Fig. 5.1
Evolution of mandible reduction surgery. Mandible reduction surgery has evolved from (a) simple resection of the angular portion to (b) contouring of the total mandible shape as the desire for a slim and small face has increased. Recently, (c) V-line surgery not only narrows the width of the mandible and contours the jawline but also reduces the size and controls the position of the chin was introduced to achieve a slim and oval-shaped jaw
On the basis of technical perfection, establishment of appropriate surgical indication for each technique is mandatory in order to achieve aesthetically pleasing results. Analysis of the individual’s entire face should come from a thorough understanding of lower facial type. Authors classified the shape of lower face according to the shape of the chin, which is helpful in establishing the treatment plan in practice [15] (Fig. 5.2).
Fig. 5.2
Classification of mandibular shape and the patient’s preference of mandibular shape. The chin should be designed based on individual needs and demands. For this, the patient can freely compare the shapes of the mandible, especially chin and consult with the surgeon in detail
Patient Consultation and Assessment
Patient Selection and Consultation
Mandibular contouring surgery that we perform mainly consists of two types; (1) simple resection of the angular portion and (2) V-line surgery which includes narrowing genioplasty combined with mandibular border resection. All of these may be combined with sagittal resection of the lateral cortex. Simple resection of the angular portion is recommended for a patient who has a prominent mandibular angle only. However, in most cases, V-line surgery is more required to change the overall shape.
Before operation, the reason for surgery must be carefully assessed and clearly understood by the surgeon because a patient may be enthusiastic and quickly consult a plastic surgeon and make a decision impulsively to undergo the surgery, especially when a patient encounters someone who has already undergo this surgery. However, her or his expectation may be much higher than the reality of the outcome, and for this reason they are not the ideal candidate. For example, a patient with a thick and abundant facial soft tissue, the surgical outcomes may be below expectations in spite of successful bony reduction of mandible.
Therefore, the patients’ desire are evaluated in detail and discussed, so that the result we hope to obtain in that particular patient can be previewed. Also, skin quality such as elasticity, subcutaneous fat, and buccal fat are very important in predicting the result. Blood tests, urine analysis, heart exams, chest x-rays, and a consultation with an anesthesiologist are required. Medications that the patient is taking are also discussed and noted.
Patient Assessment
- 1.
Diagnosis
The condition may easily be diagnosed by clinical findings and radiological examination. The degree of protrusion of the mandible, asymmetry, masseter muscle hypertrophy, and the amount of the subcutaneous fat should be evaluated. The degree of hypertrophy of the masseter muscle can be identified by palpating the tightened and relaxed status of the jaw. Hyperostosis, mostly around the mandible angle, is noted in the radiologic studies. Two-thirds of the cases show mild to moderate increase in bigonial distance due to lateral flaring of the mandible angle. However, the remaining one-third shows total mandibular hypertrophy and accentuated square contour of the whole lower face. The shape and width of the lower face in the frontal view can be classified as in Fig. 5.2. The profile as well as the height of the chin should be taken into consideration. The status of soft tissue including muscle and fat should be considered as well.
- 2.
Evaluation
The author routinely obtains the patient’s photographic documentation and radiologic examination that includes panoramic view, skull lateral view, PA cephalogram, and 3D CT image. Photographs obtained using standardized techniques include frontal, lateral, oblique, basal, and overhead views. These are essential for detailed aesthetic analysis and accurate preoperative planning. For precise surgical planning and prevention of postoperative asymmetry, three-dimensional analysis of the photographs and the radiographs in the frontal, sagittal, and transverse planes are important. Examination of the shape and symmetry and understanding the overall balance of the face is mandatory. Attractive faces have certain proportions and relationships in common. To make an accurate diagnosis and establish the best treatment plan, these proportions and relationships must be thoroughly analyzed.
Frontal Plane
Using the PA cephalogram and 3D CT, the degree of protrusion or flaring of the mandible angle, symmetry, convexity of the body, deviation, and shape of the chin should be examined. Though PA cephalogram is useful in analyzing skeletal transverse discrepancy and asymmetry, it has a disadvantage of difficulty in establishing a precise head position while shooting an x-ray. However, with the use of reliable vertical baseline (a vertical line that is connected to the chin, which is started from crista galli (Cg) and crossing ANS) and horizontal reference line (Z plane, ZA plane, J plane, a line connecting the left and right antegonial notch, a parallel line to Z plane at the level of menton), degree of parallel of each of the horizon and symmetry of the facial structure can be assessed.
First, in order to analyze the facial vertical proportion, facial height (trichion–menton) is divided into three categories: upper facial height (trichion–glabella) midfacial height (glabella–subnasale), and lower facial height (subnasale–menton). Its ideal ratio is 1:1:0.8 to 1.0 in Asian women, but recently lower facial height has a decreasing tendency toward 1:1:0.8. In lower facial analysis, the ratio between upper lip length (from subnasale to stomion) and chin length (from stomion to menton) is normally 1:2. However, when upper lip length (subnasale–stomion) is out of range (normal: 20 ± 2 mm), it is difficult for surgeons to undergo surgery at a rate of above. Surgeons need to confirm the patient’s need through thorough preoperative consultation. Horizontally, facial height (Tr–Me): bizygomatic width (Za–Za) is 1.3:1 (female), 1.35:1 (male). It is recommended that bigonial width should be reduced 70% of bizygomatic width (Fig. 5.3).
Fig. 5.3
Analyzing skeletal asymmetry and facial proportions. With the use of reliable vertical baseline (a vertical line that is connected to the chin, which is started from crista galli (Cg) and crossing ANS) and horizontal reference lines (Z plane, ZA plane, J plane, a line connecting the left and right antegonial notch, a parallel line to Z plane at the level of menton), degree of parallel of each of the horizon and symmetry of the facial structure can be assessed. The face is divided into thirds by horizontal lines drawn adjacent to the menton (Me), the nasal base, the brows (Glabella, supraorbital notch level), and the hairline (Tr). The lower third is further divided into an upper third and lower two-thirds by a line drawn through oral commissures. Horizontally, facial height (Tr–Me): bizygomatic width(Za–Za) is 1.3:1 (female) and 1.35:1 (male). It is recommended that bigonial width should be reduced 70% of bizygomatic width
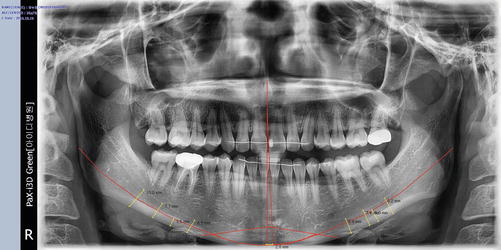
The amount of narrowing and lateralization (considering the degree of asymmetry) and the amount of angle and inferior border resection are determined after checking the course of the inferior alveolar nerve. Panoramic view is helpful in determining the amount of ostectomy of the mandibular angle and body, as well as the position of its ostectomy line (Fig. 5.4).