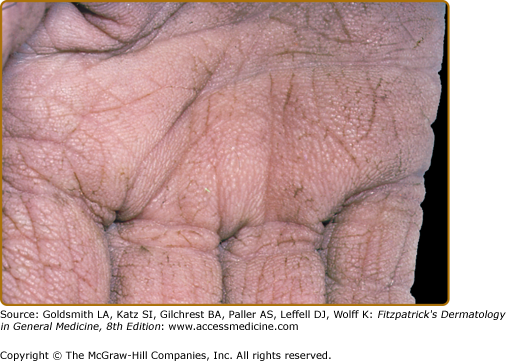
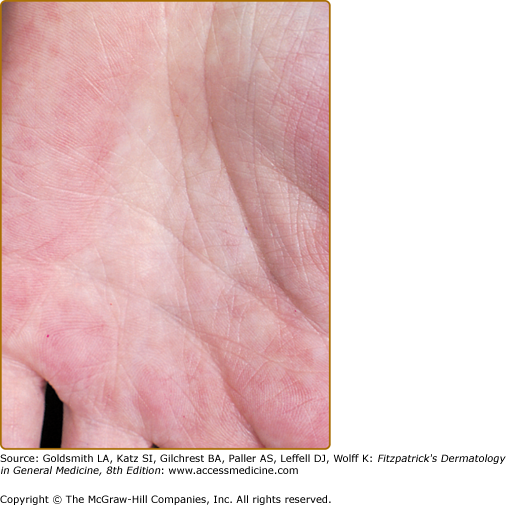
Diverse cutaneous paraneoplastic syndromes may arise from underlying tumors.33 They may precede, coincide with, or follow the diagnosis of cancer and usually indicate a poor prognosis. They include reactive erythemas, such as erythema gyratum repens and necrolytic migratory erythema; the vascular dermatoses (trousseau syndrome); and papulosquamous disorders, including tripe palms (Fig. 150-2), palmar hyperkeratosis, acquired ichthyosis, pityriasis rotunda, Bazex syndrome, florid cutaneous papillomatosis, the sign of Leser–Trélat, and extramammary Paget disease. Migratory superficial thrombophlebitis occurs in association with neoplasia, particularly carcinoma of the pancreas. Glucagonoma, one of the amine precursor uptake and decarboxylation (APUD) cell tumors, usually arises in the islet cells of the pancreas, and occurs in association with a distinctive necrolytic migratory erythema (see Chapter 153).
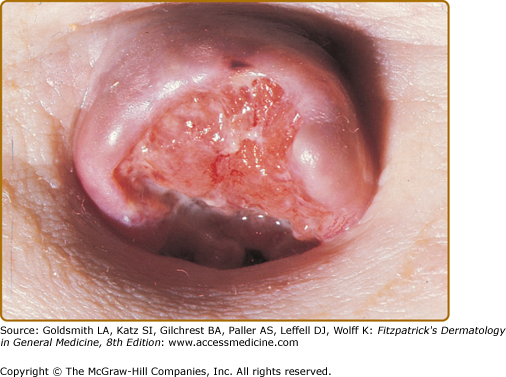
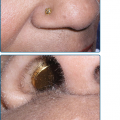
Any tumor may metastasize to the skin. The scalp is a common site. Metastases at the umbilicus (Sister Joseph nodules) occur particularly with carcinoma of the stomach, colon, or ovary (Fig. 150-3).
(See Chapter 23)
The systemic effects of erythroderma can be considerable. Patients can develop hypothermia, hypoalbuminemia, hypovolemia, secondary sepsis, the initial stages of renal failure, and high-output cardiac failure with secondary effects on hepatic function. Death from sepsis, cardiac failure, adult respiratory distress syndrome, and capillary leak syndrome occur.34
Specific Organ and System Changes
(See Chapter 89)
Lindsey, or half-and-half, nails are normal in their distal 50% and white in the proximal 50% and found in CRF.
In malabsorption or malnutrition, nails grow more slowly, become brittle, and may develop fissures.35,36 Multiple pigmented bands can appear. Koilonychia usually indicates iron deficiency, even without anemia (see below). White nails, thought to be due to selenium deficiency, have occurred with total parenteral nutrition.
Flushing of the nail beds that is synchronous with the heartbeat is a sign of aortic regurgitation called Quincke pulsation.
Nail abnormalities are a less constant physical sign than spider nevi or liver palms. In cirrhosis, however, a number of changes may occur: clubbing, curved nails, thickened nails, longitudinally ridged nails, white nails, watch-glass deformity, flattened nails, white bands, striations, and brittleness.36
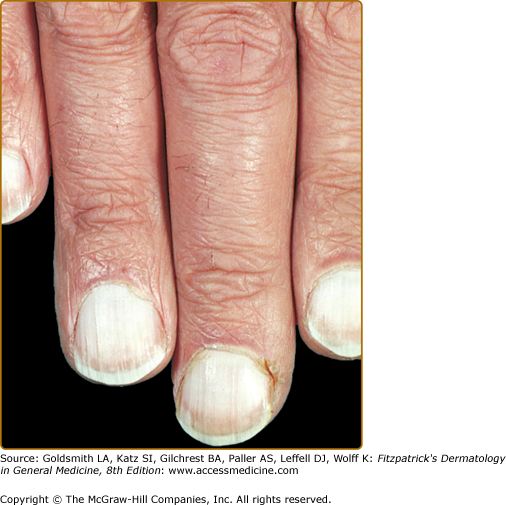
White nails may occasionally be seen in healthy individuals or in association with systemic disease, including congestive heart failure, diabetes, cryoglobulinemia, Raynaud syndrome, and systemic sclerosis. Intensely white nails (Terry nails) are characteristic of cirrhosis (Fig. 150-4).37 Thumbs and forefingers are often most affected. The whiteness does not alter with nail growth or with compression of digital vessels and is thought to be due to the opacity of the nail plate itself. The so-called watch-glass deformity may accompany white nails (see Fig. 150-5).
Azure lunulae, a bluish color of the lunular portion of nails, occurs in hepatolenticular degeneration (Wilson disease). Azure lunulae and corneal changes resembling Kayser–Fleischer rings may also be evident in patients with argyria or following treatment with busulfan or antimalarials.36
The characteristic nail changes of lichen planus, including longitudinal ridging, pterygium formation, and permanent nail loss, occur both with and without skin changes in PBC (see Section “Cutaneous Manifestations of Primary Biliary Cirrhosis”).
Splinter hemorrhages also occur in cirrhosis. Flat or spoon nails are less common in patients with liver disease. The nails are flat or concave, pale in color, and frequently show longitudinal ridging. In hemochromatosis, koilonychia is probably the most common of the nail abnormalities, but it is not related to anemia.36
Nail clubbing most commonly occurs in patients with bronchogenic carcinoma, suppurative lung disease, endocarditis, and congenital heart disease, but it may be idiopathic or familial (Fig. 150-6). Clubbing is quite common in all forms of cirrhosis, especially PBC and chronic active hepatitis. Signs include beaking or distal curvature of the nail. There may be loss of the angle between the nail and cuticle. Sponginess or “floating” of the nail when pressure is applied is also characteristic and the size of the terminal tuft may increase.
Anatomically, there is an increased thickness of the nail bed. This is due to edematous infiltration of the soft parts of the terminal segment followed by hyperplasia of the dermal fibrovascular tissue with increased vascularity.36
This is the triad of yellow nails, primary lymphedema, and pleural effusion(s). The characteristics of the nails include thickening, transverse ridging, diminished growth, increased curvature with a “hump,” and onycholysis. The lunulae and cuticles may be absent. The color may vary from pale yellow to green (Fig. 150-7). The nail changes are secondary to congenitally hypoplastic lymphatics,38 leading to lymphedema, which is characteristically slowly progressive and somewhat asymmetric, with induration and hyperkeratosis extending to the thighs. Periodic lymphangitis is frequent and may contribute to the swelling.
Respiratory findings include sinusitis, bronchiectasis, and pleural effusions. Patients may have frequent upper respiratory infections, and pneumonia. The appearance of pulmonary features and lymphedema may be late and lymphoma or sarcoma have been reported.
Fingers
(See also Chapter 173)
Erythromelalgia (labile hyperthermia) is a chronic clinical syndrome that is characterized by recurrent attacks of burning pain in the hands and/or feet with redness and warmth.39 There may be swelling that extends to the elbows and knees. Erythromelalgia may be primary or secondary to a disorder such as atherosclerosis, hypertension, and polycythemia. Symptoms are thought to be caused by vascular dysfunction including arteriovenous shunting and reduced capillary perfusion with subsequent tissue hypoxemia.40 Management includes analgesia, controlling secondary and underlying factors, and use of drugs such as aspirin and calcium channel blockers.41 A possible role for high-dose oral magnesium has been proposed42 and the use of a combination gel of 1% amitriptyline and 0.5% ketamine used to treat refractory erythromelalgia pain.43
Clubbing is often a feature of hypertrophic osteoarthropathy (HOA) but there is also associated arthralgia and/or arthritis of the fingers, wrists, knees, and ankles. There is a painful periostitis with subperiosteal new bone formation on X-ray. There may be pitting edema, shiny skin, increased sweating, and paronychial thickening. HOA is most often secondary to malignant tumors of the chest.
Pachydermoperiostosis, a primary form of HOA, is frequently familial with an onset around puberty, and has a number of cutaneous manifestations. Distinctive thickening and furrowing of the skin of the scalp, forehead, and cheeks may create leonine facies. Other features include excessive sweating and dermatitis, especially of the hands and feet, severe seborrhea of the scalp and face. Familial clubbing alone may also be found and may represent a partial expression of this syndrome. Thyroid acropachy (Chapter 151) may mimic osteoarthropathy but is most often painless.
The shoulder–hand syndrome is a painful periarthritis or adhesive capsulitis of the shoulder (“frozen shoulder”), usually on the left side, associated with erythema, increased sweating, shiny induration, edema, tenderness, pain, and immobility of the ipsilateral hand. Reduction of finger flexion, loss of movement, temperature changes, sensory disturbances, and, hair/nail growth changes have been reported.44 Neurotrophic ulcerations of the fingers and thickening of the palmar aponeurosis with nodules and/or Dupuytren contracture may be late sequelae.45 Predisposing conditions include arterial embolization, cerebrovascular accidents, and protective disuse of the arms for any reason.46
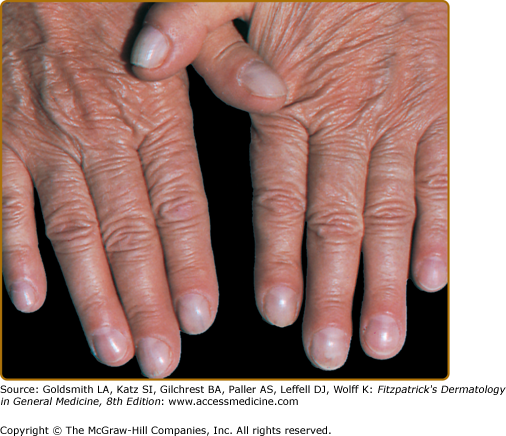
There are two clinical forms of palmar erythema. In the first (Fig. 150-8), there is an exaggeration of normal mottling; the hands are warm and bright red, especially on the palm, the dorsae of the hands, the fingers, and the nail bases. In the second, there is well-demarcated redness of the hypothenar eminence that gradually spreads to the fingertips and then to other areas of the palm. The soles of the feet may show similar changes. The mottling blanches on pressure and flushes synchronously with the pulse rate under a glass slide. Patients may complain of throbbing or tingling. Often termed “liver palms” these changes also occur in pregnancy and thyrotoxicosis. In cirrhosis, though, atrophy of the muscles of the thenar and hypothenar eminence may coexist. This is of myogenic rather than neurogenic origin.47
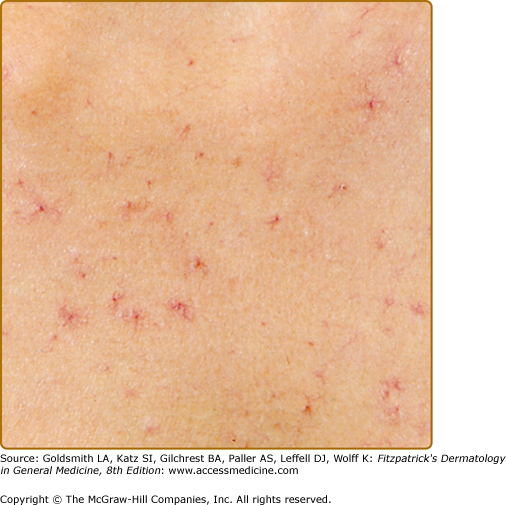
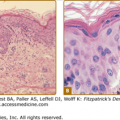
The spider nevus, or spider angioma, is the most representative and classic vascular lesion of chronic liver disease. Clinically, it has a central arteriole from which numerous small, twisted vessels radiate (Fig. 150-9). Spider nevi range in size from a pinhead to 2 cm. Larger lesions can be seen to pulsate when pressed with a glass slide. Pressure over the central arteriole causes blanching of the whole lesion. Spider nevi are characterized by the abnormal permanent dilatation of end vessels. Histologically, spider nevi consist of a central ascending arteriole ending in a thin-walled ampulla beneath the epidermis from which small arterial branches radiate outward into the papillary dermis.3
Spider nevi are most common on the face, neck, and upper part of the chest (i.e., over the region drained by the superior vena cava; see Fig. 150-9). They may be seen in 15% of healthy adults and not infrequently in children, where they tend to affect the hands and fingers. They may appear in large numbers during pregnancy, but usually disappear after parturition. They may also be seen in thyrotoxicosis or due to oral contraceptives.
In liver disease, spider nevi usually persist but can regress with improvement of the underlying condition. Spider nevi are more common in patients with alcoholic cirrhosis than in those with viral or idiopathic cirrhosis. In alcoholic cirrhosis, they are associated with the presence of esophageal varicosities, and their presence may be a useful predictive marker for the future risk of esophageal bleeds.48
Vascular spider nevi and palmar erythema (see above) are generally attributed to estrogen excess, particularly because they also occur during pregnancy and because estrogens have an enlarging, dilating effect on the spiral arterioles of the endometrium. This would also explain spider nevi in men receiving estrogen therapy for prostatic cancer. However, in addition to higher plasma estradiol:testosterone ratios, patients with nonalcoholic cirrhosis have been shown to have higher substance P levels than healthy controls.49 Vascular endothelial growth factor (VEGF) may also have an etiopathogenic role.50 In alcoholic cirrhosis, the presence of alcoholism and elevated serum bilirubin are both important predictors of the presence of spider nevi.51
Corkscrew scleral vessels (tortuous small arteries that traverse the margins of the ocular sclerae) can develop in patients with chronic liver disease.
When dermatologic diseases extend into the pharynx and esophagus, dysphagia may occur. Cutaneous and oral infections are discussed elsewhere. Symptoms resulting from infections of the esophagus occur in patients taking oral or inhaled glucocorticoids or in those who have an immunodeficiency. Candida albicans is the most frequent pathogen, although opportunistic bacteria and viruses can also be responsible.
Extensive esophageal involvement with blisters, erosions, and strictures can occur in hereditary epidermolysis bullosa particularly in the recessive dystrophic and junctional forms (see Chapter 62).52 The acquired immunobullous disorders can affect mucosae. Dysphagia is most troublesome in cicatricial pemphigoid where half of patients have pharyngeal involvement and up to 13% esophageal involvement (see Chapter 57).53
Esophageal lichen planus has been reported only in women, typically middle-aged with oral involvement (see Chapter 26). Therapeutic dilatation can lead to a Koebner-like exacerbation of the stricture.54 Esophageal involvement also occurs in Darier disease, sometimes in association with esophageal carcinoma (see Chapter 51),55 and in acanthosis nigricans. The mucosae may be extensively involved in Stevens–Johnson syndrome and toxic epidermal necrolysis (see Chapters 39 and 40).
In Behçet syndrome (see Chapter 166), which should always be considered in a patient with three episodes of oral ulceration in a 12-month period, isolated mucosal ulcers can occur at any point along the gastrointestinal tract.56 A typical site is the ileocecal region. Oral ulceration can sometimes be difficult to distinguish from the mouth ulceration associated with Crohn disease.
In Plummer–Vinson (Paterson–Kelly) syndrome, a postcricoid web is associated with koilonychia, angular stomatitis, a sore tongue, and, usually, iron deficiency. Up to 10% of patients with a postcricoid web develop carcinoma at the site. The form of tylosis in which 95% of patients develop esophageal cancer is exceedingly rare.57
Up to 90% of patients with systemic sclerosis have gastrointestinal involvement, but this is subclinical in one-third (see Chapter 157). Dyspepsia due to gastroparesis is common; decreased peristalsis, esophageal dilation, and stricture formation occur. Gastric antral vascular ectasia is a rare manifestation that may cause significant bleeding.58 In dermatomyositis and polymyositis, decreased esophageal motility and difficulty swallowing are indications for urgent systemic treatment with high-dose glucocorticoids and immunosuppressive drugs (see Chapter 156). Vasculitic ulcers in the mouth and pharynx may occur in systemic lupus erythematosus (see Chapter 155).
The presence of a diagonally positioned skin crease along the earlobe, either unilateral or bilateral, suggests an increased risk for coronary artery disease (CAD) in men under 60 years of age.59
(See Chapter 159)
Relapsing polychondritis is characterized by inflammation and destruction of cartilage and connective tissues, including those of the cardiopulmonary system. It is idiopathic but frequently associated with other immunologic disorders such as systemic lupus erytematosus (SLE). Auricular chondritis with pain, swelling, and redness of the pinna but complete sparing of the lobes is characteristic. Respiratory tract involvement may begin with hoarseness or tenderness of the anterior trachea. Degeneration of the laryngeal, tracheal, and/or bronchial rings may lead to progressive insufficiency or to sudden collapse. Cardiac involvement includes degeneration of the aortic ring with valvular insufficiency and aneurysmal dilatation. “Floppy” mitral valve syndrome also occurs. Pericardial and myocardial abnormalities have been reported.
(See Chapter 88)
Malnutrition causes hair to grow more slowly, fall out more easily, and become gray. The hair root diameter and the proportion of anagen hairs decrease. Lanugo hair may develop. Kwashiorkor, a form of protein–energy malnutrition, causes hair to become hypopigmented, varying from red–yellow to white, and curly. There may be alternating bands of pale and dark hair.35 Total parenteral nutrition has been associated with hair loss and pigmentation of remaining hair. Type 2 vitamin D-dependent rickets is associated with alopecia totalis.
Frontoparietal male pattern baldness is more prevalent in men admitted with nonfatal myocardial infarction.59 Vertex hair loss may be more strongly associated with cardiovascular risk factors, such as hypertension and hypercholesterolemia.60
|
Cardiac output frequently increases in patients with cirrhosis, and total peripheral resistance may decrease.
The familial hyperlipidemias comprise a group of metabolic disorders with elevated plasma cholesterol and/or triglycerides, associated with a high incidence of CAD. Xanthelasmata and cutaneous xanthomata are important clinical features (see Chapter 135).
This is an autosomal recessive mutation in desmoplakin, a desmosomal protein important in cell adhesion.61 Generalized striate keratodermas are seen, particularly on the palmoplantar epidermis, with woolly hair and dilated left ventricular cardiomyopathy leading to arrhythmias, heart failure, and early sudden death (see Chapter 50).
Atrial myxomas, the most common primary tumors of the heart, are benign hamartomatous intracardiac tumors. The cardiopulmonary findings include, in order of frequency, congestive heart failure, mitral murmur, chest pain, pulmonary edema, and pulmonary emboli. Additionally, valvular insufficiency, constrictive pericarditis, conduction blocks, and arrhythmias may occur. Variable murmurs can be an important clue. Other systemic findings include fever, cachexia, arthralgia, clubbing, hypergammaglobulinemia, and leukocytosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree