Left Lateral Segment Living Donor Hepatectomy
Anand Ghanekar
DEFINITION
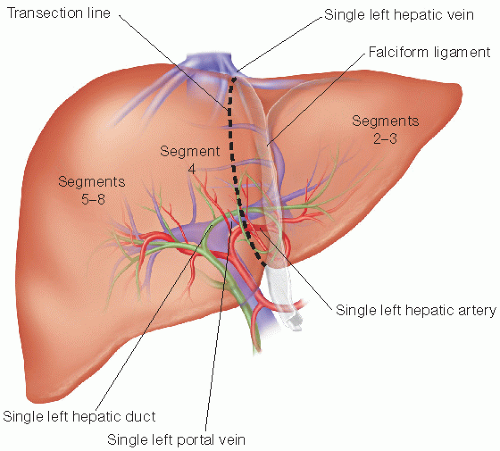
Left lateral segment living donor hepatectomy is a resection of the left lateral segment of the liver from a healthy individual for the purpose of transplantation into an individual in need of a liver transplant. The resection includes segments 2 and 3 of the liver in their entirety, with the liver parenchyma being transected through segment 4 to the right of the falciform ligament. The arterial, venous, and biliary anatomy of the left lateral segment must be confirmed by preoperative imaging and carefully preserved during the procedure until the mobilization is completed, after which the vessels can be divided and the graft flushed with preservation solution for subsequent transplantation in the recipient.
PATIENT HISTORY AND PHYSICAL FINDINGS
Donor safety is the highest priority of transplant centers offering living donation, and this principle must direct the donor assessment process.
A thorough history and complete physical examination must be performed, including attention to the points enumerated in the following text. This evaluation must be conducted by at least four individuals including a specialist in internal medicine, a hepatobiliary/transplant surgeon, a specialist in psychological medicine, and an independent medical consultant or donor advocate who has no affiliation with the transplant team.
The offer of liver donation must be completely voluntary without any evidence of external pressure, coercion, or expectation of material gain.
Left lateral segment liver donation is usually offered from an adult to a pediatric recipient. Donors must be old enough to provide informed consent (older than 18 years of age). For pediatric recipients, donors younger than 50 years of age are preferred.
Candidates for live liver donation must be in excellent physical and mental health in order to safely undergo major abdominal surgery, recover fully, and resume their normal activities. A history of cancer and/or active infection is a contraindication to organ donation.
A history of chronic liver disease is a contraindication to live liver donation. A strong family history of hereditary liver or gastrointestinal disease should be considered a relative contraindication to liver donation (e.g., primary sclerosing cholangitis, autoimmune hepatitis, primary biliary cirrhosis, inflammatory bowel disease).
Medical conditions that increase the perioperative risks of morbidity and mortality to the donor are relative contraindications to live donation, such as diabetes, hypertension, cardiac disease, respiratory disease, thromboembolic disease, renal dysfunction, obesity (body mass index [BMI] >35), and extensive previous abdominal surgery.
Smoking, oral contraceptive pills, and estrogen replacement therapy are risk factors for perioperative thromboembolic events and should be stopped for at least 4 weeks prior to donation and for 6 weeks after donation.
Alcohol consumption, even in small amounts, may affect tests of liver enzymes and liver function during the assessment phase and may impair liver regeneration after donation. Donors should abstain from alcohol consumption during the evaluation phase, for at least 4 weeks prior to donation and for at least 6 weeks after donation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Donors must undergo extensive laboratory evaluation and imaging in order to determine whether they are suitable candidates for live donor hepatectomy. Donors are not investigated until the recipient is deemed a suitable candidate to undergo living donor liver transplantation.
Laboratory evaluation includes the following:
Blood type determination—ABO compatibility with the recipient is usually confirmed prior to any further testing. ABO incompatible transplants may be performed with specific immunomodulatory protocols in place to minimize the risk of antibody-mediated rejection in the recipient.
Hematology—hemoglobin, leukocyte count, platelet count, international normalized ratio (INR), and activated partial thromboplastin time (aPTT)
If there is a personal or family history of thromboembolic disease, a thrombophilia workup should be performed in consultation with a hematologist and may include analyses of protein C, protein S, factor V Leiden, prothrombin genotype, antithrombin, and antiphospholipid antibodies.
Liver biochemistry—aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), bilirubin, albumin, protein
Abnormalities of liver enzymes or bilirubin must be further investigated with a liver biopsy (see in the following text) in consultation with a hepatologist. Mild hyperbilirubinemia due to Gilbert’s syndrome is the only acceptable cause of abnormal liver enzymes in a living donor.
In patients with a family history of hereditary liver disease or autoimmune disease, autoantibodies should be tested including antinuclear antibody, antismooth muscle antibody, and antimitochondrial antibody.
Endocrinology—fasting glucose, hemoglobin A1c, thyroid-stimulating hormone (TSH), free T3, free T4
Abnormalities of these results should be evaluated further by an endocrinologist.
Diabetes requiring medical therapy for blood sugar control is a contraindication to liver donation.
Individuals with benign etiologies of hyperthyroidism or hypothyroidism who are otherwise healthy may proceed with liver donation once thyroid function is normalized with appropriate management of the underlying condition.
Infectious disease—hepatitis C antibody, HIV antibody, human T-lymphotropic virus (HTLV) antibody, syphilis antibody, cytomegalovirus IgG, Epstein-Barr virus VCA IgG antibody, hepatitis B surface antigen, hepatitis B surface antibody, hepatitis B core antibody, West Nile virus
Evidence of hepatitis C, HIV, or HTLV contraindicates donation and requires further evaluation by a hepatologist (for hepatitis C virus [HCV]) or infectious diseases specialist.
Evidence of active hepatitis B (surface antigen positive) contraindicates donation and requires further management by a hepatologist. Hepatitis B surface antibody positivity due to immunization (surface antigen negative, core antibody negative) is not a contraindication to donation. Hepatitis B core antibody positivity (surface antigen negative) suggests prior exposure to hepatitis B and candidacy for donation should be further evaluated by liver biopsy and hepatitis B virus (HBV) DNA testing in consultation with a hepatologist if the recipient has immunity against hepatitis B and would be prepared to accept a liver graft from a donor with prior exposure to HBV.
Cardiac and respiratory testing—chest x-ray, pulmonary function tests, and electrocardiogram (ECG)
All donors older than 50 years of age or those younger than 50 years of age with abnormal ECG results or cardiac symptoms should be evaluated with exercise stress test and 2-D echocardiogram in consultation with a cardiologist.
Age-appropriate health screening tests should be up-to-date, including colonoscopy, mammogram, prostate-specific antigen, and Pap smear.
Liver imaging
Contrast-enhanced multiphasic high-resolution computed tomography (CT) scan of the liver is performed to delineate the anatomy and branching pattern of the hepatic artery, portal vein, and hepatic veins.
Contrast-enhanced magnetic resonance (MR) cholangiography is performed to delineate the anatomy of the biliary tree and to estimate the degree of fatty infiltration in the liver (using the in/out phase gradient echo T1 images).
For live liver donation, there should be no fat in the liver appreciable on magnetic resonance imaging (MRI). If fat is detected, then a liver biopsy must be performed (see in the following text) for further assessment.
Other abdominal organs and tissues should also be carefully assessed on these studies by the radiologist to exclude any pathology.
Volumetric analysis of the liver should be performed using the CT images and a suitable computer software package in order to estimate the total liver volume, graft volume, residual liver volume, and graft-to-recipient weight ratio (GRWR). The donor must be left with a minimum residual liver volume of 30% (rarely a concern when performing a left lateral segment resection). The GRWR should be a minimum of 1% but usually exceeds this substantially because the pediatric recipients of left lateral segment grafts are typically much smaller than adult donors.
Liver biopsy should be used to further evaluate the following and should be interpreted by a specialized hepatopathologist:
Fatty infiltration detected on imaging—Donation should not be permitted if steatosis exceeds 10% or if there is evidence of steatohepatitis, as this may impair liver regeneration in the donor and jeopardize graft function in the recipient. Fatty liver is often reversible with appropriate dietary modification and weight loss.
Abnormal liver enzymes or liver function tests—The liver parenchyma must appear completely normal in order to allow donation; the presence of fibrosis, cirrhosis, or inflammation is a contraindication to donation.
PREOPERATIVE PLANNING
It is preferable if segments 2 and 3 are supplied by a single hepatic artery branch (arising from the common hepatic artery, left hepatic artery, or left gastric artery) and a single portal vein branch (FIG 1). Grafts with more than one
artery pose a higher risk of hepatic artery thrombosis to the recipient but can be considered if the recipient size and anatomy will permit appropriate options for arterial reconstruction. Grafts with multiple portal vein branches can be considered if the recipient anatomy will provide satisfactory options for portal vein reconstruction (e.g., Y-graft using the recipient main portal vein bifurcation) but pose a higher risk of vascular complications in the recipient. A single left hepatic vein draining segments 2 and 3 is preferable. Multiple hepatic veins that exit the left lateral segment close to one another may be brought together for a single anastomosis in the recipient. Veins that are further apart pose limited options for reconstruction in a small pediatric recipient. A graft with one or two bile ducts draining segments 2 and 3 is also preferred in order to minimize the risk of biliary complications in the recipient.
Careful attention must be paid to the vascular and biliary structures that will supply the residual liver in the donor, in the context of the planned parenchymal transection through segment 4, approximately 1 cm to the right of the falciform ligament. Injuring structures supplying segments 5 through 8 of the liver should contraindicate left lateral segment donor hepatectomy. For example, in a liver with two separate right hepatic ducts, the posterior duct may drain into the left hepatic duct close to the point at which the left hepatic duct is normally divided during a left lateral segment donor hepatectomy.
It is important to note that during a left lateral segment donor hepatectomy, the arterial inflow, portal vein inflow, hepatic vein outflow, and biliary drainage of segment 4 can rarely be preserved. The need to sacrifice these structures is not a contraindication to left lateral segment donor hepatectomy. Similarly, the portal vein branches to the caudate lobe as well as the caudate bile duct are also sacrificed as a routine part of the procedure.
The donor should be thoroughly informed about the risks of surgery, noting that the risk of mortality is estimated at 0.15% and that up to 30% of patients experience one or more complications.
Donors should also be informed that live donation may impact on their future ability to qualify for health or life insurance coverage in some jurisdictions.
PATIENT POSITIONING AND PREPARATION
An operating room should be used that is large enough to accommodate a back table, C-arm for intraoperative cholangiography, intraoperative ultrasound machine, a red blood cell salvaging suction machine, and a hydrodissector (Hydrojet) or Cavitron ultrasonic surgical aspirator (CUSA) in addition to the usual operating room equipment. Peripheral and central venous access, arterial line, Foley catheter, TED stockings, and sequential compression devices should be placed, and the patient copiously padded to prevent pressure injuries. Prophylactic subcutaneous heparin and intravenous antibiotics should be administered.
TECHNIQUES
INCISION AND EXPOSURE
Use a Thompson retractor or other similar system to achieve uncompromised exposure during the procedure.
Make an upper midline incision extending from the xiphoid process down toward the umbilicus. Alternatively, use a right subcostal incision with vertical midline extension (FIG 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree