After completion of this article, the reader should be able to describe the indications for lateral crural repositioning, understand the key steps to performing the procedure, and be able to manage the complications associated with this treatment strategy.
Key points
- •
Indications for repositioning include deformities such as cephalic malposition, retracted alae, the pinched nasal tip, vertical asymmetries of alar base insertion, the short nose, the severely under/over projected and under/over rotated tip.
- •
The lateral crura of the lower lateral cartilages should be stabilized in their new positions with lateral crural strut grafts.
- •
Significant detail must be paid to ensure nostril symmetry after repositioning.
- •
Lateral wall splints should be used for 1 week to ensure proper healing.
Introduction
Repositioning of the lateral crus of the lower lateral cartilages is one of the most powerful moves in rhinoplasty. The surgeon that masters this advanced maneuver will be able to successfully correct deformities that were previously not amenable to traditional rhinoplasty techniques. Perhaps the most common indication for repositioning is to alter nasal tip contour. Deformities such as cephalically malpositioned lower lateral cartilages, retracted alae, the pinched nasal tip, and vertical asymmetries of alar base insertion can be corrected with this technique. Repositioning can also be a powerful tool to alter other parameters of the nose such as length (proportionally lengthen the lateral component of the nose to match central component lengthening), projection (enable unhindered alteration of tip projection by changing dome position), and rotation (release of the lateral crus allows complete control of the medial crura to enable fixation in any desired location). Although this powerful technique can be mastered with practice, it is imperative that the novice rhinoplasty surgeon understand the potential risks associated with the maneuver and the possible deformities introduced by improper execution.
Introduction
Repositioning of the lateral crus of the lower lateral cartilages is one of the most powerful moves in rhinoplasty. The surgeon that masters this advanced maneuver will be able to successfully correct deformities that were previously not amenable to traditional rhinoplasty techniques. Perhaps the most common indication for repositioning is to alter nasal tip contour. Deformities such as cephalically malpositioned lower lateral cartilages, retracted alae, the pinched nasal tip, and vertical asymmetries of alar base insertion can be corrected with this technique. Repositioning can also be a powerful tool to alter other parameters of the nose such as length (proportionally lengthen the lateral component of the nose to match central component lengthening), projection (enable unhindered alteration of tip projection by changing dome position), and rotation (release of the lateral crus allows complete control of the medial crura to enable fixation in any desired location). Although this powerful technique can be mastered with practice, it is imperative that the novice rhinoplasty surgeon understand the potential risks associated with the maneuver and the possible deformities introduced by improper execution.
Preoperative planning and preparation
Rhinoplasty consultation should begin with a thorough history and physical examination to accurately diagnose and determine treatment-specific options for each particular patient. Preoperative photographs should be obtained in a standardized fashion (frontal, lateral, three-quarter, and base views). Newer 3-dimensional stereophotogrammetry technology provides the surgeon a powerful tool to objectively quantify shape, length, and volume changes accomplished via rhinoplasty. Digital image morphing should be considered, as it improves the surgeon’s ability to communicate with their patients preoperatively on prospective changes to the nose. Function should never be compromised for aesthetics. It is imperative that the surgeon understands the patient’s aesthetic preferences to prevent a dissatisfied patient, despite what the surgeon feels is an excellent result.
The surgeon should recognize nasal deformities that may not be correctable by traditional rhinoplasty grafting, suturing, or reductive techniques and may require more powerful maneuvers such as repositioning of the lower lateral cartilages. These may include contour abnormalities of the tip, the need to significantly lengthen the nose, disharmony between the tip and upper two-thirds of the nose requiring substantial projection/deprojection, or rotation/derotation. If repositioning is a potential maneuver, the surgeon should preoperatively pay close attention to any existing asymmetry in base insertion height, alar retraction, or notching and discuss the potential for nostril asymmetry postoperatively. The surgeon should also preoperatively inform the patient (especially the revision rhinoplasty patient) that structural grafting may be required and that an adequate supply of grafting material will be needed to change the shape of the nose and provide long-term support. This may mean the potential harvest of costal or auricular cartilage if inadequate septal cartilage is available. Such structural grafting will cause the nose to be stiffer after surgery, and it would behoove the surgeon to discuss this increased firmness with the patient so that postoperative expectations are appropriately set.
Procedural approach
Overview
Before the rhinoplasty surgeon enters the operating room, he or she should spend significant time reflecting on the aesthetic effect he or she is attempting to achieve. This is especially important if one plans to alter tip contour. The ideal tip has been described by many, but one detailed description is as follows :
Frontal view
…the tip has a horizontal orientation with a shadow in the supratip area that continues into the supra-alar regions. There is a smooth transition from tip lobule to the alar lobule without a line of demarcation. The tip-defining points are seen as a horizontally oriented highlight with shadows above and below. Two horizontally oriented opposing curved lines outline the tip highlight. The lateral extent of the highlight should continue into an elevated ridge that passes in continuity with the curvilinear contour of the alar lobule.
Lateral view
…the tip projects above the dorsum with a supratip break. Most surgically untreated noses have a slightly more cephalic supratip break, preserving a rounder nasal tip. The double break is soft with a subtle shadow at the soft tissue triangle. A more refined tip is created by lowering the position of the supratip break.
Once the surgeon understands the shape he or she is trying to achieve, it then becomes important to understand the correlation between the external nasal contour and the shape of the underlying tip structures. Only then will the appropriate steps be executed during surgery to achieve the desired outcome.
Opening the Nose
Rhinoplasty can often be performed via endonasal approach, but the authors find specifically that repositioning is best executed through the external approach. Preoperative injection with 1% lidocaine with 1:100,000 epinephrine in the standard fashion should be performed before preparing and draping for optimal vasoconstriction. Rather than mindless injection into the septum, as the surgeon uses hydrostatic dissection to begin elevating the mucoperichondrial flaps he or she should be concomitantly sizing the cartilaginous versus boney components of the septum to begin formulating the amount of available cartilage here for grafting. If none exists, he or she may elect to first harvest costal or auricular cartilage, but it is often advantageous to first open the nose to determine the size, shape, and strength of grafts that will be necessary.
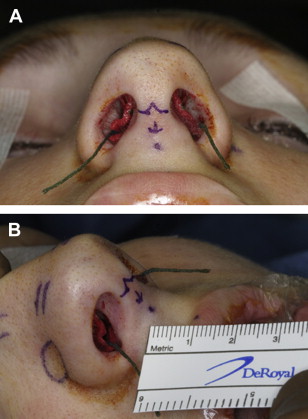
Standard inverted V-incision is made across the columella using a #11 blade, with anticipation of where the incision will be positioned at the end of the operation (ie, if the nose is deprojected, the incision is closer to the tip lobule; or, if the nose is to be projected, the incision should be closer to the lip) ( Fig. 1 ). A #15 blade should be used to make bilateral marginal incisions that are then connected to the marginal extension of the columellar incision. Sharp dissection with a Converse scissor preserves the subdermal plexus to the delicate skin of the columella, tip, and soft tissue triangles. Sharp dissection may maximize vascularity and avoid excessive swelling that can be attributed to broad spreading and tearing of the tissue with blunt dissection. Three-point retraction by 1 or 2 assistants with sharp two prong hooks will aid the primary surgeon by ensuring the proper plane is maintained. Identification of the lower lateral cartilages is followed by exposure of the cartilaginous dorsum. A Joseph periosteal elevator should then be used to dissect the periosteum from the nasal bones. Most often, septoplasty should next be initiated, either by a separate Killian incision or with lateral retraction of the lower lateral cartilages and identification of the anterior septal angle. Bilateral mucoperichondrial flaps can be raised, but harvest of septal cartilage should be postponed until work on the upper third of the nose has been completed to avoid destabilization of the keystone area. Regardless of the techniques used to straighten the septum, the surgeon should ensure a strong cartilaginous L-strut exists for long-term support of the nose. The boney dorsal contour and the middle vault should next be addressed based on the desired final tip position.
Stabilizing the Nasal Base
For advanced techniques involving repositioning of the lower lateral cartilages, the authors recommend building from a stable nasal base. Attention to the midline is critical, as this is the foundation for the nasal tip. Failure to recognize and discuss facial asymmetry with the patient preoperatively can often result in the surgeon having to offer explanations for why a straight nose may still appear deviated to the patient postoperatively. Scrupulous physical examination and study of photographs can identify these and other deviations of the caudal septum, nasal spine, dentition, or lip in relation to the midline glabella. The primary surgeon should not stand in one position, but consider frequently moving around the head of the operating room table to best evaluate symmetry.
Once the surgeon feels confident the midline has been established, the next task should be to adequately stabilize the nasal base. Traditionally, options for this have included a floating columellar strut, fixed/extended columellar strut, caudal septal extension graft, or caudal septal replacement graft. If repositioning is to be considered, it is preferable to have a fixed base rather than a floating base. If the base is freely floating, the nasal tip structure can rotate and shift with the repositioning. Obviously, this will create increased stiffness in the nasal tip.
Caudal septal extension grafts can be secured to the septum in an end-to-end fashion with extended spreader grafts and slivers of cartilage or segments of 0.25-mm polydioxanone (PDS) plate perforated with a 16-gauge needle ( Fig. 2 ). Although complex, caudal septal replacement grafts will often actually use less cartilage than attempting to straighten a severely damaged caudal portion of the L-strut. Care should be taken, as this technique requires mastery in that it has the potential to simultaneously alter the tip rotation, length, and projection. Caudal septal extension or replacement grafts are the only cartilage segments in structure rhinoplasty that need to be completely straight. If the surgeon is using costal or auricular cartilage grafts, it may be wise to use any available septal cartilage for these grafts to prevent warping or deformity.
The tripod theory is a classic description to explain tip dynamics in rhinoplasty. The nasal tip is the tabletop, with the 3 legs of the table being the left lateral crus, the right lateral crus, and the combination of the medial crura together. This theory does an excellent job of predicting rotation, projection, and length secondary to many traditional moves performed in rhinoplasty, such as cephalic trim and lateral crural steal. The theory is less applicable, however, if one plans to rigidly fixate the table of the tripod to the septum or septal extension graft. When this happens, the surgeon has essentially controlled for postoperative loss of projection and has controlled rotation/length. Once the confluence of the tripod is fixated, the legs are no longer floating in space, and thus can be moved, shortened, or lengthened, without fear of inadvertently altering position of the “tabletop.”
The next step in stabilizing the nasal base before further tip contour work is performed is to preliminarily secure the medial crura to the septum, fixed columellar strut, septal extension graft, or septal replacement graft with a 4–0 plain gut suture on an SC-1 needle. If the surgeon is pleased with this position (see later discussion), several 5–0 PDS sutures should be used to further secure the medial and intermediate crura. Care must be taken in applying these sutures, as asymmetries can affect tip position or tip symmetry. The lateral crura should then be addressed.
Tip Contouring
The next task for the surgeon during rhinoplasty is to determine which maneuvers will attain the desired changes in tip contour and position by appropriately altering length, rotation, projection, and shape. A variety of techniques can then be used including grafting, excision, suturing, and repositioning. The focus of this review is to further discuss lateral crural repositioning.
Cephalic malposition
Perhaps one of the most common indications for lower lateral cartilage repositioning is cephalically malpositioned lower lateral cartilages ( Fig. 3 ). Patients with cephalic positioning of the lateral crura typically have a parentheses-shaped tip deformity or bulbous nasal tip ( Fig. 4 ). Cephalic malposition blunts the demarcation between nasal subunits (tip/dorsum/lateral sidewall), creating excess vertical fullness in the supratip. In the more favorable orientation, the caudal margin of the lateral crus of the lower lateral cartilages, can be measured from the midline and is ideally 30° or greater. Lower lateral cartilage repositioning with lateral crural strut grafts has been shown to reliably change the orientation of the cartilages in the tip to favorably modify shape. It may also potentially reduce unwanted volume in the supratip. Repositioning with lateral crural strut grafts may also have a functional benefit over other grafts in the valve area such as alar batten grafts (Dean M. Toriumi, MD, unpublished data, 2010).






