Striae (Rubra and Alba
Adele Haimovic
Deborah S. Sarnoff
BACKGROUND
Striae distensae (SD), often referred to as stretch marks, are linear atrophic dermal scars covered by an atrophic epidermis.1 They were first described in 1936 by Nardelli as dermal scars caused by skin stretching.2 Although SD do not cause any significant medical problems, they are a common dermatologic condition that is cosmetically concerning and cause significant psychosocial distress in affected individuals. SD are 2.5 times more frequent in women than in men.3 They follow normal skin cleavage lines and are often associated with pregnancy and growth spurts in adolescents. For adolescents the incidence has been reported to be 40% to 70%,1 and for pregnancy the incidence has been as high as 90%.4
PRESENTATION
Patients typically present during puberty, during pregnancy, or after rapid weight changes or muscular changes with a complaint of discolored lines on the abdomen, shoulders, buttocks, or thighs.
DIAGNOSIS
Clinical Diagnosis
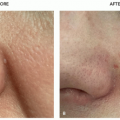
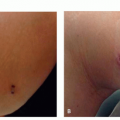
Early SD, known as striae rubra (SR), are pink to red in color (Figure 10.1.1). They may be flat areas of the skin or slightly elevated plaques. Gradually with time, they
tend to darken in color into a purple hue and increase in length. The surface may exhibit fine rhytids. Eventually, they become white and atrophic. These mature striae are referred to as striae alba (SA). SA are generally 1 to 10 mm in diameter and several centimeters in length.
tend to darken in color into a purple hue and increase in length. The surface may exhibit fine rhytids. Eventually, they become white and atrophic. These mature striae are referred to as striae alba (SA). SA are generally 1 to 10 mm in diameter and several centimeters in length.
 FIGURE 10.1.1 Axillary striae rubra in a 13-year-old girl worsened by daily application of a topical fluorinated steroid cream. |
In adolescents the most common location for striae is the buttock. The second most common location in adolescent females are the thighs, whereas it is the lower back in adolescent males. Other affected areas are the knee, breast, calf, and arms.1 In adult pregnant woman the abdomen is the most frequently affected area followed by the breasts and thighs.4,5
SR and SA are the 2 most common forms of SD. When striae develop during pregnancy, the term striae gravidarum (SG) may be used, and they typically affect the abdomen and breasts.4 Two additional types of SD were described by Hermanns and Pierard, striae nigrae and striae caerulea.6 These are found in darker skin types because of increased melanization.6
Striae induced by corticosteroid use are typically wider and larger and affect a greater surface area. They also affect areas of occlusive steroid application and typically affect the flexors.
Histopathology
On histology, early SD, or SR, demonstrate a superficial and deep perivascular lymphocytic infiltrate and sometimes eosinophils.7 Dilated venules and edema may also be seen in the upper dermis. Older striae, or SA, have a scant lymphocytic infiltrate and epidermal thinning due to rete ridge flattening.8 There is loss of both collagen and elastin fibers in the papillary and reticular dermis, which is more significant in mature striae.9 The destruction of collagen and elastin fibers is thought to be due to early mast cell degranulation and the release of the enzyme elastase.10
Subtypes
Striae rubra: red
Striae alba: white atrophic
Striae gravidarum: during pregnancy
Striae nigrae and striae caerulea: hyperpigmented
Differential Diagnosis
Cushing syndrome: extensive breadth, color, and distribution
Focal elastosis (elastotic striae): horizontal yellow linear palpable bands on lower back
PATHOGENESIS
The exact etiology of SD is unclear. Multiple theories, including mechanical stretching, endocrine abnormalities, and connective tissue defects, have been proposed. Genetic predisposition, including family and personal history, as well as ethnicity, appear to play an important role.11
SD often occur after rapid weight gain or increase in height during adolescence or pregnancy. SG affect up to 90% of women in the second or third trimester.4 One common theory is that SD are due to mechanical stretching of the skin and damage of the dermal connective tissue during this rapid growth phase.8 However, studies have contradicted this theory as increased abdominal girth, baseline body mass index, and infant birthweight do not consistently correlate with the development of SG.11,12,13
Hormonal changes may be a key player in the development of SD. Increased glucocorticoid production, as seen with puberty, pregnancy, exogenous steroid use, and Cushing syndrome, is associated with SD. Elevated levels of steroid hormones and their metabolites have been shown in the serum of individuals with striae.14 Adrenocorticotrophic hormone and cortisol are thought to stimulate fibroblast activity leading to alterations of collagen and elastin fibers.5 Cordeiro et al described a significant increase in estrogen and androgen receptors in SD skin compared with healthy skin.14
Genetic factors have been suggested to be important in the development of striae. A familial form of SD,15 as well as SD in monozygotic twins, has been reported.16 Connective tissue diseases, such as Marfan syndrome, are associated with SD.17 Marfan syndrome is associated with a mutation in the gene that is essential for normal elastic fibers, fibrillin. Fragmented elastic fibers may explain the high frequency of SD in individuals with Marfan syndrome.17
TREATMENT
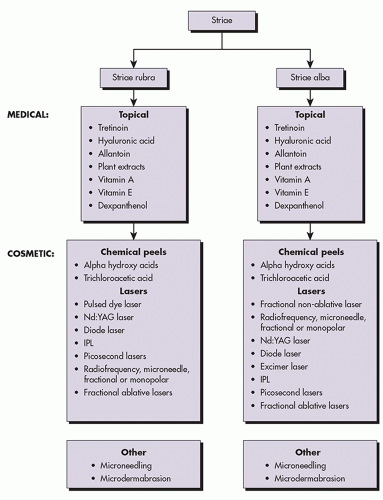
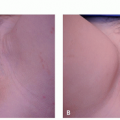
SD are very challenging and frustrating to treat. Numerous therapies have been proposed; however, to date there is no consistent effective solution for SD. Therefore, when discussing therapeutic options with patients, realistic expectations must be set. Many believe that SD are more effectively treated when they are active, before
they become white and atrophic.18 Treatment modalities including topical creams, microneedling, microdermabrasion, laser and light devices, and radiofrequency (RF) devices have been studied. Diet and exercise have not shown to improve SD.19 When choosing a therapy, one must consider the type and color of the striae as well as the patients’ Fitzpatrick skin type (FST) (Algorithm 10.1.1). Individuals with darker skin are at increased risk for adverse events such as hyperpigmentation and hypopigmentation with aggressive treatments.
they become white and atrophic.18 Treatment modalities including topical creams, microneedling, microdermabrasion, laser and light devices, and radiofrequency (RF) devices have been studied. Diet and exercise have not shown to improve SD.19 When choosing a therapy, one must consider the type and color of the striae as well as the patients’ Fitzpatrick skin type (FST) (Algorithm 10.1.1). Individuals with darker skin are at increased risk for adverse events such as hyperpigmentation and hypopigmentation with aggressive treatments.
Medical
The approach to treating striae often includes medical therapeutic options, although results from topical therapy are minimal (Algorithm 10.1.1).
Topical Therapy
Tretinoin. Tretinoin, a vitamin A derivative, has been reported to clinically improve the appearance of early active striae; however, it did not appear to have a significant effect on mature striae alba. Kang et al had 10 patients apply 0.1% tretinoin daily and 12 patients apply a placebo daily for 6 months. The striae in the patients treated with tretinoin decreased in mean length and width by 14% and 8% compared with an increase of 10% and 24% in the placebo group.20 Another study examined the role of tretinoin cream in SG. Twenty postpartum women were treated with 0.1% tretinoin cream daily for 3 months. The treated stretch marks decreased in length by 20%.21 It is important to remember that topical tretinoin should not be used in pregnant or breast-feeding women owing to possible teratogenic effects.22
Emollient Creams. The use of various hydrant creams to prevent stretch marks in pregnant woman is commonplace; however, efficacy has never been proven. Creams and ointments are being used by up to 78% of pregnant woman.5 In 2012 a Cochrane review assessed the efficacy of 6 topical agents in studies involving over 800 women.25 The preparations they studied included Alphastria, Trofolastin, Verum, olive oil, and cocoa butter. They found no statistically significant average difference in the development of SD in women who received these topical agents compared with placebo and did not find evidence to support the use of topical agents for the prevention of stretch marks during pregnancy.25
Topical Plant Extracts and Antioxidant Creams. Although more scientific evidence is needed to support their efficacy, a number of topical cosmetic products have been marketed for striae; those with some scientific evidence for their use are discussed herein. Trofolastin cream contains Centella asiatica extract, vitamin E, and collagen-elastin hydrolysates. C asiatica is believed to stimulate fibroblast activity and have an antagonistic effect on glucocorticoids.26 Mallol et al applied Trofolastin or placebo to the abdomen, breast, and buttocks of 80 pregnant woman. They reported that 22% fewer women developed stretch marks in the Trofolastin group compared with the placebo group.27 However, concerns for attrition and randomization bias have questioned the results of this study. Alphastria cream is composed of hyaluronic acid, which is thought to stimulate collagen production, along with allantoin, vitamin A, vitamin E, and dexpanthenol.3 A randomized controlled study reported that 10% of treated women compared with 70% of women in the control group developed SD.28 Randomized control studies investigating cocoa butter, which is commonly marketed for the prevention of SD, have failed to show any significant difference between cocoa butter and placebo.29,30 Many studies examining the effect of topical agents for the treatment and prevention of SD are poorly designed, and true efficacy is difficult to determine. One must also consider the potential effect of massage on SD, as there is anecdotal evidence to suggest that massage may improve the appearance of scars.31
Cosmetic
Chemical Peels
Glycolic Acid. Glycolic acid is an alpha hydroxy acid that is believed to stimulate collagen synthesis by fibroblasts.23 Mazzarello et al performed a double-blind controlled study using 70% glycolic acid on thigh striae in 40 patients. Group A applied 70% glycolic acid to the SR on their left thigh and a placebo to the striae on the right thigh. Group B applied 70% glycolic acid to the SA on their left thigh and a placebo to the striae on the right thigh. They reported a significant decrease in furrow width but not resolution in both the SR and SA groups treated with glycolic acid.24 Details on randomization and blinding in this study were not clearly defined.
Microneedling
Microneedling is a technique that uses tiny needles to penetrate the skin and produce dermal injury that generates dermal collagen and elastin. Microneedling is a safe therapy in all skin types currently being used for the treatment acne scars and fine lines.32 Park et al treated 16 patients with SD 3 times: 7 patients were noted to have excellent improvement, and the remaining 9 were noted to have minimal to moderate improvement. Posttreatment biopsies demonstrated thickened epidermis and increased collagen and elastic fibers.33 A more
recent study compared microneedling with the CO2 fractional laser.34 Of 10 needle-treated patients 9 (90%) showed improvement, whereas only 5 of 10 (50%) of the CO2 laser-treated patients had improvement.
recent study compared microneedling with the CO2 fractional laser.34 Of 10 needle-treated patients 9 (90%) showed improvement, whereas only 5 of 10 (50%) of the CO2 laser-treated patients had improvement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree