Transplant Nephrectomy
Michael J. Englesbe
Seth Waits
DEFINITION
Transplant nephrectomy is defined as excision or removal of previously transplanted kidney.
Transplant nephrectomy is a morbid operation and significant efforts should be made to avoid the procedure.
Transplant nephrectomy is indicated following early graft loss or late graft loss that is associated with significant complications.
DIFFERENTIAL DIAGNOSIS
Graft loss within 6 weeks of the transplant operation is an indication for transplant nephrectomy. This graft loss is usually associated with allograft thrombosis or profound acute rejection.
The majority of patients with a late graft failure do not require nephrectomy. The most common indication for transplant nephrectomy is pain over a nonfunctioning allograft.
Significant efforts to medically manage this pain with pulses of steroids or a temporary increase in immunosuppression medications are warranted.
Other indications for transplant nephrectomy include transplant mycotic aneurysm, uncontrolled hypertension, persistent hematuria related to the nonfunctioning graft, severe and life-threatening infection, or urologic complications of the transplant.
Transplant nephrectomy is done at the same time as a transplant operation in patients with multiple previous renal transplants.
Transplant recipients that develop a life-threatening malignancy may undergo a transplant nephrectomy to facilitate cessation of immunosuppression medications.
PATIENT HISTORY AND PHYSICAL FINDINGS
Careful consideration of alternatives to transplant nephrectomy should be considered. Make sure that a management plan is developed in collaboration with the patient’s transplant nephrologist.
Do an abdominal examination assessing for hernia over the transplant incision. Assess for graft tenderness.
Do a vascular examination, assessing for lower extremity pulses.
If transplant nephrectomy will result in the resumption of dialysis for the patient, consider a simultaneous dialysis access procedure.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Renal transplant ultrasound is mandatory prior to transplant nephrectomy. This study will assess flow into the allograft. Further, this study will determine vascular abnormalities in hilum of the kidney on recipient native vessels.
Perianastomotic aneurysms will significantly complicate the surgical dissection and need to be diagnosed prior to surgery.
Cross-sectional imaging will also delineate vascular anatomy. In patients with complex abdominal wall defects, this imaging will help plan the surgical incision and wound closure.
SURGICAL MANAGEMENT
Preoperative Planning
Careful perioperative planning and communication with the operative team is critical for an optimal outcome.
Administer prophylactic antibiotics to cover skin flora prior to the surgical incision. Administer prophylaxis for deep venous thrombosis.
Transfusions can complicate future transplantation. Nonetheless, transfusion is frequently required during the operation. Have two units of packed red blood cells available for routine cases and more blood products for cases involving complex vascular issues.
Place a three-way Foley catheter to enable instillation of Betadine or saline into the bladder during the operation to assist with identification of the bladder, if necessary.
TECHNIQUES
SURGICAL EXPOSURE
Make an incision over the previous renal transplant incision (FIG 1).
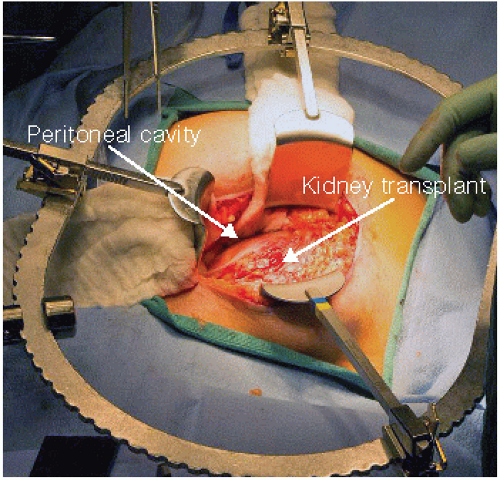
Using electrocautery, continue the dissection down to the capsule of the kidney. Ideally, the entire dissection will occur in an extraperitoneal plane, but frequently, the peritoneal cavity is entered with this dissection (FIG 2). Take care not to injure any bowel.
Place a self-retaining retractor.
LIGATION OF THE TRANSPLANT URETER
Dissect into the pelvis toward the bladder.
If a three-way Foley has been inserted, identification of the bladder can be aided with instillation of Betadine or saline into the bladder to distend it.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree