Standard Choledochocholedochostomy
Susan C. Pitt
Christopher D. Anderson
DEFINITION
Choledochocholedochostomy is the primary anastomosis of the recipient common bile duct to the donor common bile duct. This is the most common method of biliary reconstruction following whole organ liver transplantation.
PATIENT HISTORY AND PHYSICAL FINDINGS
The biliary anastomosis is the last step in a liver transplant operation. Before performing the biliary anastomosis, the allograft should be reperfused, the recipient stable, and any coagulopathy should be resolving.
If the patient remains unstable or the coagulopathy persists and bleeding continues, delay the biliary anastomosis and pack the abdomen with laparotomy packs. Reoperation following biliary reconstruction is tenuous; there is significant risk of avulsing the biliary reconstruction.
The decision to perform a choledochocholedochostomy is made based on factors such as the recipient’s diagnosis as well as the size and quality of the bile ducts. Recipients with biliary tract disease (e.g., primary sclerosing cholangitis) should be reconstructed with a choledochojejunostomy. Before performing the anastomosis, examine both the recipient and the donor bile ducts to ensure that the ends are healthy and well perfused. The size and quality of the bile duct, as well as surgeon preference, determine whether a running or interrupted anastomosis is performed. Small or size-mismatched bile ducts can sometimes be performed more easily in an interrupted fashion.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The majority of patients undergo either a liver ultrasound with a duplex, a computed tomography (CT) scan, or a magnetic resonance imaging (MRI) of the liver prior to being listed for liver transplantation. Such standard pretransplant imaging of the recipient should be reviewed prior to the operation to ensure the absence of pathology (stricture, etc.) in the distal recipient bile duct. It would be unusual to require intraoperative imaging, but access to fluoroscopy and the ability to perform an intraoperative cholangiogram should be available.
TECHNIQUES
PREPARATION OF RECIPIENT AND DONOR BILE DUCTS
Examine the recipient and donor bile ducts and assess for size match, ischemia, and lack of stricture in the recipient distal common bile duct. If reconstruction would result in an inappropriate amount of tension on the anastomosis, a choledochojejunostomy should be considered.
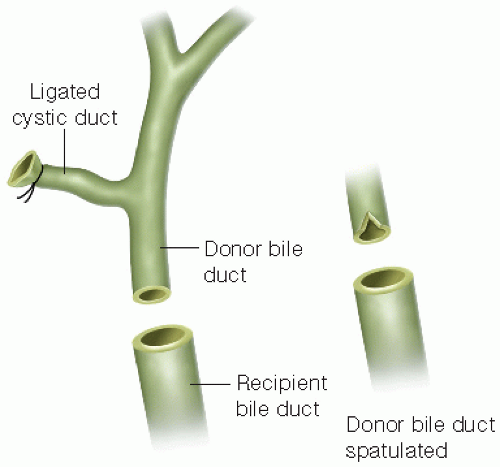
If a size mismatch is notable, the smaller bile duct can be spatulated to facilitate an easier anastomosis with a better match (FIG 1).
If one of the bile ducts appears ischemic, cut it back to healthy tissue using a sharp scissor. Stop bleeding from the bile duct with a fine absorbable monofilament suture (usually 5-0 or 6-0). Take care using cautery; do not damage the bile duct or surrounding structures.
Confirm that the distal recipient bile duct is patent with either a biliary probe or an appropriately sized pediatric feeding tube (8 Fr).
SETTING UP THE ANASTOMOSIS
The biliary anastomosis can be performed in an interrupted or a running fashion. There is no difference in biliary complications between the techniques.1 Use fine (5-0 or 6-0) absorbable monofilament sutures such as PDS (polydioxanone, Ethicon, Somerville, NJ) or Maxon (polyglyconate, Covidien, Mansfield, MA) for either technique.
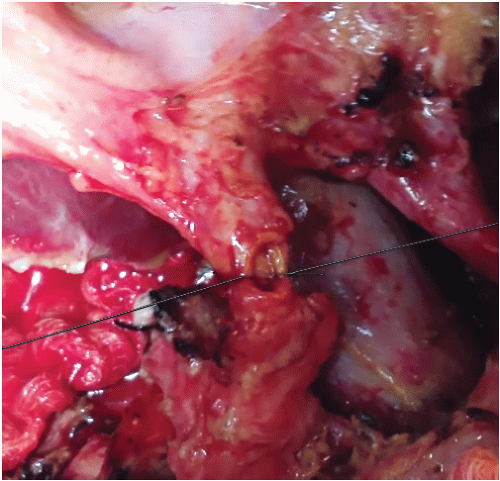
Both the running and the interrupted techniques begin in the same manner. Once the bile ducts are
prepared, place two fine absorbable monofilament sutures posteriorly in the 6 o’clock position to set up the choledochocholedochostomy (FIG 2A,B). Do not tie either suture to allow for complete visualization of both the recipient and donor bile ducts.
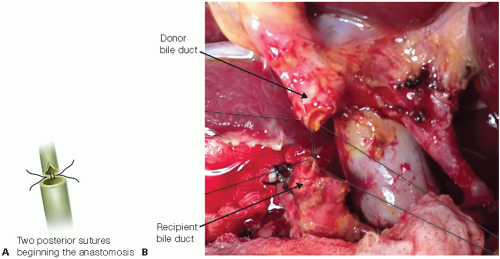
FIG 2 • A,B. Following spatulation, the posterior (6 o’clock position) corner is secured with two fine monofilament sutures.
Place sutures at least 1 to 2 mm from the cut edge of each duct into the mucosa to ensure that the stitches do not pull through. Take care not to twist or torque the bile ducts, assuring that they align properly.
Tie down the sutures with at least six knots while keeping the opposite suture under tension. Loosen retractors on the donor liver or recipient bowel to allow the two ducts to come together without tension. Examine the vascular anastomoses to ensure that no kinking or twisting has occurred with the repositioning of the transplanted liver.
Interrupted Anastomosis
To perform an interrupted anastomosis, place fine absorbable monofilament sutures from the posterior 6 o’clock position circumferentially around each side to reach 12 o’clock position.
Place one or two sutures and tie and cut them as one progresses from posterior to anterior. If you tie and cut all of the sutures at the end, they frequently become tangled. Two surgeons can sew the lateral sides of the bile duct at the same time placing the sutures 1 to 2 mm apart. Too many sutures may play a part in causing ischemia and late strictures.
When the anastomosis is approximately 75% complete, stop tying the sutures so that the lumen of the duct can still be visualized. Then place the final few sutures, do not tie them, and secure them on rubber shod (FIG 3). Visualizing the interior of the duct helps to avoid “back-walling” the anastomosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree