■ The thyroid isthmus is clamped and divided early in the course of operation for most patients with Graves’ disease (FIG 1, right). Alternatively, an energy device can be used to transect the isthmus.
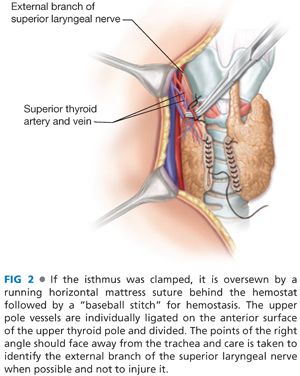
■ The isthmus on each side is then sharply dissected from the front of the trachea in order to improve mobilization of the gland. The isthmus on each side is oversewn for hemostasis (FIG 2). The medial side of the thyroid lobe to be operated on first is then carefully dissected in a superficial plane toward the upper pole, developing a plane between the thyroid lobe and the cricothyroid muscle. Care is taken to preserve and not damage the external branch of the superior laryngeal nerve and the cricothyroid muscle.
■ The thyroid lobe to be operated on first is mobilized by dividing the areolar tissue and any small vessels along its lateral surface.
■ The upper pole vessels are then individually ligated along the front surface of the upper pole and not more cephalad in the neck. The right angle is kept “pointing out laterally” to prevent damage to the external branch of the superior laryngeal nerve (FIG 2). This nerve can often be visualized if the area is carefully evaluated.
■ The thyroid lobe is then retracted medially again and the middle thyroid vein is identified, ligated, and divided (FIG 3). This vein is usually in a plane superficial to the inferior thyroid artery and to the recurrent laryngeal nerve, but all structures should be carefully evaluated before ligation.

■ The inferior thyroid artery, a branch of the thyrocervical trunk which runs medially and enters the field deep to the carotid artery, as well as the recurrent laryngeal nerve are now carefully identified (FIG 4). Whenever possible, the inferior thyroid artery is not ligated as a single trunk because this might devascularize the parathyroid glands. Rather, the small branches of the artery are individually ligated and divided along the surface of the thyroid lobe. The inferior parathyroid gland, which often is present high along the lower thyroid lobe, is mobilized with its blood supply and moved more posteriorly and laterally off the thyroid lobe.

■ The carotid artery is now retracted laterally and the recurrent laryngeal nerve is more carefully identified, usually in the lower neck, and followed in an inferior to superior direction by “unroofing” the tissues from the front of the nerve (FIG 5). Remember that on the right side, the recurrent laryngeal nerve takes an oblique course from lateral to medial and from deep to superficial. On the left side, the nerve usually runs straight upward and is usually found in the lower neck much more medially than on the right side within or near the tracheoesophageal groove.
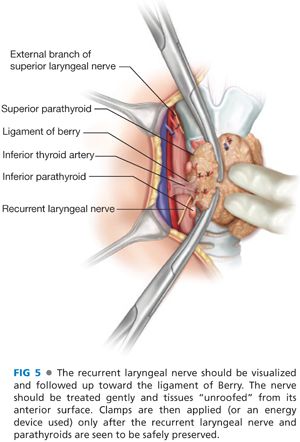
■ If a subtotal lobectomy is to be done, before any clamps are placed on the thyroid lobe, the surgeon must be certain that the recurrent nerve has been identified and followed in a cephalad direction to near the ligament of Berry and that the nerve and parathyroid glands are clearly posterior and away from the sites to be clamped. Then hemostats are applied to the tissue and most of the lobe is resected (FIG 5). The remaining small thyroid remnant is oversewn for hemostasis. This resection can also be accomplished by using an energy device if one is far enough from the nerve so the heat does not damage it. Do not perform a subtotal thyroid lobectomy without visualizing the recurrent laryngeal nerve, for this is unsafe.
■ At the end of the procedure for Graves’ disease (FIG 6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








