Chapter 46 Tendon Repairs in Replantation Surgery
This chapter does not appear in the print edition.
Surgeries and Tendon Repairs
Digital Replantation
Surgery
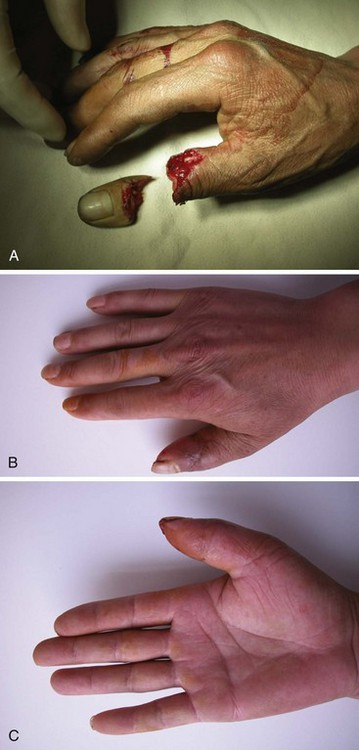
Digital amputation after clean-cut injuries does not have loss of tendon substance (Figure 46-1), but the level of tendon cut may not be the same as those in the tendons, particularly the flexor tendon. The proximal tendon ends retracted to the proximal phalanx or the palm. During crush and avulsion injuries, both flexor and extensor tendons can be avulsed from more proximal parts of the tendon (Figures 46-2 and 46-3). Additional incisions are needed to find the proximal ends and do end-to-end repair. In the thumb, both flexor pollicis longus (FPL) and extensor pollicis longus (EPL) tendons are usually cut without loss of tendon substance (Figure 46-4), and tendon avulsion from the thumb is also sometimes seen. Surgical priority should be given first to the bony fixation and re-establishment of vascular circulation. Ideally, tendons are repaired in all the cases. During replantation surgery, though slightly shortening of phalanges are necessary, tendons do not usually require shortening. Trimming the rugged tendon ends is required, which usually only produces about 0.5 cm shortening of the tendon substance.
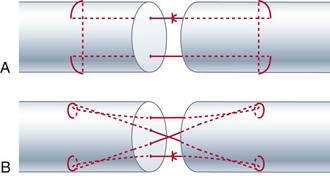
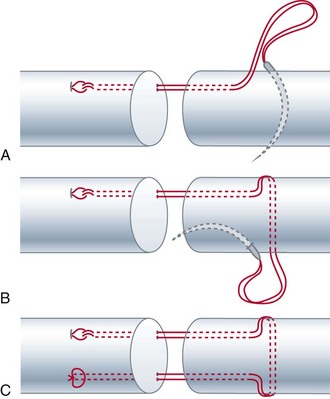
Both 2-strand Kessler and cruciate repair methods are now used popularly for flexor tendon repair (Figure 46-5). In our unit, we use a cruciate or an U-shaped four-strand repairs (Figures 46-5 and 46-6). We do not repair the FDS tendon. The FDS tendons are excised, because it is not possible to obtain good gliding and prevent adhesions after injuries to multiple tissues including bones involved in digital amputation. During surgery, we attempt to preserve the annular pulleys and synovial sheath as much as possible. Frequently, we incise or left open the sheath around the area of digital amputation. It is not possible to perform complicated pulley reconstruction during the replantation surgery, as this is not possible and lengthen the surgery. It is a practical way to leave completely disrupted annular pulleys open without surgical repair or reconstruction. It is not infrequent that we see that the A2 pulley is almost entirely damaged by the trauma, or is significantly shortened during surgery. In the case of thumb amputation, the FPL tendon must be repaired.
Outcomes
A few reports indicated effectiveness of tenolysis after digital replantation. In 1989, Jupiter and colleagues reported 37 replanted digital units and four thumb replantations with a flexor tendon tenolysis at an average of 10 months after replantation.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree