Superficial Viral Infections
Overview
Viruses are capable of causing a wide variety of disorders of the skin and mucous membranes. Specific skin lesions vary greatly and include vesicles, pustules, papules, ulcers, and tumors. Cutaneous viral infections present in various reaction patterns, most commonly, vesicobullous, vascular (viral exanthems), or papulosquamous (pityriasis rosea).
Certain viral infections—warts in particular—vary greatly in their gross clinical manifestations despite all being caused by the same, albeit different subtypes, of human papilloma virus (HPV). For example, the clinical appearances of warts often differ markedly and manifest as papillomatatous (common warts), threadlike (filiform warts), flat (planar warts), to exuberant moist papules (condyloma acuminata), or tumors (giant condyloma acuminatum of Buschke-Löwenstein). See Chapter 19, “Sexually Transmitted Diseases.” In contrast, lesions of molluscum contagiosum tend to be quite monomorphic and uniform in appearance and vary primarily by size.
The virus of varicella-zoster (VZV) may produce the clinical syndrome of either chickenpox or herpes zoster. Herpes simplex virus (HSV) lesions may manifest in ways that produce systemic problems, whereas the virus of warts and molluscum contagiosum are entirely localized to the skin (dermatotrophic) and do not cause systemic symptoms. Systemic viral disorders such as varicella are discussed in Chapter 8, “Viral Exanthems.”
 Warts (Nongenital)
Warts (Nongenital)
Common warts
Plantar warts
Flat warts
Filiform warts
 Molluscum contagiosum
Molluscum contagiosum
 Herpes simplex (Nongenital)
Herpes simplex (Nongenital)
Primary orolabial herpes simplex
Recurrent orolabial herpes simplex
Clinical variants of herpes simplex infections
 Herpes zoster
Herpes zoster
Disseminated herpes zoster
Post herpetic neuralgia
Warts (Nongenital)
Basics
The emergence of common warts (verrucae vulgaris) and other forms of cutaneous warts is extremely common, particularly in children and young adults. An estimated 20% of school-age children will at some time have at least one wart. In children, warts tend to regress spontaneously. In many adults and in immunocompromised patients, however, warts often prove difficult to eradicate.
All warts are caused by the human papillomavirus (HPV); to date, more than 150 different subtypes have been identified. The virus infects epidermal keratinocytes, which stimulates cell proliferation. Viral transmission occurs primarily through skin-to-skin contact such as handshaking or kissing. The recently shed virus can also be found on almost anything in a moist, warm environment, including doorknobs, hand railings, and floors of locker rooms, as well as around swimming pools. Contact with any of these surfaces is another means of viral transmission; the virus is virtually impossible to avoid. Often, several family members develop warts. Whether this reflects a genetic susceptibility or is simply a result of the ubiquitous nature of the contagion has not been determined.
Factors that Predispose to Human Papillomavirus Infection
Infection with the human immunodeficiency virus (HIV) or the presence of other immunosuppressive diseases, such as lymphomas, can predispose one to become infected.
Taking drugs that decrease cell-mediated immunity (e.g., prednisone, cyclosporine, chemotherapeutic agents) is another predisposing factor. Transplant recipients who, by necessity, use such medications on a long-term basis have warts that can be very resistant to treatment.
Handling raw meat, fish, or other types of animal matter in one’s occupation (for example, butchers) increases susceptibility.
Description of Lesions
Warts are most often diagnosed based on their clinical appearance, but a biopsy can be performed if the diagnosis is in doubt. A typical wart is a papillomatous, corrugated, hyperkeratotic growth that is confined to the epidermis. Despite a common misconception, warts have no “roots,” and there is no “mother wart.”
Warts may be skin colored to tan and measure 5 to 10 mm in diameter. However, they may coalesce into clusters (mosaic warts) that can be up to 3 cm in diameter.
Warts often vary widely in shape, size, and appearance. The different names for warts generally reflect their clinical appearance, location, or both. For example, filiform warts are threadlike, planar warts are flat, and plantar warts are located on the plantar surface of the feet.
Genital warts (condyloma acuminata) may be large and cauliflowerlike, or they may consist of small papules.
Distribution of Lesions
Warts may develop anywhere on the body, but they are most often found at sites subject to frequent trauma, such as the hands and feet.
The distribution is generally asymmetric, and lesions are often clustered.
Viral protein and infectious particles have been detected in the absence of visible skin surface lesions using electron microscopy, polymerase chain reaction, and DNA hybridization techniques. Thus, it is well documented that HPV can exist in a subclinical or latent state.
This latency explains the not infrequent recurrence of warts at the same site or at an adjacent site, even when they had been apparently “cured” many years before.
Clinical Variants
Common Warts
Verrucae vulgaris, or common warts (Fig. 6.1), occur most often on the hands and fingers and in the nail area—both around (periungual) and under (subungual) nail areas (Figs. 6.2 and 6.3). They are frequently seen on the knees and elbows, especially in children.
Their distribution is generally asymmetric, and lesions are often grouped.
Description of Common Warts
Common warts generally have a verrucose, or vegetative, appearance.
Lesions show loss of normal skin markings (e.g., fingerprints and handprints).
“Black dots,” or thrombosed capillaries, are pathognomonic (Fig. 6.4).
Usually warts are asymptomatic, but they can be tender and often cause embarrassment.
 6.4 Common warts (verruca vulgaris). These lesions demonstrate loss of normal skin markings, and “black dots,” or thrombosed capillaries, are pathognomonic. |
Adult/Elderly
Seborrheic keratosis
Acrochordon (skin tag)
Solar keratosis and cutaneous horn
Squamous cell carcinoma
Keratoacanthoma
Seborrheic Keratosis
See Chapter 21, “Benign Skin Neoplasms.”
These benign lesions occur in middle-aged and older people.
They are most often seen along the frontal hairline, face, and trunk.
They have a “stuck-on” appearance.
They may be clinically indistinguishable from warts.
Solar Keratosis (Actinic Keratosis)
See Chapter 22, “Premalignant and Malignant Skin Neoplasms.”
These lesions occur in elderly, fair-complexioned persons, and they are sometimes associated with a cutaneous horn.
They are rough-textured papules that appear in sun-exposed areas.
Biopsy may be necessary to distinguish these lesions from squamous cell carcinoma.
Squamous Cell Carcinoma Under the Nail
Biopsy is necessary.
This lesion can easily be misdiagnosed as a subungual wart.
Onychomycosis
See Chapter 7, “Superficial Fungal Infections.”
The potassium hydroxide examination or fungal culture is positive.
Plantar Warts
Plantar warts are seen on the plantar surface of the feet and occur mostly in children and young adults.
They usually appear on the metatarsal area, heels, insteps (Fig. 6.5), and toes in an asymmetric distribution.
Description and Distribution of Plantar Warts
Plantar warts may be painful and can impair ambulation, particularly when present on a weight-bearing surface, such as the sole of the foot during walking.
Lesions may be solitary or multiple, or they may appear in clusters (mosaic warts) (Fig. 6.6).
There is loss of normal skin markings (dermatoglyphics). Often, there are pathognomonic “black dots” (thrombosed dermal capillaries) and punctate bleeding that become evident after paring with a no. 15 blade (Fig. 6.7).
 6.7 Plantar wart. Characteristic punctate bleeding is present after paring. Note the loss of skin markings. |
Corns (clavi) are sometimes difficult to distinguish from warts. Similar to calluses, corns are thickened areas of the skin that form in response to excessive pressure and friction.
They are usually hard and circle-shaped, with a polished or central translucent core, like the kernel of corn from which they take their name (Fig. 6.8).
Corns do not have “black dots,” and skin markings are retained, except for the area of the central core.
Corns most commonly develop on the tops and the tips of toes and along the sides of the feet. Lesions are also typically seen between the fourth and fifth toes (“kissing corns”).
Wearing high-heeled shoes—particularly shoes that shift the body weight into a narrow, tapering toe box—can produce corns.
Flat Warts
Verrucae planae, or flat warts, are commonly found on the face (Figs. 6.9 and 6.10), arms (Fig. 6.11), dorsa of hands, and the shins (women), where lesions are often spread by leg shaving.
 6.10 Flat warts (verruca planae). Very subtle, flesh-colored papules are present on this woman’s chin. |
Description of Flat Warts
These small, flat-topped, papular warts are slightly elevated and well-defined.
Papules are skin-colored or tan to brown in color, and they range in size from 1 to 5 mm. Side lighting may be necessary to see them.
Sometimes, flat warts show a linear configuration caused by autoinoculation.
In men, flat warts are spread by shaving. Flat warts tend to resolve spontaneously, sometimes after a sudden increase in number, size, and inflammation.
Flat warts may resemble molluscum contagiosum (see later text), which manifests as shiny, waxy, dome-shaped papules with a central white core.
Filiform Warts
These tan, slender, delicate, fingerlike growths that emanate from the skin, filiform warts, are most commonly seen on the face (Fig. 6.12)—usually around the ala nasi, mouth, eyelids—and on the neck.
These finger-like papules that are seen in the elderly, usually on sun-exposed areas, may overlie a wart or a squamous cell carcinoma.
 6.12 Filiform and common warts. This child has filiform warts on her nose and a common wart on her finger. |
General Principles
The management of warts is often challenging, and there is no ideal treatment. The abundance of therapeutic modalities described in this chapter is a reflection of the fact that none of them is uniformly effective (see also Table 6.1). The method of treatment depends on the following:
The age of the patient
The patient’s pain threshold
The type of wart
The location of the lesion
Providing no treatment at all may be safe and cost effective, because many warts resolve on their own. Painful, aggressive therapy should be avoided, unless there is a pressing need to eliminate the wart.
Children
In children, most warts tend to regress spontaneously, which is probably related to a host immune response.
Social factors are also important. For example, a 2-year-old child with a filiform wart located near the ala nasi, or with multiple hand warts, should warrant less aggressive treatment than a 6-year-old child with similar lesions who may suffer from the teasing of other children.
Table 6.1 Topical Wart Medications Formulary | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
Duct Tape (“Ducto-Therapy”)
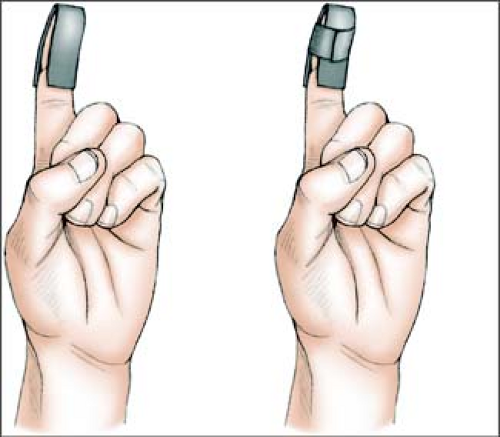
For stubborn common warts around and under the fingernails, the patient (or parent) is instructed in the following safe, easy, painless, inexpensive method that has been reported to help promote wart resolution:
Cut a roll of shiny, electrical (duct) tape into 1-inch strips.
Completely wrap the affected area with two “layers” of the tape (Ill. 6.1), making it airtight. Do not wrap the tape too tightly.
Leave the tape on for 6 days, and then remove it for half a day. Leave the tape on during bathing, working, school, and all activities.
Repeat this procedure (6 days on, 6 days off).
Treat one digit at a time.
Expect that after several weeks, the wart will become smaller, soft, and macerated and hopefully disappear.
Adults and Immunocompromised Patients
In many adults and immunocompromised patients, warts often prove difficult to eradicate.
It is necessary to explain to patients that there is no known practical way actually to kill HPV, and in many patients, when warts regress it is not because they have been “cured” but because the infection has become latent.
Patients may also be reminded that so far there are no cures for acquired immunodeficiency syndrome (AIDS) or the common cold—both of which are caused by viruses—so it is not surprising that the virus that causes warts is difficult to eradicate. Treatment often takes numerous sessions, and, on occasion, warts fail to resolve.
In short, the immune system apparently plays the most significant role in the expression of HPV. Treatment merely prompts or stimulates the immune system into dealing more effectively with the virus.
The following treatment suggestions are given in a stepwise fashion, beginning with the least painful methods. (Note: The use of many of the following topical chemical approaches may be contraindicated during pregnancy or in women who are likely to become pregnant during the treatment period.)
Home Treatment: Topical Salicylic Acid
Salicylic acid is a keratolytic (peeling) agent that can be self-administered. It has a role in exfoliating the hyperkeratotic “dead skin” of warts and inducing inflammation.
Salicylic acid is available in numerous over-the-counter (OTC) trade name preparations such as Compound W gel and solution and Duofilm gel, patch, and solution.
For best results with any keratolytic agent, the affected area should be hydrated first by soaking it in warm water for 5 minutes before application of the agent.
Advantages
These preparations provide the best treatment for small children in whom warts are usually self-limiting.
Usable on periungual warts
Nonscarring
Painless to apply
Relatively inexpensive
Do not require office visits
Disadvantages
Slow response
Often no response
Time-consuming
Cryotherapy with Liquid Nitrogen
Liquid nitrogen (LN2) may be applied with a cotton swab or with a cryotherapy gun (Cryogun) (see Chapter 26, “Diagnostic and Therapeutic Procedures”). The goals are a rapid freeze and a slow thaw. Repeated freeze–thaw cycles increase cell damage. Cryotherapy is best for warts on hands.
Regardless of whether LN2 is applied with a saturated cotton swab or with a cryotherapy gun, one should aim to create a 2- to 3-mm zone of freeze around the lesion for a total of 4 to 5 seconds. The time of application varies, depending on the thickness of the lesion.
If possible, an attempt should be made to freeze lesions at a right angle; this approach may lessen the patient’s pain and may minimize collateral damage to normal surrounding skin.
The procedure is repeated at 2- to 3-week intervals, based on patient tolerance or on previous treatment results, degree of pain, and posttreatment morbidity.
Advantages
Treatment is rapid.
Many lesions can be treated during a single office visit.
It works well for hand warts.
Disadvantages
This approach necessitates the availability of an LN2 unit and holding tank.
Treatment is painful and must be used cautiously on fingertips and on periungual lesions.
This treatment can cause painful blisters.
On darkly pigmented skin, cryotherapy can result in hypopigmentation or hyperpigmentation, or even depigmentation, because LN2 destroys melanocytes.
Overaggressive treatment may cause scarring.
Treatment often requires multiple office visits.
Electrocautery and Blunt Dissection
In electrosurgical procedures, the wart is burned by an electrical current that uses heat conduction from a hot probe heated by a direct current.
These methods are best for warts on the knees, elbows, and dorsa of hands. They are also effective for filiform warts.
Advantages
Treatment is tolerable in most adults.
Warts are removed on the day of treatment.
Disadvantages
Local anesthesia is required. Treatment sometimes necessitates a digital block, which can be painful, especially on the fingers and the soles of the feet.
Treatment may cause scarring.
It can cause nail deformity after injury to the nail matrix.
Laser Ablation
Laser destruction of warts is reserved only for large or refractory lesions.
This method is expensive and requires local anesthesia.
One study concluded that laser ablation is no more effective in eradicating recalcitrant warts than are the less costly conventional methods described herein.
Immunotherapy
Interferon Induction
Aldara cream 5% (imiquimod), a local inducer of interferon that stimulates immune up-regulation, may be applied at home by the patient. It is available as a 5% cream that is approved for the treatment of genital warts (condyloma acuminatum) (See Chapter 19, “Sexually Transmitted Diseases”).
There have been numerous anecdotal reports of the successful off-label use of imiquimod on common warts and plantar warts. It is applied under duct tape occlusion after hydrating the area to be treated. This is best done at bedtime and washed off after 6 to 10 hours. It is applied to facial flat warts without occlusion (see later discussion).
Sensitizing Agents
The deliberate induction of allergic reactions by injecting or applying sensitizing agents is sometimes used to treat warts.
Intralesional injection of the Candida skin test antigen has been associated with some reports of total clearance of warts in sites that were remote from the location of injection.
There are other contact (applied) immunotherapy agents, such as diphencyprone, dinitrochlorobenzene (DNCB), and squaric acid dibutylester (SADBE), that produce a delayed-type hypersensitivity reaction; however, there are possible mutagenic and side effects with these agents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree