Diced cartilage with deep temporalis fascia (DC-F) graft has become a popular technique for reconstruction of the nasal dorsum. Cartilage can be obtained from the septum, ear, or costal cartilage when employing the DC-F technique. The complications seen with DC-F grafts tend to occur early in the surgeon’s implementation of this technique. Management of the complications varies depending on the severity of the problem. This article gives an overview of both the technique and the complications commonly encountered.
Key points
- •
Diced cartilage with deep temporalis fascia (DC-F) graft is a popular technique for reconstruction of the nasal dorsum.
- •
Cartilage can be obtained from the septum, ear, or costal cartilage when employing the DC-F technique.
- •
The complications seen with DC-F grafts tend to occur early in the surgeon’s implementation of this technique.
- •
Management of the complications varies depending on the severity of the problem.
Diced cartilage with deep temporalis fascia (DC-F) graft has become a popular technique for reconstruction of the nasal dorsum. Simple in concept, the use of DC-F grafts is a choice many facial plastic surgeons make for their primary and secondary rhinoplasty operations. This graft has been validated histologically and has recently gained popularity because of its inherent advantageous characteristics. Its construction is autogenous in nature; it creates a reliable and manageable method of creating the dorsal aesthetic lines, and its complication rate is minimal compared with other dorsal grafts. Yet, there still exists a significant learning curve, and complications that require reoperation do occur despite DC-F’s growing popularity and acceptance as a standard technique. In this article, the current techniques for utilizing DC-F grafts are discussed along with the technique-specific nuances that help to increase success rates. Complications and their management are also discussed.
Diced cartilage has been used for soft tissue reconstruction since the mid-20th century. Peer first published on its use in cranioplasty and showed excellent long-term results. Burian was also utilizing this technique for nasal reconstruction in the 1960s in Prague. At that time, a curious medical student named Rollin Daniel made a visit to Burian’s unit and witnessed first-hand the technique of diced cartilage for soft tissue reconstruction. Then, in 2000, Erol wrote about his experience with over 1800 primary rhinoplasty operations using diced cartilage and Surgicel (Ethicon, Somerville, NJ, USA) (DC-S) on the nasal dorsum. This spurred Daniel to try the technique on 20 patients for radix grafts and dorsal on-lay grafts, but unfortunately, he did not have the success he had hoped for.
It was at this time that Daniel and Calvert began working together on a solution for the prevention of absorption of the diced cartilage grafts. They settled on deep temporalis fascia as the external wrap for the diced cartilage. Given his previous experience of 20 patients with the absorbed DC-S grafts, Daniel initially overcorrected many of his new DC-F grafts such that they needed subsequent operations to reduce the DC-F grafts. Thus, the first nuance of the technique was elucidated; given a stable dorsal base, there is no need for overcorrection when using DC-F for raising the radix, dorsal height, or defining the dorsal aesthetic lines. Daniel and Calvert went on to publish the first report of using diced cartilage and deep temporalis fascia grafts for radix and dorsal reconstruction.
Current techniques
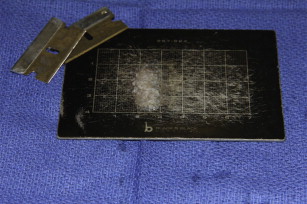
Cartilage can be obtained from the septum, ear, or costal cartilage when employing the DC-F technique. No study currently exists that shows any difference in these different types of cartilage, and the experience of the authors has been that there is no difference. The dicing of the cartilage into cubes smaller than 1 mm most likely negates any differences that might exist in the inherent cartilage properties from different sources. In fact, there have been cases in which mosaics of ear and septum, or ear and costal cartilage have been used, and there appears to be no difference in the outcome. What does, however, make a difference is is how the cartilage is diced. The cartilage must be diced into cubes smaller than 1 mm on an edge and preferably 0.5 mm on the edge ( Fig. 1 ). This can be done using #11-blades, Weck blades, or more simply autoclaved stainless steel razor blades. Typically, the dicing can be done by an assistant while the primary surgeon is preparing the nose or harvesting the deep temporalis fascia, which allows for increased efficiency during the operation.
Harvesting the deep temporalis fascia can be performed though several different incisions. In women with long hair, the incision placement is more out of convenience, but effort should be made to place the incision 1 cm above and 0.5 to 1 cm posterior to the root of the helix ( Fig. 2 ). However, the deep temporalis fascia can also be harvested through a temporal brow lift incision, an incision just above the root of the helix at the hairline for men who wear crew cuts, or even from a posterior helical incision with the aid of an endoscope. Regardless of the incision, the most important thing is to get a fascia graft that is large enough to use for the dorsum. This typically should be 4 cm in diameter or larger. Any smaller and there is a risk of a shortage of fascia when trying to construct the DC-F graft. Closure of the incision on the scalp is typically performed by reapproximating the superficial temporal fascia with an absorbable suture and then stapling the hair-bearing scalp skin ( Fig. 3 ). Routine skin closure with sutures can be used if the pretrichal incision is used (as in a man with short hair).


Once the fascia is harvested and the cartilage diced, the DC-F construct is made. It is first prudent to get an idea of what size and shape the graft needs to be in order to create the desired result. The question that must be answered is: what is the purpose of this graft? The answer can vary from augmenting the radix, raising the dorsal height, or camouflaging the multiple osteotomies of a secondary nasal fracture repair. Table 1 outlines some of the most common uses of the DC-F graft in the primary author’s (JC) practice. It is also important to get a sense of the size of the graft that is necessary when building the construct. This can be done by using dorsal sizers that are normally used in conjunction with dorsal silicone implants ( Fig. 4 ). These sizers can be placed into the soft tissue envelope to determine if the right look is created with a specific sizer. The appropriate sizer can then be duplicated using diced cartilage and fascia.
| Type of Operation | Function of Graft | Type of DC-F Graft |
|---|---|---|
| Primary rhinoplasty | Camouflage | Thin graft with 0.1–0.2 cc of diced cartilage |
| Primary rhinoplasty | Radix graft to raise the radix | Variable—depends on requirements for filling of the radix |
| Primary rhinoplasty | Define dorsal lines and smooth the dorsum | Full dorsal length (radix to septal angle) with anywhere from 0.1–1.0 cc of diced cartilage |
| Primary rhinoplasty | Major camouflage in the crooked nose | Full-length graft with variable amounts of diced cartilage and differential placement for volumetric balance of the dorsum |
| Asian rhinoplasty | Create a custom autogenous dorsum | Full-length graft with emphasis on structure for predictable healing |
| Secondary rhinoplasty | Camouflage of underlying grafts and structures | Thin graft with variable amounts of diced cartilage |
| Secondary rhinoplasty | Correct soft tissue irregularities of the dorsum from previous grafts, structural elements, damage | Full-length graft with variable amounts of diced cartilage; the greater the damage, the more cartilage should be used |
| Secondary rhinoplasty | Correct the over-resected dorsum | Used in concert with dorsal reconstruction grafts—either spreader grafts or dorsal onlay grafts to build up height |
| Infected dorsal implant | Used immediately after removal of the infected implant | Graft should be designed to replace the dorsal implant with whatever aesthetic modifications are needed for aesthetic improvement |
| Saddle nose deformity | After raising dorsal height with dorsal reconstruction grafts or on-lay grafts, DC-F used to create the aesthetic result | This graft needs to be placed as the aesthetic covering of the underlying reconstructed cartilaginous framework and establish dorsal aesthetic lines and contour |
The construct is then prepared on a silicone block with 27-gauge needles to help stabilize the fascia. The estimated amount of diced cartilage is placed into the fascia, the fascia folded over the diced cartilage, and the edges trimmed to the desired size. Typically, the width of a graft for an average dorsum is 10 mm. This takes into account the fact that the graft will shrink slightly over time, edge to edge, as it heals into position. 4–0 plain gut sutures are used to close the open edge of the fascia, and 2 4–0 plain gut sutures are then sutured to the cranial end of the graft and left with attached needles ( Figs. 5–9 ). These will be used to transcutaneously fix the DC-F graft at the radix. The DC-F graft is then placed into position with an Aufricht retractor and a needle driver with an assistant using an empty needle driver to retrieve the plain gut suture needles as they pass through the skin. These needles are cut off and the sutures taped to the forehead to secure them in place. The caudal end and lateral aspects of the graft are fixed in position under direct vision to ensure that graft position is maintained over the acute healing period using 5–0 chromic gut or vicryl sutures.







